most common causes of infectious vaginitis.pptx
- 1. LEUCORRHEA Dr. Ravali Kethineedi final year pg GEMS & H –SRIKAKULAM
- 3. BACTERIAL VAGINOSIS ◦ Also called nonspecific vaginitis or Gardnella vaginitis ◦ Alteration of normal vaginal bacterial flora that results in loss of lactobacilli and an overgrowth of predominantly anaerobic bacteria. ◦ Concentration of anaerobes and G. vaginalis and Mycoplasma hominis, is 100 to 1,000 times higher than in normal women. ◦ Lactobacilli are usually absent. ◦ repeated alkalinization of the vagina, which occurs with frequent sexual intercourse or use of douches, plays a role.
- 4. ◦ Increased risk ⁻ pelvic inflammatory disease (PID) ⁻ postabortal PID ⁻ postoperative cuff infections after hysterectomy ⁻ and abnormal cervical cytology ⁻ Pregnant women risk for premature rupture of the membranes, preterm labor and delivery, chorioamnionitis ⁻ postcesarean endometritis . In women with BV who are undergoing surgical abortion or hysterectomy, perioperative treatment with metronidazole eliminates this increased risk • Hydrogen peroxide–producing lactobacilli disappear, it is difficult to reestablish normal vaginal flora -recurrence of BV is common
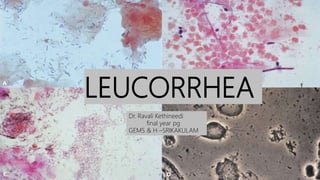
- 5. A) Normal mature vaginal cells with Döderlein’s lactobacilli. B) Clue cells with very few Döderlein’s bacilli.
- 6. DIAGNOSIS- ◦ A fishy vaginal odor, which is particularly noticeable following coitus ◦ vaginal discharge- gray and thinly coat the vaginal walls. ◦ The pH of these secretions is >4.5 (usually 4.7 to 5.7). ◦ Microscopy of the vaginal secretions reveals an increased number of clue cells. • the “whiff” test -releases a fishy, amine like odor- +
- 7. ◦ Clinicians who are unable to perform microscopy should use alternative diagnostic tests such as a -pH -amines test card -detection of G. vaginalis ribosomal RNA -Gram stain . ◦ Culture of G. vaginalis is not recommended as a diagnostic tool because of its lack of specificity.
- 8. Bacterial vaginosis. (A) Vaginal smear showing Döderlein’s bacilli. (B) Clue cells suggestive of bacterial vaginosis
- 9. ◦ Amsel et al. established clinical criteria for diagnosing BV.
- 10. ◦ Nugent et al. described a Gram stain scoring system of vaginal smears to diagnose BV
- 12. ◦ Ideally, treatment of BV should inhibit anaerobes but not vaginal lactobacilli. ◦ METRONIDAZOLE- ◦ Excellent activity against anaerobes but poor activity against lactobacilli, is the drug of choice for the treatment of BV. ◦ Avoid using alcohol during treatment with oral metronidazole and for 24 hours ◦ A dose of 500 mg administered orally twice a day for 7 days should be used. ◦ Metronidazole gel, 0.75%, one applicator (5 g) intravaginally once daily for 5 days, may also be prescribed.
- 13. ◦ CLINDAMYCIN ◦ Clindamycin ovules, 100 mg, intravaginally once at bedtime for 3 days ◦ Clindamycin bio adhesive cream, 2%, 100 mg intravaginally in a single dose Clindamycin cream, 2%, one applicator full (5 g) intravaginally at bedtime for 7 days ◦ Clindamycin, 300 mg, orally twice daily for 7 days ◦ Many clinicians prefer intravaginal treatment to avoid systemic side effects ( GI upset , unpleasant tasete) ◦ Treatment of the male sexual partner is not recommended
- 14. TRICHOMONAS VAGINITIS ◦ Caused by -sexually transmitted -flagellated parasite. ◦ The transmission rate is high (70% of men contract the disease after a single exposure to an infected woman.) ◦ It is a anaerobe that has the ability to generate hydrogen to combine with oxygen to create an anaerobic environment. ◦ It often accompanies BV,
- 16. ◦ Diagnosis – Trichomonas vaginitis is associated with a -profuse, purulent, malodorous vaginal discharge -vulvar pruritus. -The pH of the vaginal secretions >5.0. -patchy vaginal erythema and colpitis macularis (“strawberry” cervix) - present
- 17. ◦ Microscopy of the secretions - motile trichomonads -increased numbers of leukocytes. -Clue cells may be present (common association with BV) ◦ The whiff test may be positive. ◦ increased risk for postoperative cuff cellulitis following hysterectomy ◦ Pregnant women with trichomonas vaginitis are at increased risk for premature rupture of the membranes and preterm delivery.
- 18. TREATMENT: ◦ Metronidazole is the drug of choice for treatment of vaginal trichomoniasis. - single-dose (2 g orally) / multidose (500 mg twice daily for 7 days) regimen - The sexual partner should be treated. - Metronidazole gel, although effective for the treatment of BV, should not be used for the treatment of vaginal trichomoniasis. - Women who do not respond to initial therapy -treated again with metronidazole, 500 mg, twice daily for 7 days. -If repeated treatment is not effective-treated with a single 2-g dose of metronidazole once daily for 5 days or tinidazole, 2 g, in a single dose for 5 days.
- 19. -should be tested for other STDs, particularly Neisseria gonorrhoeae and Chlamydia trachomatis. -Serologic testing for syphilis and HIV infection should be considered. - Uncommon refractory cases-obtain cultures of the parasite to determine its susceptibility to metronidazole and tinidazole.
- 20. VULVOVAGINAL CANDIDIASIS ◦ An estimated 75% of women experience at least one episode of vulvovaginal candidiasis (VVC) during their lifetimes. ◦ Few are plagued with a chronic, recurrent infection. ◦ Candida albicans is responsible for 85% to 90% of vaginal yeast infections. ◦ Other species of Candida, such as C. glabrata and C. tropicalis, can cause vulvovaginal symptoms and tend to be resistant to therapy.
- 21. Candida – DIMORPHIC FUNGI -BLASTOSPORES which are responsible for transmission and asymptomatic colonization -MYCELIA result from blastospore germination and enhance colonization and facilitate tissue invasion. • The extensive areas of pruritus and inflammation often associated with minimal invasion of the lower genital tract • A hypersensitivity phenomenon may be responsible for the irritative symptoms associated with VVC, especially for patients with chronic, recurrent disease.
- 23. ◦ Predisposing factors- – antibiotic use – Pregnancy – diabetes ◦ Categorize women with VVC -uncomplicated or complicated disease Uncomplicated Complicated Sporadic or infrequent in occurrence Recurrent symptoms Mild to moderate symptoms Severe symptoms Likely- candida albicans Non albicans candida Immunocompetent women Immunocompromised – DM, HIV
- 24. ◦ Diagnosis The symptoms of VVC consist - ◦ vulvar pruritus ◦ vaginal discharge that typically resembles cottage cheese. ◦ Vaginal soreness, dyspareunia, vulvar burning ◦ External dysuria (“splash” dysuria) -micturition leads to exposure of the inflamed vulvar and vestibular epithelium to urine.
- 25. ◦ The whiff test is negative. ◦ A fungal culture is recommended to confirm the diagnosis. ◦ women with a normal physical examination findings and no evidence of fungal elements disclosed by microscopy are unlikely to have VVC and should not be empirically treated unless a vaginal yeast culture is positive.
- 26. TREATMENT 1.Topically applied azole drugs ◦Symptoms usually resolve in 2 to 3 days. ◦Short-course regimens up to 3 days are recommended. 2.The oral antifungal agent -fluconazole, used in a single 150-mg dose, -Patients should be advised that their symptoms will persist for 2 to 3 days so they will not expect additional treatment
- 27. 3.Women with complicated VVC -150-mg dose fluconazole given 72 hours after the first dose. -Patients with complications treated with a more prolonged topical regimen lasting 10 to 14 days. -Adjunctive treatment with a weak topical steroid, such as 1% hydrocortisone cream, may be helpful in relieving some of the external irritative symptoms.
- 28. RECURRENT VULVOVAGINAL CANDIDIASIS ◦ defined as ≥4 episodes / year ◦ Persistent irritative symptoms of the vestibule and vulva. ◦ Burning replaces itching as the prominent symptom in patients with RVVC. ◦ The diagnosis confirmed by direct microscopy of the vaginal secretions and by fungal culture. ◦ Many of these patients have chronic atopic dermatitis or atrophic vulvovaginitis.
- 29. ◦ TREATMENT : -inducing a remission of chronic symptoms with fluconazole (150 mg every 3 days for three doses). -Patients should be maintained on a suppressive dose of this agent (fluconazole, 150 mg weekly) for 6 months. ◦ On this regimen, 90% of women with RVVC will remain in remission. ◦ After suppressive therapy, approximately half will remain asymptomatic. ◦ Recurrence will occur in the other half and should prompt reinstitution of suppressive therapy .
- 31. DESQUAMATIVE INFLAMMATORY VAGINITIS ◦ Clinical syndrome characterized by -diffuse exudative vaginitis -epithelial cell exfoliation -profuse purulent vaginal discharge ◦ The cause of inflammatory vaginitis is unknown, but Gram stain findings reveal a relative absence of normal long gram-positive bacilli (lactobacilli) and their replacement with gram-positive cocci, usually streptococci. ◦ .
- 32. ◦ Vaginal erythema is present, and there may be an associated vulvar erythema, vulvovaginal ecchymotic spots, and colpitis macularis. ◦ The pH of the vaginal secretions is >4.5 in these patients . ◦ TREATMENT: ◦ 2% clindamycin cream treatment of choice
- 33. ATROPHIC VAGINITIS ◦ Deficency of oestrogen. ◦ Women undergoing menopause ◦ secondary to surgical removal of the ovaries, ◦ Develop inflammatory vaginitis, accompanied by an increased, purulent vaginal discharge. ◦ They may have dyspareunia and postcoital bleeding resulting from atrophy of the vaginal and vulvar epithelium.
- 34. ◦ Examination reveals -atrophy of the external genitalia, along with a loss of the vaginal rugae. -The vaginal mucosa friable . -predominance of parabasal epithelial cells TREATMENT: ◦ Atrophic vaginitis is treated with topical estrogen vaginal cream. -Use of 1 g of conjugated estrogen cream intravaginally each day for 1 to 2 weeks generally provides relief. -Maintenance estrogen therapy, either topical or systemic, should be considered to prevent recurrence of this disorder
- 35. SEXUALLY TRANSMITTED DISEASES ◦ STD ASSOCIATED WITH WHITE DISCHARGE - GENITAL ULCERS- genital herpes granuloma inguinale (donovanosis), lymphogranuloma venereum (LGV), chancroid and syphilis - STD ASSOCIATED VAGINITIS Gonococcal Chlamydia Trichomonas
- 37. -
- 38. GONOCOCCAL VULVOVAGINITIS ◦ Gram-negative intracellular diplococcus -Neisseria gonorrhoea. ◦ The vaginal squamous epithelium is resistant to gonococcal infection. ◦ The gonococci attack the columnar epithelium of glands of Skene, Bartholin, urethra and its glands, cervix and fallopian tubes. ◦ It ascends in a piggy-back fashion attached to the sperms to reach the fallopian tubes.
- 39. Signs and symptoms- ◦ Urinary frequency ,dysuria ◦ dyspareunia, rectal discomfort, ◦ vaginal discharge ◦ pruritus . ◦ Examination – ◦ swollen, painful external genitalia, ◦purulent vaginal discharge ◦erythema surrounding external urinary meatus, ◦opening of the Bartholin’s ducts, vaginitis , endocervicitis. ◦ Late clinical findings: Bartholinitis, Bartholin’s abscess, Bartholin’s cyst, tubo- ovarian abscess, pyosalpinx, hydrosalpinx and blocked tubes. ◦ End result of chronic pelvic infection - chronic pelvic pain, dysmenorrhoea, menorrhagia, infertility with fixed retroversion and at times dyspareunia.
- 40. ◦ DIAGNOSIS ◦ Gram staining of smear prepared from any suspicious discharge. ◦ Culture -Thayer–Martin medium, and McLeod chocolate agar. ◦ Complement fixation tests and PCR staining.. ◦ NAAT from urine, endocervical discharge—95% sensitive ◦ Laproscopy- gonococcal and chlamydial infection showing Fitz-Hugh Curtis syndrome
- 41. ◦ Treatment – ◦ Injecting cefoxitin 2.0 g IM plus probenecid 1.0 g orally ◦ followed by 14 days treatment with oral cap. Doxycycline100 mg bid for 14 days or oral cap. ◦ Tetracycline 250 mg qid for 14 days. Treat the male partner as well
- 42. CHLAMYDIA ◦ Chlamydial infection is common in young. ◦ transmitted by vaginal and rectal intercourse. ◦ caused by -Chlamydia trachomatis -Gram-negative bacterium, ◦ asymptomatic mostly- vaginal discharge, dysuria and frequency of micturition, cervicitis. ◦ During pregnancy, abortion, preterm labour and intrauterine growth retardation (IUGR) may occur. ◦ The cervix is the first site of infection but may spread upwards to develop PID and spread to the partner and neonate. ◦ it may cause salpingitis and infertility,
- 43. ◦ Diagnosis ◦ Immunofluorescence tests on smears prepared from urethral and cervical secretion ◦ IgM can be detected -recent infection. ◦ Enzyme-linked immunosorbent assay (ELISA) ◦ Chlamydia is cultured from the cervical tissue in 5–15% of asymptomatic women. ◦ PCR- fast, highly sensitive and specific -‘gold standard’ in the laboratory diagnosis. ◦ Urine for PCR is simple.
- 44. ◦ Treatment- ◦ Tetracycline 500 mg and clindamycin 500 mg for 14 days are found effective. ◦ The combination of cefoxitin and ceftriaxone with doxycycline (100 mg bid for 14 days) or tetracycline is also useful. ◦ During pregnancy, erythromycin or amoxicillin tid or qid is given for 7 days. ◦ Contact tracing, avoidance of sex or barrier contraceptive is necessary to avoid recurrence.
- 45. References- ◦ Berek and novacks ◦ Shaws gynaecology
- 46. THANK YOU