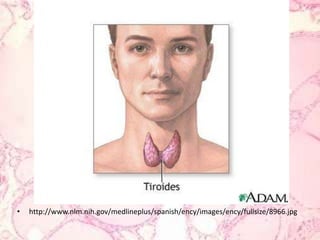
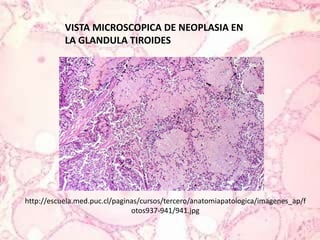
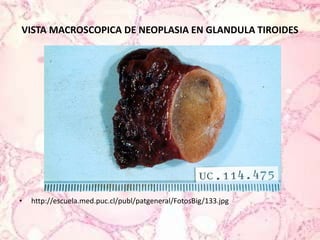
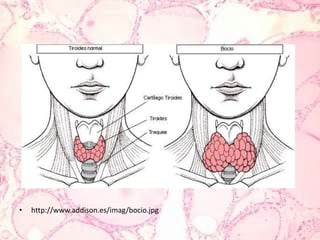
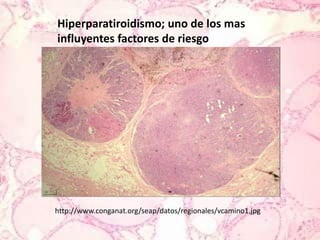
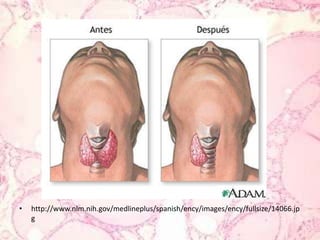
The document discusses medullary carcinoma of the thyroid gland. It begins with an overview of thyroid anatomy and the characteristics of medullary thyroid carcinoma, which originates from C cells that produce calcitonin hormone. The document then examines the causes, types, risk factors, signs and symptoms, diagnostic tests, treatment options including surgery, radiotherapy and chemotherapy, and prognosis for medullary thyroid carcinoma. It also references several medical studies and articles on topics such as variants of medullary thyroid carcinoma and detection of metastases.



![“Current role of metaiodobenzylguanidine in the diagnosis of pheochromocytoma and medullary thyroid cancer.Ilias I, Divgi C, Pacak K.SourceDepartment of Endocrinology, E. Venizelou Hospital, Athens, Greece.AbstractDespite early reports of excellent diagnostic characteristics of [(131)I]/[(123)I]-metaiodobenzylguanidine (MIBG) in the evaluation of pheochromocytomas/paragangliomas (PHEOs/PGLs) or medullarythyroid cancer as experience with it was accumulated, the sensitivity dropped. Nevertheless, this modality is still useful in the diagnostic work-up of PHEOs/PGLs because it is widely available, and in case of positive scans it might indicate patients who are potential candidates for [(131)I]MIBG therapy.Published by Elsevier Inc.”12](https://image.slidesharecdn.com/carcinomamedulardetiroides-110802205142-phpapp02/85/Carcinoma-medular-de-tiroides-24-320.jpg)

![3)Goldman JM, Goren EN, Cohen MH, et al.: Anaplasticthyroid carcinoma: long-termsurvivalafter radical surgery. J SurgOncol 14 (4): 389-94, 1980. [PUBMED Abstract]4)Aldinger KA, Samaan NA, Ibanez M, et al.: Anaplastic carcinoma of thethyroid: a review of 84 cases of spindle and giantcell carcinoma of thethyroid. Cancer 41 (6): 2267-75, 1978. [PUBMED Abstract]5)Carling T, Udelsman R: Thyroidtumors. In: DeVita VT Jr, Hellman S, Rosenberg SA, eds.: Cancer: Principles and Practice of Oncology. Vols. 1 & 2. 8th ed. Philadelphia, Pa: Lippincott Williams & Wilkins, 2008, pp 1663-82.](https://image.slidesharecdn.com/carcinomamedulardetiroides-110802205142-phpapp02/85/Carcinoma-medular-de-tiroides-33-320.jpg)
![6)Shimaoka K, Schoenfeld DA, DeWys WD, et al.: A randomized trial of doxorubicin versus doxorubicin plus cisplatin in patientswithadvancedthyroid carcinoma. Cancer 56 (9): 2155-60, 1985. [PUBMED Abstract]7)Haigh PI, Ituarte PH, Wu HS, et al.: Completelyresectedanaplasticthyroid carcinoma combinedwithadjuvantchemotherapy and irradiationisassociatedwithprolongedsurvival. Cancer 91 (12): 2335-42, 2001. [PUBMED Abstract]8)De Crevoisier R, Baudin E, Bachelot A, et al.: Combinedtreatment of anaplasticthyroid carcinoma withsurgery, chemotherapy, and hyperfractionatedacceleratedexternalradiotherapy. Int J RadiatOncolBiolPhys 60 (4): 1137-43, 2004. [PUBMED Abstract]](https://image.slidesharecdn.com/carcinomamedulardetiroides-110802205142-phpapp02/85/Carcinoma-medular-de-tiroides-34-320.jpg)