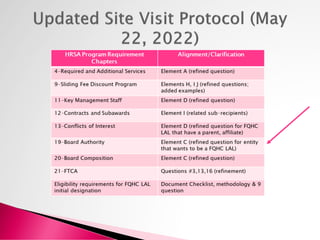
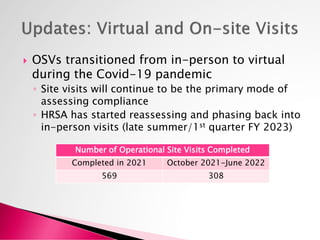
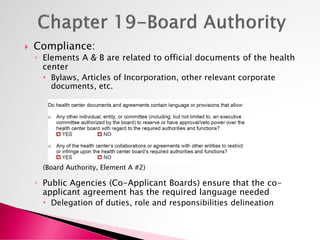
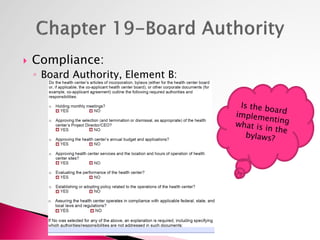
The document outlines a webinar series focused on continuous compliance for health centers, emphasizing the importance of understanding site visit protocols and requirements for achieving excellence. It discusses various compliance elements, strategic planning, and methods to assess service utilization and patient satisfaction. The presentation also highlights the transition from in-person to virtual operational site visits due to the COVID-19 pandemic and ongoing governance requirements for health center boards.