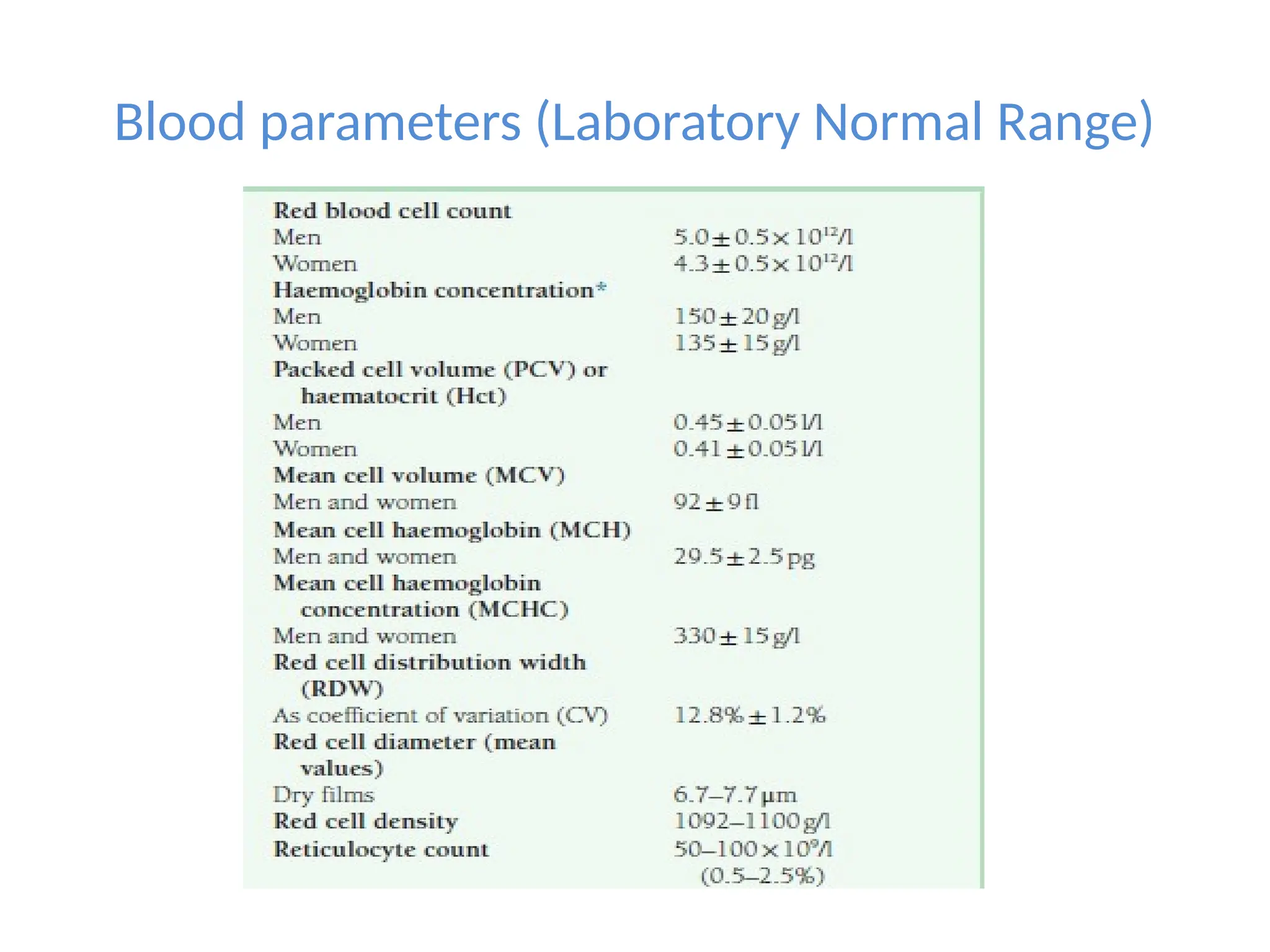
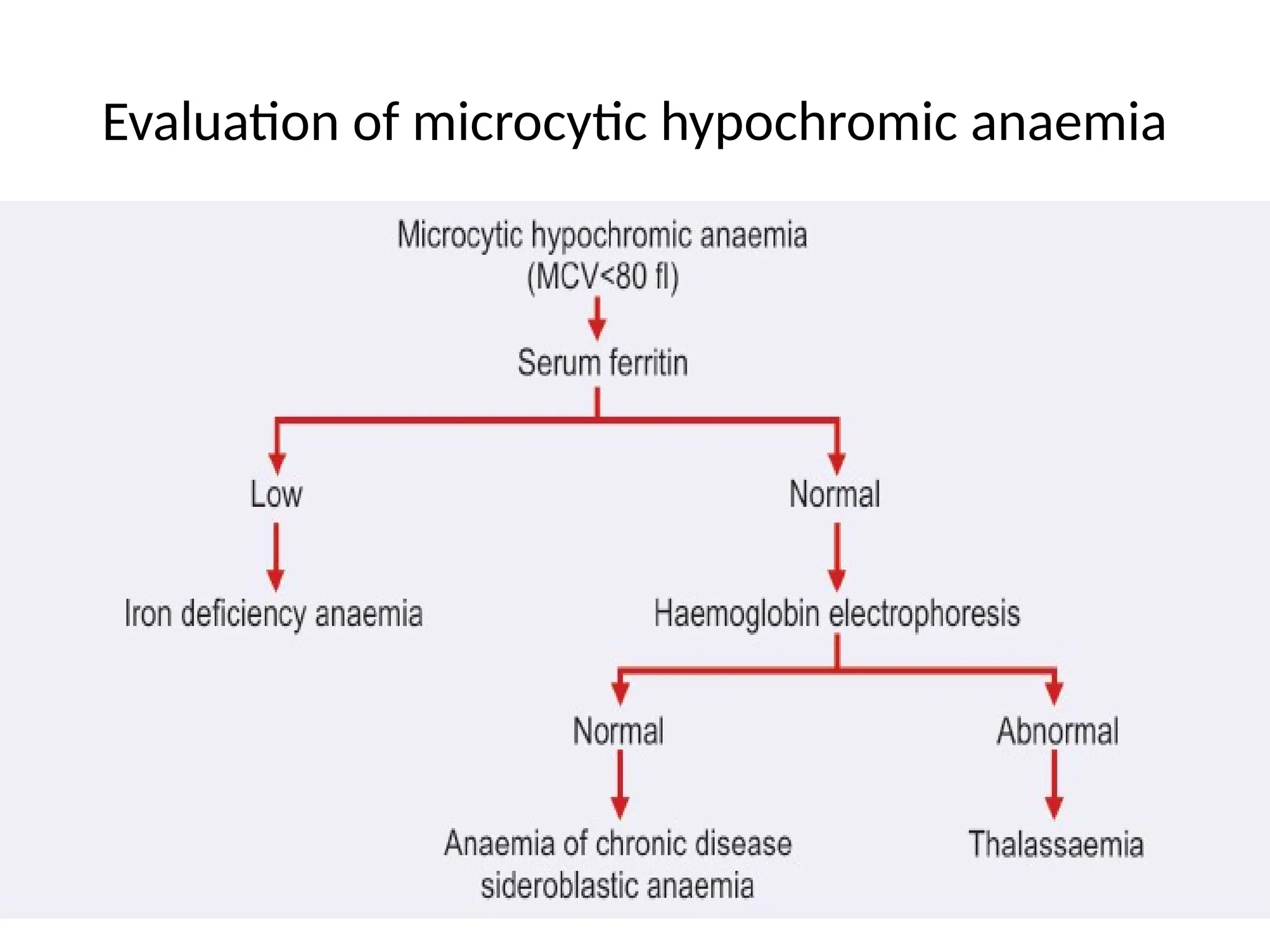
The document provides a comprehensive overview of anemia, detailing its clinical presentation, definition, diagnosis approach, classification, and distinct features of various types such as microcytic hypochromic, macrocytic, and normocytic anemia. It outlines laboratory parameters, grading, and the importance of reticulocyte counts in the diagnosis of different anemias, including conditions like iron deficiency and megaloblastic anemia. The document also covers hemolytic anemias, their causes, and relevant tests, culminating in a summary of key anemia classifications.