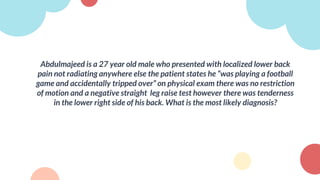
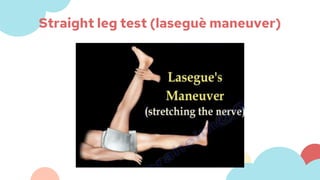
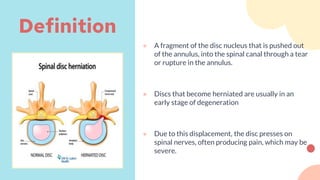
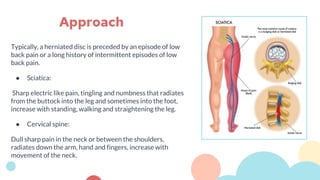
Abdulmajeed, a 27-year-old male, presented with lower back pain after tripping during a football game. On examination, he had tenderness but no restriction of motion or positive straight leg raise. The most likely diagnosis is muscle strain or sprain, which are common causes of low back pain from sudden injury or overuse. Differential diagnoses include lumbar spine disorders like herniated disc or compression fracture. Conservative treatment includes rest, ice/heat, over-the-counter pain medication, and physical therapy exercises.






![Systemic disorders:
● Primary or metastatic neoplasms
● Osseous, diskal, or epidural infections
● Inflammatory spondyloarthropathy
● Metabolic bone diseases, including osteoporosis
● Vascular disorders (eg, atherosclerosis, vasculitis)
Referred pain:
● Gastrointestinal disorders (eg, pancreatitis, pancreatic cancer, cholecystitis)
● Cardiorespiratory disorders (eg, pericarditis, pleuritis, pneumonia)
● Disorders of the ribs or sternum
● Genitourinary disorders (eg, nephrolithiasis, prostatitis, pyelonephritis)
● Thoracic or abdominal aortic aneurysms
● Hip disorders (eg, injury, inflammation, or end-stage degeneration of the joint and associated
soft tissues [tendons, bursae, ligaments])
Systemic causes of back pain:](https://image.slidesharecdn.com/backpaintutorial-240320133420-c8323531/85/Back-Pain-Tutorial-pptx-approach-to-back-pain-58-320.jpg)