13 april 2011 child health in sa
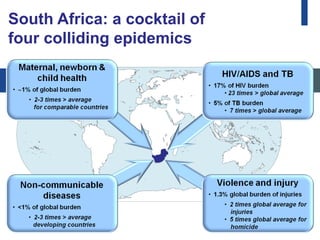
- 1. South Africa: a cocktail of four colliding epidemics
- 2. South Africa: coping with a very high burden of disease Percentage of total 22% 9% 6% 4% 4% 4% 3% 3% 3% 2% 2% 2% 2% 2% 2% 2% 1% Population: 45 M Figure 2: National burden of disease Data sourced from WHO Global Burden of Disease (2002). DALYs=disability-adjusted life years. DR Congo=Democratic Republic of the Congo. DTP=diphtheria, tetanus, and pertussis. *Low birthweight, birth asphyxia, and birth trauma.
- 3. South Africa: coping with a very high burden of disease Percentage of total 22% 9% 6% 4% 4% 4% 3% Population: 153 M 3% Population: 48 M 3% 2% 2% 2% 2% 2% 2% 2% 1% Population: 45 M Figure 2: National burden of disease Data sourced from WHO Global Burden of Disease (2002). DALYs=disability-adjusted life years. DR Congo=Democratic Republic of the Congo. DTP=diphtheria, tetanus, and pertussis. *Low birthweight, birth asphyxia, and birth trauma.
- 4. South Africa: coping with a very high burden of disease Percentage of total 22% 9% 6% 4% 4% 4% 3% 3% Population: 48 M 3% 2% 2% 2% 2% 2% 2% 2% 1% Population: 45 M Population: 45 M Figure 2: National burden of disease Data sourced from WHO Global Burden of Disease (2002). DALYs=disability-adjusted life years. DR Congo=Democratic Republic of the Congo. DTP=diphtheria, tetanus, and pertussis. *Low birthweight, birth asphyxia, and birth trauma.
- 5. Assessment of S. Africa’s progress on 6 MDGs MDG Progress in South Africa On track? 1. Eradicate extreme Underweight children < 5 years:12% Target ≤5% Reversal of progress poverty & hunger Mean reduction per year: –6% Target 2-6% 1. Achieve universal Enrolment in primary school: 87% Target 90% Insufficient progress primary education 1. Promote gender Gender parity ratio: 1·0 Target 1·0 On track equality & empower women 1. Reduce mortality of <5 mortality 1995-2005 - increasing Target -66% Reversal of progress children <5 years 1. Improve maternal Maternal mortality 1995-2005 – no Target -75% No progress health reduction 1. Combat AIDS, HIV prev 1995-2005 - increasing Target -50% Insufficient progress malaria, etc
- 6. Potential for significant impact
- 7. A lack of health improvement despite major investments The paradox is poor health outcomes despite good policies and relatively high health expenditure 5 main areas where contradictions help explain the discordance between high investments and poor outcomes
- 8. Avoidable Causes of Deaths • Clinical Care: poor quality • Administrative Management: shortcomings • Community: avoidable factors-awareness and demand
- 9. Family and Managers and Healthcare Community policy makers providers 44% of maternal deaths 32% of maternal deaths 54% of maternal deaths had a had a modifiable factor had a modifiable factor modifiable factor related to related to related to administrator healthcare provider action at family/community action, action, e.g. lack of blood primary level; 48% at secondary e.g. Inadequate or no for transfusion, lack of level; and 37% at tertiary level antenatal care transport between health e.g. not adhering to standard institutions protocols 38% of stillbirths and 19% of stillbirths and early 35% of stillbirths and early early neonatal deaths had neonatal deaths had a neonatal deaths had a modifiable a modifiable factor related modifiable factor related to factor related to healthcare to family/community administrator action, e.g. provider action, e.g. fetal distress action, e.g. delay in personnel not available or not identified in labour, poor seeking care during not sufficiently trained response to maternal labour hypertension 25% of all modifiable 22% of all modifiable 53% of all modifiable factors in factors in child deaths factors in child deaths were child deaths were related to were related to related to administrator healthcare provider action, e.g. family/community action, action, e.g. lack of senior IMCI not used in clinics, and poor e.g. caregiver did not doctors and nurses, and assessment and management in recognise severity of the insufficient paedaitric beds hospitals illness
- 10. SPECIALIST OBSTETRIC AND GYNAECOLOGICAL SPECIALIST NEONATAL AND PAEDIATRIC CARE Regional hospital CARE Connecting places of caregiving REPRODUCTIVE EMERGENCY PREGNANCY AND EMERGENCY NEWBORN AND CHILD CARE CARE CHILDBIRTH CARE Care for sick children including those with HIV&AIDS, based hospital District Termination of pregnancy Care for high risk pregnancies and Post-abortion care on Integrated Management of Childhood Illness principles Treatment of complicated immediate newborn care including Extra care of preterm babies including kangaroo mother care sexually transmitted resuscitation Emergency care for sick newborns infections REPRODUCTIVE ANTENATAL BASIC CHILDBIRTH POSTNATAL CARE CHILD CARE HEALTH CARE CARE CARE •Early detection & Immunisations •Family planning Basic antenatal Care for normal referral of complications Growth monitoring and Outpatient and •Prevention and care care package with deliveries and immediate nutrition maternity unit •Support for infant of sexually prevention of HIV newborn care including feeding choices Integrated Management of transmitted infections mother-to child resuscitation •HIV testing for infants at Childhood Illness integrated and HIV&AIDS transmission and prevention of mother- with care of children with HIV 6 weeks •Preconception folic care for women to child transmission of including cotrimoxazole acid HIV •Adolescent and pre- •Healthy behaviours eg maternal nutrition, •Appropriate home care of babies: appropriate feeding, avoiding pregnancy nutrition reduced work load hypothermia, hygienic cord/skin care, extra care for preterm babies •Prevention of HIV •Danger sign recognition, and emergency •Good nutrition, including complementary feeding •Demand for key preventive services such as immunisations community and sexually preparedness Family and transmitted infections •Recognition of danger signs and appropriate care-seeking Intersectoral Improved living conditions – housing , water and sanitation, nutrition Education and empowerment Pre-pregnancy Pregnancy Birth Postnatal Childhood
- 11. Need to address key structural and health systems bottlenecks Improving capacity and stewardship of health system to institute fundamental changes such as: improving levels of morale and commitment amongst health workers; scaling up of mid-level workers; task-shifting; standardization, expansion and strengthening of community health worker programmes; and re-orientation of pre-service training, accelerated production of such graduates and enhancing capacity of public health managers.
- 12. Violence and injuries Distribution of injury mortality by cause, 2000 (A) Worldwide. (B) South Africa.
- 13. Examples of innovation in the system Examples of innovation Maternal, • Audits of deaths of mothers and children26; Newborn and • Twinning of hospitals and clinics; Child Health • On-site mentoring within health system27; • Development of ‘mothers to mothers’ support groups28; • Use of participatory research to improve malnutrition management29 HIV/TB • Widespread implementation of lay counsellors and community workers30; • Universal use of rapid HIV test kits; • Shift towards nurse driven treatment and care; • Development and introduction of electronic clinical information systems31 • Outreach support for nurses in TB programmes32 Chronic disease • Development of simplified clinical protocols33; and mental health • Inclusion of adult health indicators in national health survey to monitor the prevention and control of chronic diseases and their risk factors34 • Outreach support from hospital to clinics Violence and • Development of Family Courts; injury • Establishment of peace committees; • Use of group interventions and micro-credit to reduce violence35 36; • Settings based approach (schools and cities) towards improving environmental determinants;
- 14. Key Messages – HIV/AIDS and poor implementation of existing packages of care are the main reasons for the lack of progress towards the MDGs on MNCH. – Full coverage of key packages of interventions would put South Africa on track to achieve MDG 4 and make substantial progress towards MDG 5.
- 15. Key messages High coverage of priority care for MNCH is financially feasible, requiring a 24% increase in expenditure. Strengthening of leadership, accountability mechanisms, and high quality of care interventions are required
- 16. 4 million newborns die annually within the first month of life, and their fate is intimately linked to their mothers’ health.
- 17. HIV AND MATERNALMORTALITY King Edward Vlll Hospital, Durban., South Africa Hypertension Other Causes (24%) (35%) AIDS Pre-existing Med (15%) Conditions Pregnancy-related Haemorrhage Sepsis (7%) Under-reporting of AIDS Deaths HIV Status unknown in 75.8%
- 18. Why do mothers die in South Africa? Other, 16% Non- pregnancy related infections Sepsis, 8% sucAIDS, TB, Pre-existing pneumonia, medical 38% disease, 6% Haemorrhag e, 13% Hypertensio n, 19% Source: Saving mothers report, DOH.
- 19. Why do newborns and children die in South Africa? Pneumonia, 1% Other child, 2% Injuries, 5% Diarrhoea, 1% Neonatal infections, 7% Preterm, 13% Neonatal HIV & Birth asphyxia, AIDS, 8% 35% Congential, 4% Other neonatal, 2% Source: UN estimates and South African data for 2008
- 20. WHY DO WHY DO AFRICAN NEWBORNS AND CHILDREN UNDER CHILDREN DIE IN THE AGE OF 5 SOUTH AFRICA? YEARS DIE? Pneumonia, 1% Other child, 2% Injuries, 5% Diarrhoea, 1% Neonatal infections, 7% Preterm, 13% Neonatal HIV & Birth asphyxia, AIDS, 8% 35% Congential, 4% Other neonatal, 2% Source: UN estimates and South African data for 2008
- 21. Number of Children on Comprehensive HIV and AIDS Treatment Plan Source of data: Monitoring and Evaluation, DoH, SA 21
- 23. Mortality trend in selected countries Brazil * 56 46 21 17 IMR U5MR 1990 2009 South Africa * 62 62 48 43 IMR U5MR 1990 2009 Source: : UN Inter-agency Group for Child Mortality Estimation,2010 23
- 24. WHY DO WHY DO AFRICAN MOTHERS DIE MOTHERS IN SOUTH DIE? AFRICA? Why do mothers die in South Africa? Other, 16% Other, 16% Non- pregnan related infectio Sepsis, 8% Sepsis, 8% Non- sucAID pregnancy TB, related infections Pre-existing pneumon sucAIDS, TB, pneumonia, medical Pre-existing medical disease, 6% 38% 38% disease, 6% Haemorrhag Haemorrhage, 13% e, 13% Hypertension, 19% Hypertensio n, 19% Source: Saving mothers report, Source: Khan KS et al. Lancet 2006 Source: Saving mothers report. DoH.
- 25. TOTAL MATERNAL POPULATION MORTALITY BURDEN SASI Group and M. Newman 2006
- 26. HIV/AIDS BURDEN Source: SASI Group and M. Newman 2006
- 27. MORTALITY: 1-4 YEAR OLDS
- 28. Family and HIV First steps to healing the South African Family. Lucy Holborn and Gail Eddy. SAIRR Fractured families: a crisis for South Africa “In South Africa, the “typical” child is raised by their mother in a single-parent household. Most children live in households with unemployed adults”
- 29. Orphans and child-headed households: There are 860 000 double-orphans in this country, 624 000 maternal orphans and 2 400 000 paternal orphans. More than half had lost parents due to AIDS. Single-parent households: 23% of children were living with neither biological parent; 35% were living with both biological parents. Absent fathers: Living but absent fathers 48% and present 36% in 2009.
- 31. Broken families breaking youth. Family breakdown impacts on: education, employment opportunities, teenage pregnancies, attitudes to sex, HIV, violence and crime, mental health
- 32. WHAT NEEDS TO BE DONE AT FAMILY LEVEL? NOW! 1. Support children through families 2. Develop comprehensive & integrated family-centered services 3. Create social protection for the poorest families 4. Expand income transfers to poor families Linda Richter. Mexico IAS Conference 2008
- 33. NOT ONLY ORPHANS ARE AFFECTED • AIDS Orphans ?? • Children infected and affected • Few differences between “orphans” and very poor children • A massive social problem <10% of children orphaned or made vulnerable by AIDS currently receive public support and services. UNAIDS . 2007 AIDS EPIDEMIC UPDATE
- 34. TREATMENT: WAYS FORWARD • Each infection can and should be prevented • Early diagnosis prior to disease progression • Earlier initiation of ART • Expand screening for HIV in health care facilities
- 35. TREATMENT: IMPROVING EFFECTIVENESS OF ARV THERAPY AMONG HIV-INFECTED CHILDREN IN SUB-SAHARAN AFRICA “..findings emphasise the need for: **low-cost diagnostic tests that allow for earlier identification of HIV infection in infants **improved access to antiretrovirals, including expansion into rural areas **integration of antiretroviral treatment programmes with other health-care services, such as nutritional support”. Sutcliffe et al, Lancet Infectious Diseases, 2008; 8:477-89
- 36. All children, including those affected by HIV and AIDS are best cared for in functional families with basic income security, access to health care and education, and support from kin and community Our work is to ensure these conditions for children and families
