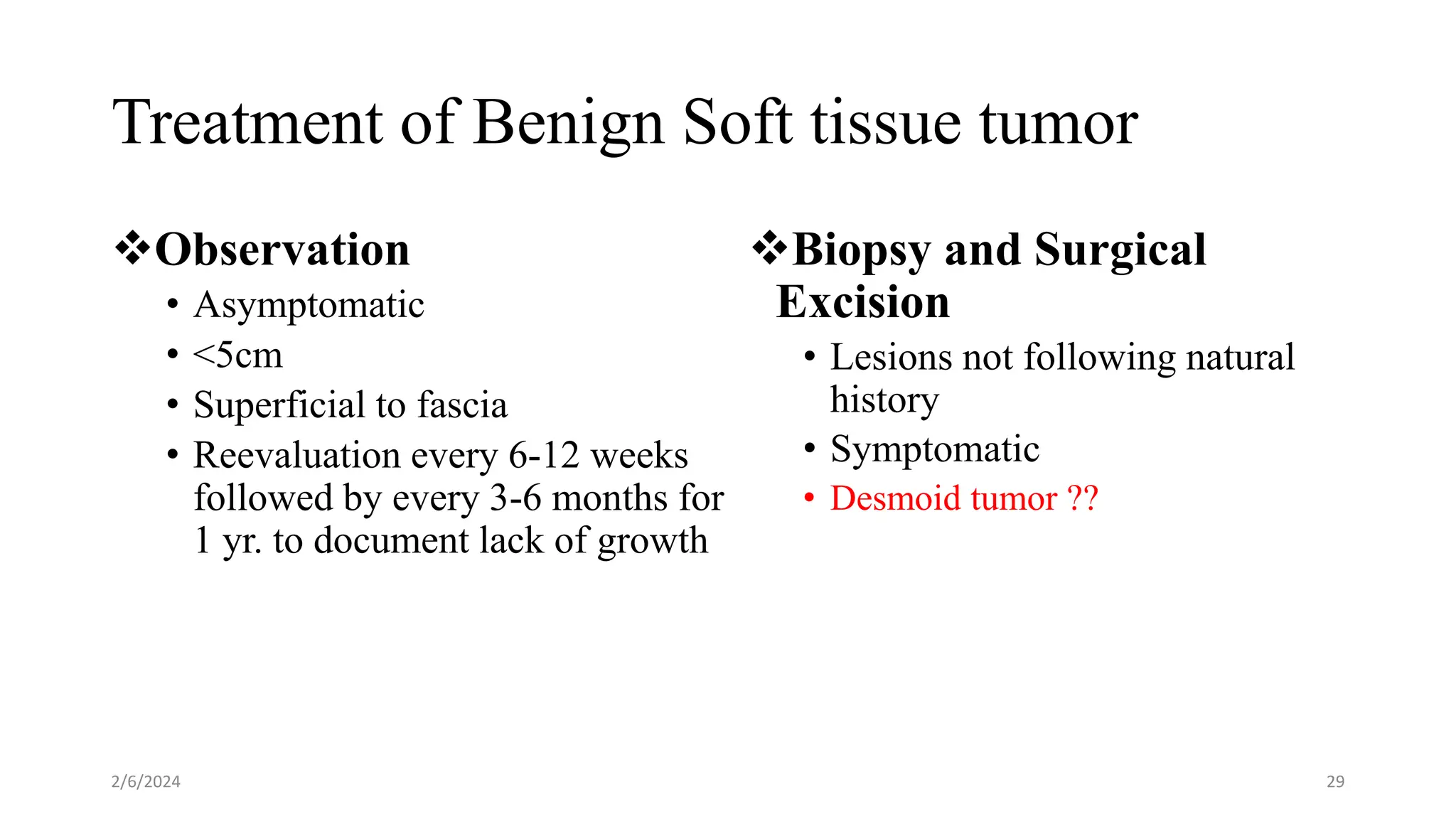
This document provides an overview of soft tissue tumors, including their epidemiology, diagnostic evaluation, classification, treatment principles, and some common types. Soft tissue tumors can be benign or malignant, with malignant soft tissue sarcomas making up about 1% of adult cancers. Diagnostic evaluation involves history, imaging such as MRI or CT, and biopsy. Treatment depends on whether the tumor is benign or malignant, with malignant soft tissue sarcomas typically requiring a multidisciplinary approach involving surgery, radiation, and chemotherapy.