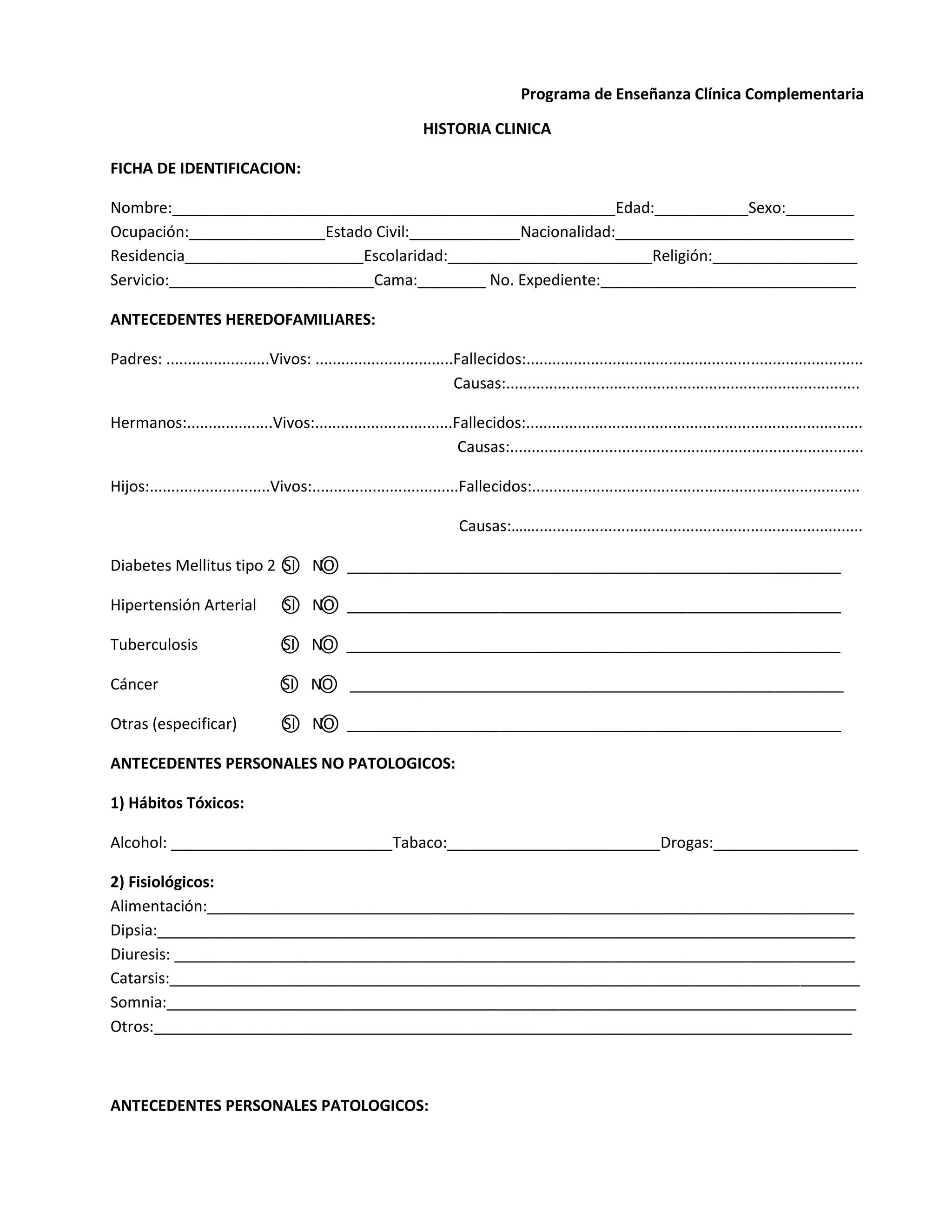
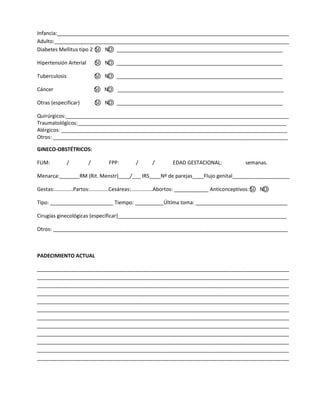
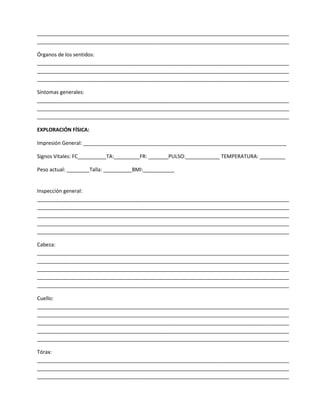
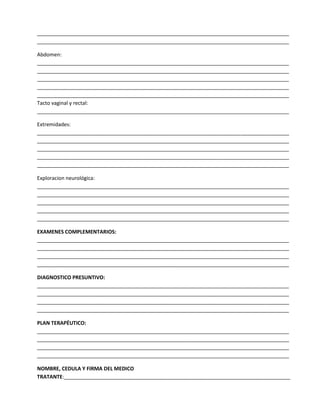
This document contains a clinical history form for a patient, collecting information about their family medical history, personal medical history, current complaints, and physical exam findings. Sections include ancestry, habits, gynecological history, review of symptoms by body system, and vital signs. The physical exam section documents the general impression and assessments of head, neck, and other body areas.