.-14 - The renal system.pdf
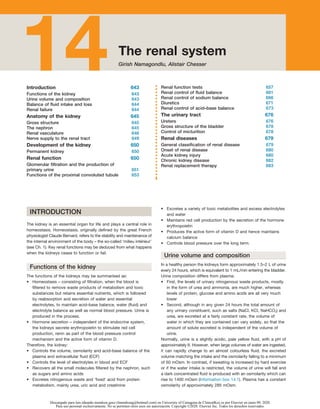
- 1. Introduction 643 14 14The renal system Girish Namagondlu, Alistair Chesser Introduction 643 Functions of the kidney 643 Urine volume and composition 643 Balance of fluid intake and loss 644 Renal failure 644 Anatomy of the kidney 645 Gross structure 645 The nephron 645 Renal vasculature 646 Nerve supply to the renal tract 649 Development of the kidney 650 Permanent kidney 650 Renal function 650 Glomerular filtration and the production of primary urine 651 Functions of the proximal convoluted tubule 653 Renal function tests 657 Renal control of fluid balance 661 Renal control of sodium balance 666 Diuretics 671 Renal control of acid–base balance 673 The urinary tract 676 Ureters 676 Gross structure of the bladder 678 Control of micturition 678 Renal diseases 679 General classification of renal disease 679 Onset of renal disease 680 Acute kidney injury 680 Chronic kidney disease 682 Renal replacement therapy 683 INTRODUCTION The kidney is an essential organ for life and plays a central role in homeostasis. Homeostasis, originally defined by the great French physiologist Claude Bernard, refers to the stability and maintenance of the internal environment of the body – the so-called ‘milieu intérieur’ (see Ch. 1). Key renal functions may be deduced from what happens when the kidneys cease to function or fail. Functions of the kidney The functions of the kidneys may be summarised as: • Homeostasis – consisting of filtration, when the blood is filtered to remove waste products of metabolism and toxic substances but retains essential nutrients, which is followed by reabsorption and secretion of water and essential electrolytes, to maintain acid–base balance, water (fluid) and electrolyte balance as well as normal blood pressure. Urine is produced in the process. • Hormone secretion – independent of the endocrine system, the kidneys secrete erythropoietin to stimulate red cell production, renin as part of the blood pressure control mechanism and the active form of vitamin D. Therefore, the kidney: • Controls the volume, osmolarity and acid–base balance of the plasma and extracellular fluid (ECF) • Controls the level of electrolytes in blood and ECF • Recovers all the small molecules filtered by the nephron, such as sugars and amino acids • Excretes nitrogenous waste and ‘fixed’ acid from protein metabolism, mainly urea, uric acid and creatinine • Excretes a variety of toxic metabolites and excess electrolytes and water • Maintains red cell production by the secretion of the hormone erythropoietin • Produces the active form of vitamin D and hence maintains calcium balance • Controls blood pressure over the long term. Urine volume and composition In a healthy person the kidneys form approximately 1.5–2 L of urine every 24 hours, which is equivalent to 1 mL/min entering the bladder. Urine composition differs from plasma: • First, the levels of urinary nitrogenous waste products, mostly in the form of urea and ammonia, are much higher, whereas levels of protein, glucose and amino acids are all very much lower • Second, although in any given 24 hours the total amount of any urinary constituent, such as salts (NaCl, KCl, NaHCO3) and urea, are excreted at a fairly constant rate, the volume of water in which they are contained can vary widely, so that the amount of solute excreted is independent of the volume of urine. Normally, urine is a slightly acidic, pale yellow fluid, with a pH of approximately 6. However, when large volumes of water are ingested, it can rapidly change to an almost colourless fluid, the excreted volume matching the intake and the osmolarity falling to a minimum of 50 mOsm. In contrast, if sweating is increased by hard exercise or if the water intake is restricted, the volume of urine will fall and a dark concentrated fluid is produced with an osmolarity which can rise to 1400 mOsm (Information box 14.1). Plasma has a constant osmolarity of approximately 285 mOsm. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 2. 644 The renal system 14 measuring GFR. Over the years, calculation methods have become more accurate and have lesser bias. A commonly used method, which is easy and reasonably reliable, is estimating GFR by the chronic kidney disease epidemiology collaboration formula (CKD-EPI), which is based on age, sex, race, and serum creatinine; it is popularly known as estimated glomerular filtration rate (eGFR). In healthy individuals, the GFR is a very large volume of fluid – 125 mL/min in the young male (equivalent to 180 L/24 h). Blood urea and serum creatinine are commonly measured but are surrogate and late markers of renal failure (Fig. 14.1). Levels only increase in the blood when 50% of kidney function is lost. For a healthy person on a mixed diet, the level of plasma urea is approximately 5 mM and it does not begin to change until the GFR has fallen by approximately 75%. However, this response does depend on diet – a high protein intake in a meat eater would cause the plasma urea to rise more rapidly in renal disease, whereas a vegetarian diet would delay this rise until an even greater loss of renal function had occurred. Often, prior to the rise in plasma urea, the blood pressure begins to increase to high levels at rest (hypertension) and this can be an early warning sign of renal problems (Clinical box 14.2). Balance of fluid intake and loss In a healthy human, the daily intake of water roughly equals loss in the steady state. The principal source of water is drinking water and other fluids and in food (oral), and most of the loss is in urine, via the kidneys. Some water is lost as ‘insensible loss’, via respiration, skin, sweating and faeces. Table 14.1 shows the approximate balance of the total intake and loss of water by the body over 24 hours and the electrolyte balance, and the factors that can disturb this balance. Renal failure In a person whose kidneys are beginning to fail, there is at first no detectable sign or symptom of damage because humans have a massive over-capacity in renal function. Few changes are seen until three-quarters of the normal renal function is lost (Clinical box 14.1). Symptoms appear late in renal failure and are usually: • A result of waste product accumulation, mainly urea (uraemia), such as loss of appetite, lethargy, nausea, vomiting, weight loss, itching (uraemic frost), muscle cramps etc. • The inability to excrete water (fluid overload), resulting in breathlessness, orthopnoea, oliguria and peripheral oedema. An early feature of renal failure is a drop in the glomerular filtration rate (GFR) by all the nephrons (see later). There are several ways of Information box 14.1 Osmolarity Osmolarity measures the concentration of ‘particles’ that are capable of exerting osmotic pressure, so that the osmolarity of a solution reflects the number of ‘particles’ in a given volume of fluid that can exert an osmotic pressure across a membrane. The kidneys are vital in keeping the osmolarity of blood and the extracellular fluid (ECF) constant. The kidneys are therefore a key element in the control of electrolytes and acid–base balance in the body. Sodium as NaCl and NaHCO3 is conserved, whereas potassium is eliminated and ‘fixed’ acid is excreted in the form of ammonia and phosphate ions in the urine. Table 14.1 Water balance and factors which disturb the balance Sources for the input of water Litres Sources of output Litres Water content in food 1.0 Urine osmotic load 0.7 Food metabolism 0.5 Urine from choice drinking 0.8 Drinking minimum 0.5 Lungs and airways 0.4 Drinking by choice 1.0 Skin insensible loss 1.0 Faeces 0.1 Total 3.0 Total 3.0 Factors disturbing balance Composition and route Hyperventilation/fever Loss of pure H2O – diffusion through skin Sweating H2O + Na+ , Cl− – sweat glands and ducts Air conditioning (dry air) 0.5–1 L/day pure H2O – diffusion into lungs Diarrhoea – cholera 20 L in 48 h Na+ , Cl− , HCO3 – , K+ – small bowel/colon Lactation – milk Isotonic salts – milk secretion, breasts Clinical box 14.1 Clinical consequences of renal failure The consequences of renal failure are related to kidney functions other than fluid balance and excretion, which include: • Hypertension – the kidneys secrete the enzyme renin in response to impaired renal perfusion. Renin activates angiotensin-converting enzyme (ACE) to convert angiotensin I to angiotensin II, which is a powerful systemic vasoconstrictor and stimulates aldosterone secretion to promote sodium and water retention (see later and Ch. 4). Chronic disruption of the renin–angiotensin–aldosterone system in renal failure leads to hypertension. Pharmacological treatment with ACE inhibitors is used in the management of hypertension (see later). Before the advent of effective hypotensive drugs, nephrectomy was performed to prevent renal hypertension. • Cardiovascular disease – is the major cause of death in renal failure patients. Ischaemic heart disease is common and often a combination of arteriosclerosis and atherosclerosis. Incidence of cardiac arrhythmias and sudden cardiac death is increased in chronic kidney disease (CKD). • Anaemia – renal interstitial cells secrete erythropoietin, which stimulates red cell production (see Ch. 12). Destruction of renal tissue in CKD results in iron and erythropoietin deficiency. • Vitamin D deficiency – the distal convoluted tubules secrete the enzyme 1α-hydroxylase. Naturally occurring vitamin D needs to be hydroxylated to an active metabolite in the liver, then further converted by 1α-hydroxylase to produce the metabolically active 1,25-dihydroxychlolecalciferol (vitamin D3). Chronic renal failure thus leads to disorders of bone (renal osteodystrophy), calcium metabolism and secondary hyperparathyroidism (see Chs 10 and 16). • Hypoproteinaemia – the persistent and chronic urinary protein loss in chronic renal failure leads to hypoproteinaemia, which can lead to impaired protein binding with consequent adverse reactions from therapeutic agents (see Ch. 4), wasting and malnutrition (see Ch. 16). • Other metabolic complications – e.g. defective excretion of urate leads to gout; defective insulin excretion may lead to hypoglycaemia in insulin-dependent diabetics. • Other endocrine disorders – may arise owing to defective protein binding of hormones consequent to hypoproteinaemia (e.g. thyroid hormone), or impairment of hormone action and excretion (e.g. hyperprolactinaemia leading to gynaecomastia in men, growth retardation secondary to complex defects of growth hormone secretion and action in uraemic children). • Neurological complications – severe, persistent uraemia depresses cerebral function and may lead to convulsions (see also Ch. 3). Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 3. Anatomy of the kidney 645 14 Renal pyramids In longitudinal section, the kidney is divided into a number of conical structures, the renal pyramids (see Fig. 14.2). The gross structure also reflects the highly organised microstructure with linear feature, the medullary rays, arranged into the inner and outer stripes. These are related to the capillary networks and to the straight tubular elements of the loop of Henle, the vasa recta and the collecting ducts (see later). The tip of each pyramid forms a papilla which is enclosed in a funnel-shaped extension of the renal pelvis, the calyx. It is these structures which collect the urine draining from the collecting ducts passing through renal papilla at the apex, into a minor calyx (usually 9–12), then into a major calyx (3–4) before passing through the renal pelvis into the ureters via the pelviureteric junction. The walls of calyces, renal pelvis and ureters are lined with smooth muscle, which produces peristaltic waves to carry urine down the ureter and into the bladder. The nephron The functional unit of the kidney is the nephron, of which there are some 800000 to 1.5 million in each kidney. Each nephron consists of the renal corpuscle, where the primary urine is first formed, and the renal tubule, a highly coiled tube where the primary urine is modified. A simplified overall structure of the nephron is shown in Fig. 14.3. The renal corpuscle (renal glomerulus) The renal corpuscle, the filter in the kidney sited in the cortex, consists of the glomerulus, which is a knot of capillaries attached to the mesangium, surrounded by the Bowman capsule where fluid is forced out of the plasma into Bowman space to form the glomerular filtrate. The Bowman capsule, also known as the glomerular capsule, elongates to become the renal tubule. It has an inner layer formed by visceral epithelial cells (podocytes), which, at the vascular pole, is reflected to form the outer layer (parietal epithelial cells). ANATOMY OF THE KIDNEY Gross structure The adult kidneys are two ‘bean’-shaped structures weighing approximately 150 g each, lying on either side of the vertebral column (at approximately the level of T12–L3) in the midline, but outside the peritoneum in the abdominal cavity (retroperitoneal). The concave aspect of each kidney faces medially (towards the vertebral column). Each kidney normally measures 10–12 cm in length, 5–7 cm in width and 2–3 cm in thickness. The kidneys are surrounded by three layers of tissue: • Renal fascia (Gerota fascia) – a thin, outer layer of fibrous connective tissue that surrounds each kidney (and the attached adrenal gland). • Adipose capsule – a middle layer of fat tissue that cushions the kidneys. • Renal capsule – an inner, thick, fibrous membrane. The thickness of the capsule is necessary to withstand the high tissue pressure of 10 mmHg generated within the tissue ECF by the filtration process. The inside of the kidney has three distinct regions: • Outer cortex borders the convex side and lies immediately under the capsule. It contains the renal corpuscles and tubules (apart from the ‘hairpin’ loop of Henle), blood vessels and the cortical collecting ducts (see later). The renal filtration processes take place in the cortex. • Inner medulla (Fig. 14.2) which is deep to the cortex, contains 10–20 striated, cone-shaped regions called renal pyramids. This alternates with an unstriated region called renal columns. • Renal sinus which lies adjacent to medulla and opens to the hilum (an opening in the medial aspect of the kidney) that allows passage of the renal artery and vein, nerve supply and ureters (see Fig. 14.2). 0 0 120 ml/min Dietary protein Creatinine clearance GFR (ml/min) Blood urea (mmol/L) 30 30 60 90 High Normal Low 10 20 20 0 0 1.0 2.0 3.0 4.0 5.0 6.0 7.0 8.0 100 120 140 160 180 40 60 80 Plasma creatinine (mg/dL) A B Fig. 14.1 (A) The relationship between blood urea concentration and creatinine clearance showing the effect of high, normal and low protein intakes. (B) Relationship between true glomerular filtration rate (GFR) (as measured by inulin clearance) and plasma creatinine concentration in 171 patients with glomerular disease. The open circles joined by the solid red line represent the relationship that would exist if creatinine were excreted solely by glomerular filtration; the dashed line represents the upper limit of ‘normal’ for plasma creatinine concentration of 1.4 mg/dL. In patients (dark dots), variations in GFR between 129 and 60 mL/min were often associated with a plasma creatinine concentration that remained within the normal range due to increased creatinine excretion, which becomes saturated at a plasma concentration above 1.5–2 mg/dL; as a result, plasma creatinine concentration rises as expected with further reductions in GFR. Redrawn with permission from Richards P, Truniger B 1983 Understanding water electrolytes and acid base balance. William Heinemann, London. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 4. 646 The renal system 14 medulla. The PCT is lined by cuboidal cells having fine densely packed microvilli (brush border) on the luminal side (urine side). Each cell is joined to the others around it, close to the luminal boundary, by an occluding band of tight junctions. The base of each cell (blood side) is inwardly convoluted in many folds which interdigitate with the cells around it. These structures enormously expand the surface of the cell for exchange processes. The cells are also densely filled with mitochondria, which are always present in cells that are metabolically active and use energy generated from glucose and oxygen. Loop of Henle After the PCT, the nephron then descends from the cortex towards the medulla via the hairpin loop of Henle. There are three types of loop: • Loops from juxtaglomerular nephrons which are very long and extend all the way down to the renal pyramids (medulla). • Loops from cortical nephrons which are short and only reach the cortex/medulla border. Approximately 80% of nephrons have short loops. • A few intermediate loops between the above types. The functional reasons for the differences in the length of the loops are not fully understood but desert animals that produce a highly concentrated urine have the highest proportion of the long loops. The loop of Henle consists of several cell types; the bulk of this structure is the thin descending and thin ascending loops. The cells of this region are sparse in number, and are narrow, with few infoldings on either face and few mitochondria. The loop of Henle is amazingly long, the length being approximately 1000 times the diameter, and if Fig. 14.3 was drawn to scale, it would be as high as a 20-storey building! After the thin ascending loop, the next section undergoes a major change in structure, becoming the thick ascending loop. The cells in this section are thick, complex and rich both in mitochondria and cellular inclusions, which reflects their active transport functions. Distal convoluted tubule Fluid now leaves the loop of Henle and enters the DCT, which is in the renal cortex. Here, 10%–15% of ions and fluid of the filtrate are recovered. Tubules from five to six nephrons then merge to form the larger CD, which re-enters the renal medulla. Up to this point the fluid recovery is a fixed proportion of that which has been filtered, and is said to be constitutive. Collecting ducts The CDs are derived from a different embryological origin than the rest of the nephron, and are divided into a cortical section (cortical collecting duct (CCD)) and a medullary section (medullary collecting duct (MCD)). In these ducts the fluid recovery can be varied either to produce a dilute or a concentrated urine under the influence of the antidiuretic hormone (ADH), also called vasopressin (see later). Renal vasculature Each kidney is supplied by a large artery from the descending aorta, and together they receive approximately 20% of the cardiac output (1.2 L/min). After circulating through the medulla and cortex, blood from renal capillaries is collected in renal venules and leaves the kidney via the renal vein to join the inferior vena cava. The kidneys also have a prominent lymphatic drainage. The renal arteries enter the kidney on the medial surface of each kidney via the hilum, through which the renal artery enters and the veins and lymphatics exit; here also the renal nerves enter and leave the kidney. The renal tubule The renal tubule is the reabsorptive part of the renal system. It is a highly convoluted structure, varying in size throughout its length, consisting of: • Proximal convoluted tubule (PCT) • Loop of Henle • Distal convoluted tubule (DCT) • Collecting ducts (CDs). Although originating in the renal cortex, the renal tubule descends into the medulla as the hairpin loop of Henle (see later), which doubles back so that the DCT returns to the cortex, ending next to the glomerulus of the same nephron. Proximal convoluted tubule The fluid formed by the glomerular capillaries flows from Bowman space along the nephron into the highly coiled structure of the PCT. The PCT is grossly divided into pars convoluta (initial convoluted portion) and pars recta (straight portion) that descends into the Clinical box 14.2 Renal failure Renal failure occurs when glomerular filtration is compromised from a variety of causes, but may also be the consequence of renal tubular function: • Pre-renal – due to depressed renal vascular perfusion so that the hydrostatic filtration forces are reduced. Causes can be divided into: – True volume depletion, e.g. hypotension, dehydration, vomiting, diarrhoea, haemorrhage (gastrointestinal blood loss), shock – Decrease in ‘effective’ circulating blood volume, e.g. heart failure, liver failure, NSAIDs and ACE inhibitors. • Renal – often called intrinsic renal disease and is due to disease of the nephron, the glomeruli and or microvasculature, or the tubules, e.g. microvascular disease as in diabetes mellitus (see Ch. 3), nephrotoxic drugs, acute tubular necrosis. – Renovascular – Macrovascular – renal artery stenosis, renal vein thrombosis – Microvascular – small vessel disease, e.g. diabetes mellitus, vasculitis. – Renal parenchymal – Glomerulonephritis – nephritic syndrome, rapidly progressive glomerulonephritis, nephrotic syndrome – Tubulointerstitial disease – ATN, tubulointerstitial nephritis. • Post-renal – due to obstruction anywhere in the outflow system: the renal pyramid (calyces, pelvis), ureters, down to the bladder neck, or recurrent ascending infections (e.g. pyelonephritis). Renal failure may be acute or chronic: • Acute kidney injury is the sudden deterioration of renal function, which is usually reversible over time. When severe, the consequent fluid and biochemical disturbances may be life-threatening and constitute a medical emergency. Management of acute renal failure is aimed to correct the fluid and biochemical imbalance during the time needed for renal function to recover. Dietary controls of electrolyte, nitrogen and water intake (see Ch. 16), pharmacological interventions (see Ch. 4) and dialysis to remove toxic products of metabolism and excess fluid may be necessary. • Chronic kidney disease is a long-standing and progressive impairment of renal excretory function, which may be insidious in onset and should be diagnosed after at least 3 months of persistent renal failure. The biochemical abnormalities may be undetected for long periods. Causes of chronic renal failure may be congenital (see later) and include glomerular or vascular disease. Treatment is aimed at controlling the biochemical and fluid imbalances (including chronic dialysis), and at the cause, e.g. tight glycaemic control in diabetes mellitus, and to manage complications. Renal transplantation may ultimately be needed. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 5. Anatomy of the kidney 647 14 the peritubular capillaries, which envelop both the PCT and DCT, or descending as looped capillaries into the medulla of the kidney as the vasa recta around the loop of Henle (see Fig. 14.4). Blood flowing through the glomerular capillaries is under high pressure, whereas the tubular capillaries and vasa recta are under low pressure. Glomerular filtration barrier Filtration of the blood entering the glomerulus at the afferent arteriole relies on the permeability of the glomerular filtration barrier, which is formed inside out by (Fig. 14.5): • Capillary endothelial cells with round to oval fenestrations (holes or pores) measuring 50–100 nm. • Glomerular basement membrane (GBM) consisting of a fibrillar network of matrix proteins, rather like an irregular fishing net, but with holes of a fairly consistent size. Each of these ‘holes’ Renal microvasculature On entering the kidney, the renal artery divides to form interlobar vessels, which supply each pyramid. These then subdivide to form arcuate arteries and finally interlobular arteries supplying the grape-like glomerular capillaries (Fig. 14.4), where the renal filtrate is formed. The arterial supply enters the start of the nephron at the blind-ended dilation, the Bowman capsule, and divides into a knot of capillaries, the glomerulus. The glomerular capillaries are unusual in that they have an arteriole at the start of the capillary bed, the afferent arteriole, and a second arteriole, the efferent arteriole, at the end of the glomerulus, where the capillaries combine to emerge from the Bowman capsule. Peritubular capillaries The glomerular capillaries reunite into an efferent arteriole which then divides again to form a second capillary bed, becoming either Cortex Renal artery Renal vein Arcuate Interlobular Arteries Interlobar Area of ureter prone to narrowing and collection of stones Longitudinal muscle Circular muscle Urothelium Medullary pyramid Pelviureteric junction Calyx Capsule Pelvis Vesicoureteric junction Trigone (on floor of bladder) External urethral sphincter Urethra Abdominal pressure Ureter Brim of pelvis Detrusor muscle Fig. 14.2 The major components of the urinary tract and bladder. Note the pelviureteric junction, the brim of the pelvis and the vesicoureteric junction, which are sites where renal stones can lodge and impede urine flow, so causing back pressure and renal damage. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 6. 648 The renal system 14 Proximal convoluted tubule Juxtamedullary nephron Interlobular artery and vein Afferent arteriole Arcuate artery and vein Collecting duct Interlobar vein Interlobar artery Vasa recta Distal convoluted tubule Collecting duct Papillary duct Thick ascending loop of Henle Thin ascending loop of Henle Thin descending loop of Henle Medulla Outer zone Inner stripe Outer stripe Inner zone Cortex Fig. 14.3 Structure of the nephron. Primary urine formed within the glomerulus is modified during its passage along the kidney tubules before entering the collecting duct from where it goes to the bladder for excretion. The zones of the kidney are shown on the left-hand side with the major blood vessels that supply the kidney. The nephron shown is the juxtaglomerular nephron, consisting of the proximal convoluted tubule (PCT), which dips deep into the medulla as the thin descending loop of Henle, then bends acutely as the thin ascending loop of Henle and then becomes the thick ascending loop. The thick ascending loop of Henle emerges into the cortex to form the distal convoluted tubule (DCT). The DCTs merge to form the collecting duct, which again descends into the medulla and forms the urine. The changing morphology of the tubule walls reflects the differences in permeability and function. The macula densa, a densely packed group of specialised cells lining the DCT, is at the top of the thick ascending loop of Henle, a key site for the control of sodium balance. Some nephrons only penetrate into the outer medulla, the cortical nephrons. It is thought the nephrons with the longest loops of Henle are responsible for forming the most concentrated urine. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 7. Anatomy of the kidney 649 14 enabling them to withstand the large filtration pressures which are needed to form the urinary filtrate. Filtration through the glomerular capillary wall occurs along an extracellular pathway including the endothelial pores, the GBM and the slit diaphragm. Thus, formed filtrate enters Bowman space and then pass through tubules. The main challenge for the glomerular capillaries is to combine selective leakiness with stability. Nerve supply to the renal tract The kidney is supplied via the renal plexus and the course is along the renal arteries to reach each kidney: • Sympathetic nervous system triggers vasoconstriction in the kidney and reduces renal blood flow. This travels through T10–T11 levels of the spinal cord. • Parasympathetic nerve supply is through the renal branches of the vagus nerve (cranial nerve X). The function of this is not yet clear. Nerve supply of the ureters is from the following sources: • Renal plexus • Aortic plexus • Superior hypogastric plexus • Inferior hypogastric plexus • Testicular (or ovarian) plexus. Nerve supply to the bladder is described in detail on pages 678–679. Nerve supply to the sphincters controlling urethral orifice is from has negative charges on the surface of the matrix, so molecules with a similar charge would be repelled by these charges. In health, this prevents negatively charged molecules from being filtered out of the blood (see later). Matrix proteins consist of type IV collagen (α3, 4 and 5 chains), laminin, fibronectin, entactin, other negatively charged glycoproteins and sulphated glycosaminoglycans, such as heparin sulphate. • Podocytes have foot processes, which are finger-like projections of the capillary epithelium that interdigitate with each other, leaving between them filtration slits, which are bridged by an extracellular structure, the slit diaphragm. The foot processes enclose and strengthen the vessels, so Collecting duct Loop of Henle Renal vein Renal artery (branch) Efferent arteriole Glomerulus Bowman space Proximal tubule Peritubular capillaries Distal tubule Bowman capsule Afferent arteriole Vasa recta Fig. 14.4 Renal vasculature. The blood supply originates from the renal artery (red) and leaves via the renal vein (blue). Blood passes through two capillary beds, the glomerular capillaries followed by the vasa recta. Bowman capsule Lamina densa Basement membrane Lamina rara Lamina rara Endothelial cell Fenestra Epithelial foot process Slit membrane Capillary lumen Fig. 14.5 Glomerular capillary wall. The structure of the glomerular capillary wall, which is the filtration pathway. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 8. 650 The renal system 14 and partly from the Wolffian duct. At approximately the fifth or sixth week of gestation, the Wolffian duct develops a diverticulum, the ureteric bud, which eventually becomes the renal pelvis and calyces (proximal and distal convoluted tubules, loop of Henle, collecting tubules), and the ureters. The ureteric bud invades the cell mass of the intermediate mesoderm, when cells from the mesoderm migrate over the ureteric bud and differentiate to eventually form the excretory part of the kidneys, the nephrons (the renal cortex, glomeruli). The metanephros migrates upwards to the lumbar region to take up the lumbar position of the adult kidney. The ureters elongate as the metanephros ascends. Permanent kidney The ureteric buds bifurcate until the 32nd week of gestation producing 1–3 million CDs (Fig. 14.6). At the tip of each is a metanephric tissue cap (metanephric blastema, containing cells capable of asexual division and differentiation; see Fig. 14.6B) which forms the nephric vesicle (see Fig. 14.6C). This eventually forms the Bowman capsule and the rest of the nephron. As the vesicle elongates, a capillary complex forms near one end and invaginates into the tubule to form the Bowman capsule and glomerulus (see Fig. 14.6D–F). Between the sixth and ninth week, the kidneys ascend to a lumbar site just between the adrenal glands (Fig. 14.7). By the 10th week, the metanephros has evolved into the cortex and medulla, and each ‘tree’ of CDs drains into a minor calyx and converges to form the renal papilla. Urine produced by the foetus is excreted into the amniotic fluid but kidney function is not necessary until after birth. Congenital renal agenesis Congenital renal agenesis leads to the absence of one (unilateral renal agenesis) or both (bilateral renal agenesis) kidneys at birth. Bilateral renal agenesis is rare but incompatible with life. While in utero, the absence of foetal kidneys leads to a deficiency in amniotic fluid production (oligohydramnios or anhydramnios). Without amniotic fluid to cushion the foetus, the foetal facial and other features become ‘squashed’. The combination of absent kidneys, oligohydramnios and characteristic features is sometimes referred to as Potter syndrome (also called Potter sequence, oligohydramnios sequence). Unilateral renal agenesis is more common but not life-threatening as long as the single kidney remains healthy. Polycystic kidney disease Polycystic kidney disease is characterised by multiple renal cysts (Clinical box 14.4). The autosomal dominant form of polycystic kidney disease (ADPKD) is a hereditary disorder presenting in adulthood, with associated other organ abnormalities (e.g. liver cysts). Autosomal recessive polycystic kidney disease is rare, thought to be due to gene mutation and is fatal in early childhood. RENAL FUNCTION In healthy individuals, the kidneys filter 180 L (125 mL/min) of fluid in 24 hours, excreting 1.5–2 L as urine (see earlier). They are also involved in the retention of essential nutrients such as protein and glucose; water, acid–base and electrolyte balance; and hormone secretion, as well as the excretion of waste products of metabolism. The complex processes concerned are: • Filtration • Reabsorption, which may be passive or selective • Secretion. pudendal nerve, pelvic splanchnic nerves and inferior hypogastric plexus. DEVELOPMENT OF THE KIDNEY In humans, the embryonic kidneys originate from the intermediate mesoderm (see Ch. 10). The reproductive organs and adrenal cortex also develop from the intermediate mesoderm. The tissues that are destined to become permanent kidneys are preceded by embryonic structures, most of which degenerate and atrophy before birth. Clinical box 14.3 describes some congenital abnormalities of the kidneys and urinary tract. There are three stages in the development of these embryonic structures: • Pronephros • Mesonephros • Metanephros. Pronephros Cells that develop into the pronephros originate in the intermediate mesoderm. Structures known as the cervical nephrostomes, at the level of the fifth cervical to the third thoracic segments, grow as evaginations from the segments to fuse and extend in a caudal direction (downwards) to form a series of ducts, the pronephric ducts (or nephric ducts). Within the ducts, glomeruli develop. The pronephric ducts and glomeruli make up the pronephros. The Wolffian duct forms below the pronephric duct. The pronephros is not functional, and rapidly degenerates and disappears at an early stage. Mesonephros The mesonephros originates in the cell mass on the medial side of the Wolffian duct (from approximately the sixth thoracic to the third lumbar segment), developing into a series of tubules. One end of the tubules dilates and is invaginated by capillaries to form glomeruli. The mesonephros is functional until the fifth gestational week, but atrophies rapidly from the sixth week onwards. Metanephros The metanephros is destined to become the permanent kidney. It arises partly from the caudal end of the intermediate mesoderm Clinical box 14.3 Congenital abnormalities of the kidneys and urinary tract Congenital malformations of the kidneys and urinary tract (CAKUT) are relatively common. Many are asymptomatic and only detected during investigative (e.g. excretion urogram, ultrasound examination) or therapeutic procedures (e.g. laparotomy). Some conditions, however, lead to serious complications, such as progressive renal failure, and require surgical interventions or even renal transplantation. The aetiology of the anomalies is generally unknown, but genetic mutation and chromosomal anomalies have been proposed. The congenital defects include: • Defect in embryonic development owing to abnormal interaction between the ureteric bud and metanephric blastema, which may lead to agenesis (failure to develop), hypo- or dysplasia of the kidneys, vesicoureteric reflux (VUR) (see later, Clinical box 14.14) and congenital malformation of the ureters (ectopic or double ureters) among others. • Hereditary autosomal dominant or autosomal recessive polycystic kidney disease. • Embryological errors with one kidney failing to ascend (ectopic kidney) or the two kidneys fusing to form a horseshoe kidney, which is still functional and is only incidentally detected (see Fig. 14.7E). Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 9. Renal function 651 14 capillaries, most probably through the gaps between the endothelial cells and through the fenestrae (regions of thinning of the wall) in the capillary wall (see Fig. 14.5). The fluid then passes between the epithelial podocytes, and between these structures lies the basement membrane. This is the filter bed of the kidney which holds back plasma proteins from passing into the nephron (see earlier). From measurements of the permeability of molecules of different sizes, all molecules of less than 12000 molecular weight (MW 12000) are filtered into the nephron. This implies that all electrolytes, sugars, amino acids, vitamins etc., pass easily into the Bowman capsule Different parts of the nephron perform different functions. Fig. 14.8 is a simplified diagrammatic representation of how the nephron functions. See also Renal Filtration Made Easy online (www.studentconsult.com). Glomerular filtration and the production of primary urine Urine is formed by the capillary hydrostatic pressure (HP) forcing the water and salts of plasma through the wall of the glomerular Collecting ducts Collecting ducts Metanephric tissue cap Nephric vesicle Glomerulus Bowman capsule Loop of Henle Distal convoluted tubule Proximal convoluted tubule A B C D E F Fig. 14.6 Development of the renal collecting system and nephrons. (A) The ureteric buds continue to bifurcate until the 32nd week, producing 1–3 million collecting ducts (B–F). The tip of each collecting duct induces the development of a metanephric tissue cap, which differentiates into a renal vesicle. This vesicle ultimately forms a Bowman capsule and the proximal and distal convoluted tubules and loop of Henle. Functional nephric units (of the type shown in (E)) first appear in distal regions of the metanephros at 10 weeks. Dorsal aorta Renal artery Ureter Ureter Sixth week Normal Pelvic kidney Horseshoe kidney A B C D E Fig. 14.7 Normal and abnormal ascent of the kidneys from the pelvis. (A–C) The metanephroi normally ascend from the sacral region of their definitive lumbar position between the sixth and ninth week. (D) Infrequently, a kidney may fail to ascend, resulting in a pelvic kidney. (E) If the inferior poles of the metanephroi make contact and fuse before ascent, the resulting horseshoe kidney catches under the inferior mesenteric artery. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 10. 652 The renal system 14 and then must be recovered by the rest of the nephron, back into the plasma. Pore size and macromolecules If it is assumed that the ‘holes’ (pores) in the basement membrane are tiny cylinders in the wall of approximately 1.4 nm in diameter, as the size of the molecule approaches the diameter of the pore, it will have less and less chance of being filtered. The size of a molecule is usually judged by its MW, but this can be misleading because some molecules are spherical (globular), whereas others are long and thin. This latter group may get through into filtrate in small amounts by passing ‘end on’ through the pores, although from their MW it could be assumed that they are far too large; this effect may explain why a small quantity of even the largest proteins do get filtered into the urine, although there may also be a small population of large pores. However, the most critical factor that affects the filtration of a macromolecule is whether it has a surface charge. Haemoglobin Clinical box 14.4 Polycystic kidney disease The pattern of inheritance for polycystic kidney disease is autosomal dominant (ADPKD), which means that each offspring has a 50% chance of inheriting the responsible mutation and, hence, the disease. ADPKD is a genetically heterogeneous condition that involves at least two genes. PKD1 is located on 16p13.3 and accounts for most ADPKD cases (85%). PKD2 is located on 4q21-q22 and accounts for 15% of ADPKD cases. ADPKD presents earlier in life. ADPKD1 is more severe than ADPKD2. The mean age of end-stage renal disease for patients with ADPKD1 and ADPKD2 is 53 years and 74 years, respectively. Clinical features are usually loin pain, haematuria, urinary tract infections, renal stones, hypertension and progressive renal failure. Approximately 20%–25% have polycystic liver, 10%–15% have mitral valve prolapse and 5%–50% have berry aneurysms. Differentiating features from other causes of multicystic disease is that ADPKD patients have bigger kidney size/volume and there is usually a strong family history. Management involves analgesics, good control of BP and proteinuria and prompt treatment of urinary tract infections. Collecting duct Renal blood flow (25% of cardiac output) Renin from afferent arterioles Juxtaglomerular apparatus Glomerulus Secretion Toxic metabolites Filtrate: G, AA, anions, cations, proteins <20000, urea Proximal convoluted tubule Thick ascending limb Loop of Henle Thin descending limb Urea Urine Vasa recta Urine concentration and dilution Counter-current hypothesis Thin ascending limb Distal convoluted tubule H2O Na+ Cl– Na+ Cl– Na+ Urea Aldosterone Reabsorption: Na+, Cl– , K+, hydrogen ion exchange, H2O Reabsorption: Water Vasopressin Reabsorption: G, AA, Na+, Cl– , K+ , HCO3 – Peritubular circulation Medulla Cortex Medulla Cortex 80% 20% Fig. 14.8 Diagrammatic representation of major transport sites in the nephron. Apart from macromolecules, the glomerular filtrate contains glucose, amino acids, electrolytes such as Na+ , K+ , Cl− , urea, bicarbonate and water. The PCT is the major site for reabsorption: 99% of the glucose is reabsorbed into the peritubular circulation, as well as essential nutrients and electrolytes. Bicarbonate reabsorption at the PCT affects renal acid–base homeostasis. Toxic metabolites, cations and anions are also secreted by the PCT. The loop of Henle is the major site for urine concentration according to the counter-current hypothesis. Further NaCl and water reabsorption takes place in the DCT and CT, controlled by vasopressin and aldosterone. AA, amino acid; CT, collecting tubule; DCT, distal convoluted tubule; G, glucose; HCO3 – , bicarbonate; PCT, proximal convoluted tubule. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 11. Renal function 653 14 • It is the prime site for both the recovery of bicarbonate and the generation of new bicarbonate depending on the arterial pCO2 • It secretes a number of organic acids and bases, as well as a wide variety of toxic and fat-soluble molecules into the urine. This latter function means that the level of these compounds is higher in the urine than in the blood capillaries (see later). Urinary organic acids and bases, as well as toxic and fat-soluble molecules, can be in excess of endogenous molecules, from administered drugs or dietary sources. These functions involve a wide range of different types of transport and a large number of different carrier molecules (Fig. 14.9). Most of these processes require energy. The renal metabolic processes are aerobic and consume large amounts of oxygen, almost equal to cardiac muscle. Tight junctions Each epithelial cell of the PCT is joined to those surrounding it by an occluding band of tight junctions close to the apical, or urine, side of the cells (rather like the plastic holding a ‘six-pack’ of soft drink cans); these junctions can vary in their ‘tightness’ or permeability. In the PCT, they are ‘moderately leaky’, so, although they slow the rate of passage of small molecules between cells, they do not permit steep gradients to be established between the lumen and the blood across the whole epithelium. Any concentration gradients established between the cells on the blood side of the PCT by the transport processes across the cell wall will osmotically draw fluid and some ions through these ‘leaky’ tight junctions. This process helps to recover water, salts and other small molecules back into the blood by a relatively low-energy-cost process. This recovery of water is mainly aided by a member of cellular water channels called aquaporins (AQPs). Aquaporin 1 (AQP1) is localised in the apical and basolateral region of the PCT epithelial cell membrane (see Fig. 14.9A). AQP1 is not regulated by vasopressin, whereas AQP2, located in the apical plasma membrane and intracellular vesicles of CD principal cells, is regulated by vasopressin. The high permeability of the PCT enables a vast volume of fluid to be recovered at low energy cost. The PCT only uses approximately 5% of the total energy consumption of the kidney. The sodium pump The ‘power house’ which drives most of the processes in the kidney is the sodium pump (sodium–potassium pump, Na+ /K+ -ATPase pump), located in the basolateral membrane of the tubular epithelial cells. All cells in the body have the ability to pump sodium from inside the cell across the cell membrane into the ECF (see Ch. 1). The pump requires energy in the form of adenosine triphosphate (ATP), which is generated from oxygen and glucose. The pump must also have K+ on the outside of the cell, and it usually pumps 3Na+ out of the cell for every 2K+ transferred in the opposite direction. Transport of sodium in PCT by this pump is an example of primary active transport (uphill against electrochemical gradient). The walls of the epithelial cells of the PCT are polarised, which is to say they have functionally different properties on the luminal (urine) side compared with the blood side of the cell (see Fig. 14.9B). The sodium pumps are only found on the blood side of the cell, as tight junctions between the epithelial cells maintain the differential distribution of membrane proteins between apical and basal membranes, and this difference enables the cells to transport ions and non-electrolytes from the urinary filtrate back into the blood. A rise in intracellular Na+ concentration increases sodium pump activity, to ‘pump’ Na+ ions out of the cell into the ECF. The pumping (MW 67000) escapes into the urine, whereas albumin (MW 62000), although smaller, is not filtered. This is related to the fact that although both molecules are globular proteins, albumin has a negative surface charge, so is held back by the repulsion of the charges on the fibrillar matrix of the basement membrane, whereas haemoglobin is not charged, so it can pass through relatively freely. In disease states the surface charge on the fibrillar matrix can be disturbed and albumin now appears in the urine (albuminuria), which is a useful early warning sign of kidney injury. Filtration forces The HP at the afferent arterioles as they enter the glomerulus is approximately 50 mmHg, which is approximately 15 mmHg higher than most other systemic capillaries. The capillary HP only falls by 5 mmHg along the length of the glomerular capillary to 45 mmHg in the efferent arterioles. This large HP and high permeability of the capillary walls causes a large fraction of fluid and small molecules to be filtered into the Bowman capsule of the nephron. This ‘outward’ force is, however, balanced by the opposing pull of the plasma proteins which, being too large to pass through the wall, exert an osmotic force in the opposite direction to the HP force. This is the colloid osmotic pressure (COP) or oncotic pressure of the plasma proteins and has a value of approximately 25 mmHg at the start of the glomerular capillaries. The COP gradually rises along the length of the capillary, as water and salts move out of the blood, so increasing the effective concentration of the plasma proteins. By approximately one-third along the length of the glomerular capillary, the COP has risen to approximately 35 mmHg. In addition, the movement of fluid into the Bowman capsule surrounding the capillaries causes a rise in HP of approximately 10 mmHg in the tubular pressure within this space because the exit into the rest of the nephron is narrow. These two pressures balance the HP so only approximately 20% of the volume of the blood is filtered into the nephron, as shown in Fig. 14.8. Note that in other systemic capillaries, the pressure in the ECF is usually slightly negative (−0.5 mmHg). The HP of the blood draining from the glomerulus is 45 mmHg, as opposed to 12 mmHg in muscle capillaries. This high pressure is needed to drive the blood through the second capillary bed of the peritubular capillaries or through the vasa recta (see Fig. 14.4). The COP of the peritubular blood is also elevated to 30–35 mmHg, which also helps to draw fluid back into the peritubular capillaries. Proteins Proteins are mostly held back by the basement membrane. However, a small percentage is filtered and has to be recovered by the cells of the nephron as the filtrate passes down the renal tubule. This recovery is by the process of receptor-mediated endocytosis so the eventual loss of protein into the urine is small, usually approximately 50–80 mg/24 h. Functions of the proximal convoluted tubule The first segment of the tubular portion of the nephron, the PCT, has four main functions: • It recovers some 70% of glomerular filtrate with respect to the filtered water and electrolytes • It reabsorbs most of the filtered sugars, amino acids, nucleosides, other small non-electrolytes and low-molecular- weight proteins (e.g. retinol-binding proteins, α and β microglobulins) Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 12. 654 The renal system 14 H+ H+ H+ H+ H+ K+ channels Facilitated carriers ‘Uphill’ ‘Downhill’ ATPase Na+ channels Na+ pump K+ K+ K+ Na+ /K+ -ATPase (Na+ pump) Na+ and HCO3 – recovery Na+ Na+ Na+ Na+ Na+ Na+ Na+ Dicarboxylate Dicarboxylate Na+ H+ + HCO3 – H+ H2CO3 H2CO3 H2CO3 H2CO3 Na+ Na+ Na+ , K+ , Cl– 3HCO3 – HCO3 – HCO3 – H+ HCO3 – HCO3 –, sugars, amino acids Amino acid (SGLT) Amino acid Sugar GLUT series Carbonic anhydrase Sugar Glomerular filtrate Cl– PAH– A– PAH– Cl– Aquaporin 1 Basolateral face Early proximal convoluted tubule Late proximal convoluted tubule Secretion of organic acids Middle proximal convoluted tubule Na+ -dependent uptake of sugars/amino acids Peritubular capillary Aquaporin 1 Renal tubule Leaky tight junctions Carbonic anhydrase Leaky tight junctions CO2 + H2O CO2 + H2O CO2 CO2 H2O H2O, Cl– H2O, Cl– Cl– H2O Cl– H2O H2O H2O B C D E A Fig. 14.9 Functions of the proximal convoluted tubule (PCT). (A) The glomerular capillaries filter all small ions, sugars and amino acids into the tubule at a rate related to their plasma concentrations and the GFR. (B) Filtered Na+ is recovered in exchange for H+ ions and by ATPase-dependent H+ transport. (C) In the middle PCT, sugars and amino acids are recovered by a Na+ -dependent uptake into the cells of the PCT, then moved into the blood by facilitated downhill carriers, such as the GLUT series. (D) In the late PCT, Na+ is recovered by Na+ channels. (E) The transport pathway for organic anion secretion. See text for further details. GLUT, glucose transporter; PAH, para- aminohippuric acid; SGLT, sodium-coupled glucose transporter. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 13. Renal function 655 14 Some of the H+ ions are fed into the Na+ /H+ antiport process and thus help to recover Na+ ions. The Na+ and the HCO3 – are extruded into the blood on the basolateral side of the cell by the Na+ /K+ -ATPase and by a Na HCO + − 3 3 carrier (see Fig. 14.9B). These processes recover the filtered HCO3 − and approximately 30% of the filtered Na+ water will osmotically accompany the process, so aiding the fluid and ionic balance. Inhibition of carbonic anhydrase activity thus promotes the excretion of Na+ and water (see also Ch. 4). Acetazolamide is a carbonic anhydrase inhibitor. Water As ions are moved into the ECF on the blood side of the proximal tubular epithelium, both between cells via the ‘leaky’ tight junctions and into the basal infoldings, osmotic forces are generated which draw water through the cell and across the tight junctions (see Fig. 14.9). The passage of water through the lipid bilayer of the cell membranes has been something of a puzzle. The PCT recovers some 67% of 180 L of the glomerular filtrate, which is approximately 120 L of fluid being recovered over 24 hours. Although the tight junctions between the cells can be classified as moderately ‘leaky’, the total surface area offered by this paracellular route between the cells would be inadequate to explain this vast movement of water. In addition, because water molecules are partly polar and have a negative charge, it is difficult to envisage that this molecule could pass through a lipid bilayer. Aquaporins A chance finding from work on the protein content of the red cell membrane identified a special class of proteins – the AQPs. The AQPs are membrane-spanning proteins with the ability to form a specific channel for water through the cell membranes. Approximately 10 classes of aquaporins have been identified, with AQP1 being most prevalent on both sides of the cells of the PCT, which explains the unexpected high water permeability of this tissue (see Fig. 14.9). These molecules allow the osmotic gradient created by the movement of various electrolytes and non-electrolytes to exert a much greater force than could be predicted, and permit a relatively low expenditure of energy for the vast movement of fluid. The location of other AQPs, especially AQP2, which can be added to the luminal side of the CD cells under the influence of ADH, will be discussed later. Peritubular capillaries The PCT and the DCT are enveloped in a dense capillary network, the peritubular capillaries (see Fig. 14.4). The recovery of fluid into these capillaries is further aided by the raised COP of 30–35 mmHg of the blood draining from the glomerulus. This also draws water, salts and other molecules into the blood by the Starling mechanism so that by the time this blood passes into the veins, it has a normal COP of 25 mmHg. Sugars, amino acids and other small organic molecules Sugars, amino acids and other small molecules are recovered from the glomerular filtrate by sodium-dependent carriers found on the luminal side of the PCT cell wall (see Fig. 14.9C). Each of these carriers has a special site for the binding of Na+ and a site for a specific molecular species. There are several carriers for sugars (Na+ -coupled glucose transporter (SGLT)), five for amino acids, others for ions and many nutrients, each of which are specific for their own molecule. Once both sites are occupied, the carrier undergoes transformation and the Na+ and the other molecule on the carrier are now transferred of sodium out of the cell, and a gradient in the opposite direction for K+ , creates a potential energy gradient across the cell wall that can be used to recover many substances from the glomerular filtrate. Carrier proteins In the membranes of all epithelial cells are a number of carrier proteins which can move ions across the cell walls on either the lumen or the blood side of the cell. These carriers use the potential energy of the gradients of Na+ or K+ ions set up by the sodium pump to move ions either both in the same direction or one goes ‘out’ and the other comes ‘in’. This arrangement maintains the balance of positive and negative charges across the cell wall, i.e. • A positive ion and negative ion go out together (symport or co-transport) or • A positive ion goes ‘out’ in exchange for a positive ion coming ‘in’ (antiport or countertransport). The arrangement of these carriers is also different on the two sides of the cell and often certain ions, such as K+ , are recirculated, being carried into the cell by one carrier and then passing back out again either via an ion selective channel or on another carrier. The overall effect of these carriers is to recover most of the filtered ions, as well as sugars and amino acids, from the tubular fluid back to the blood (see Fig. 14.9B). Ion channels There are also membrane-spanning proteins which form ion channels that are selective for a specific ion which will move through a pathway formed by the transmembrane loops of protein. Ions move under the influence of the concentration gradient through these channels across the cell wall. Some ion channels can be in an ‘open’ state, which permits the ion to pass through, or a ‘closed’ state when the flow is impeded. These changes in opened or closed state, called ‘gating’, can be brought about by variation in the membrane potential or by ligands (chemical factors such as acetylcholine (ACh), cyclic nucleotides or G proteins) (see Ch. 4; see also Fig. 14.9B). Recovery of bicarbonate by the PCT Bicarbonate (HCO3 – ) is filtered at the same concentration as the blood, i.e. 24–26 mM, which represents some 4000 mM/24 h. The first segment of the PCT has cells which exchange Na+ for H+ ions using the Na+ gradient to ‘power’ the process. This is an antiport process by which there is a balance in charge and is a major component in the recovery of filtered Na+ (see Fig. 14.9B). There is also an H+ -ATPase–dependent process in this section which secretes the H+ ions into the tubule, but it is only a small part of the process and reduces the pH by the end of the PCT to 6.7. The H+ produced by these two processes reacts with the filtered HCO3 – ions to form carbonic acid (H2CO3), which immediately dissociates non-enzymically to form CO2 and H2O (see also Ch. 3). The CO2, being lipid soluble, crosses the lumen side of the cell membrane where the enzyme carbonic anhydrase is present, both bound to the cell wall and in the cytoplasm. In the cell, carbonic anhydrase catalyses the formation of H2CO3 from CO2 and H2O, speeding up the reaction many-fold, so that H2CO3 rapidly forms inside the cell, which again dissociates to form H+ ions and HCO3 – ions (see Fig. 14.9B). CO H O H CO H HCO 2 2 2 3 3 + + + − Most of the bicarbonate is thus reabsorbed, and the H+ ions are excreted in the urine. This is an important process in the renal control of acid–base balance (see later and also Chs 1 and 3). Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 14. 656 The renal system 14 In this region, there are also Na+ channels which allow Na+ to enter the cell and be recovered into the blood by the Na+ /K+ -ATPase. This would produce a large potential difference, but Cl− ions pass through the leaky tight junctions into the intracellular spaces and balance the Na+ ion charge. Water accompanies these processes, so water and salt are recovered (see Fig. 14.9). Secretion of organic anions and cations Renal tubules can secrete a wide variety of toxic metabolites, both ingested in the diet and produced as by-products of metabolism, including drugs. These are often organic lipid-soluble anions and cations that can cross the cell membrane into the cell. These metabolites could accumulate in the cytoplasm, requiring a specific system of transport to eliminate the molecules from the circulation. Organic anion transport Organic anions are mostly weak aromatic and aliphatic organic acids, with pKs generally of less than 7. The transporter systems to eliminate organic anions have a wide substrate specificity. At the pH of blood (7.4), these molecules are anions, whereas in the acid pH of the urine, they become undissociated and lipid soluble. The renal tubules are able to secrete these compounds into the lumen so the urinary concentration of these molecules is higher than in the plasma. This is a basis for measuring renal plasma flow by the clearance method described later. Although this secretory mechanism is an advantage for the elimination of unwanted molecules, the broad specificity of the process means that many drug molecules will also be excreted. For example, this was a major problem with penicillin when the bulk of the administered dose was lost into the urine. Probenecid was found to competitively inhibit the secretion of penicillin, so that administration of probenecid together with penicillin maintained the plasma level of the antibiotic (see Ch. 4). Probenecid inhibits organic anion transporters. By the use of coloured organic acids, the site of secretion was identified as the second S2 segment of proximal tubules. The mechanism of PCT anion secretion is shown in Fig. 14.9E and some examples of typical compounds are given in Table 14.2. The SLC22A gene family codes for organic anion transporter (OAT) proteins. The OAT family plays the central role in renal organic anion transport. OAT1, OAT3, OAT4 and URAT1 are expressed in the proximal tubular cells of the kidneys. OAT1 and OAT3 mediate uptake of a wide range of relatively small and hydrophilic organic anions from plasma. URAT1 transports those organic anions from the cytoplasm of the proximal tubular cells into the lumen of the nephron. Other known substrates of OAT1 include para-aminohippurate (PAH), into the cell. This process is termed co-transport and although it does not use energy directly, it does again use the steep gradient for sodium across the cell wall which has been generated by the Na+ pump on the opposite side of the cell to ‘power’ the entry of the non-electrolyte ‘up’ their concentration gradient (see Fig. 14.9C). This is secondary active transport (see also Chs 2 and 4). The Na+ -dependent SGLT co-transport carriers will move their sugar molecules against a concentration gradient. In the first part of the PCT, there are SGLT2 carriers, which have a low affinity for glucose, so they will work when there is a high sugar content in the lumen. In the later PCT segment, where the concentration of sugar is low, SGLT1 carriers, which have a high affinity for glucose, will move the sugar against a steep concentration gradient to recover molecules from the filtrate back into the blood. As these processes depend on a finite number of carriers in the cell wall, a sudden large excess of a particular molecule present in the blood will increase the amount filtered into the tubule and cause all the sites to become occupied. When this occurs, the process is said to be saturated; the molecules are not fully recovered by the PCT, and will appear in the urine. This condition is seen in diabetes mellitus when glucose appears in the urine (glycosuria), leading to an osmotic diuresis (see also Ch. 3). Facilitated carriers Once inside the PCT cell wall, there are other carriers on the blood side for sugars and amino acids called facilitated carriers. This is a type of secondary active transport (see Chs 2 and 3). For sugars, these are the GLUT series, with other series for amino acids, ions and other nutrients. These types of carrier move the non-electrolytes only down their concentration gradient into the ECF and then by diffusion into the blood. This type of carrier can also work in the opposite direction and carry sugars, amino acids and other molecules from the blood into the cell when the concentration gradient is reversed (see Fig. 14.9C). Sodium and chloride The initial recovery of Na+ is coupled to the Na+ /H+ antiporter which in turn is dependent on HCO3 – in the tubule to generate the H+ ions. The first third of the PCT recovers most of the HCO3 – ions, so that when its concentration in the tubular fluid falls, the recovery of Na+ slows. However, to overcome this problem, the next section of the tubule has a Cl HCO − − 3 coupled exchange process, so here the HCO3 – ions are returned to the tubular fluid to help recover Cl− ions. Now, the H+ /Na+ antiport has more HCO3 – to react with to help the recovery of more Na+ ions, as well as the Cl− (see Fig. 14.9D). Table 14.2 Representative compounds secreted by the renal organic anion and cation transport systems Anions Cations Endogenous compounds Drugs Endogenous compounds Drugs Amino acids Benzoate Bile salts Cyclic AMP Long-chain fatty acids Hippurate Hydroxybenzoates Hydroxyindoleacetic acid Oxalate Prostaglandins Urate Acetazolamide Cephalothin Chlorothiazide Ethacrynic acid Furosemide Indometacin Penicillin G Probenecid Saccharin Salicylate Acetylcholine Epinephrine (adrenaline) Choline Creatinine Dopamine Histamine 5-Hydroxytryptamine Norepinephrine (noradrenaline) N-Methylnicotinamide Serotonin Thiamine Amiloride Amprolium Atropine Cimetidine Hexamethonium Mecamylamine Morphine Neostigmine Paraquat Quinine Tetra-ethylammonium Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 15. Renal function 657 14 Nephrotoxicity Some drugs can damage the cells of the nephron as they accumulate within the cytoplasm and this nephrotoxicity is related to their uptake in the tubule cells by these processes and the lower ability of the cells to transport these drugs into the urine. Neonates are protected from this damage as their uptake transport system is poorly developed at this stage. Organic cation transport Many organic cations in the blood are excreted by the kidney where a series of organic cation transporters (OCT1–3) are expressed. These are electrogenic organic cation transporters with a broad specificity, which suggests they are involved in the first step of secretion of the compounds, moving the molecules across the basolateral membrane. The exit across the brush border is accompanied by an organic cation/ H+ antiporter acting down the lumen/cell H+ gradient established by Na+ /H+ exchange. Table 14.2 gives some examples of these compounds (Clinical box 14.5). However, the detailed mechanism of their transport has not been well characterised and work is still in progress, although the structure of OAT and OCT has been identified. Renal function tests The symptoms of renal failure can masquerade under an amazing variety of clinical conditions, so it is essential to be able to screen patients using simple low-cost techniques before proceeding to more complex and expensive diagnostic tests. Blood and urine tests In routine blood tests, raised levels of urea and creatinine are the first signs of possible renal problems, which can be confirmed by testing the urine, where increased levels of protein and tubular debris after centrifugation can often be found. Measurement of the urinary volume over 24 hours and the ability to form concentrated urine, when water intake is restricted, can also be used and will identify both problems within the kidney and of the water control mechanisms. Relative density of urine This can be measured by a number of methods. Osmolality Osmolality of urine depends on the number of particles present and can be measured directly by the depression of freezing point with an osmometer. It is significantly increased in glycosuria but not influenced by temperature or protein. Specific gravity A more simple guide is to measure the specific gravity using a hydrometer, which compares the specific gravity of the test fluid with the specific gravity of pure water: Specific gravity density of test fluid density of water = In pure water, the float will sink to a level of 1.000 on the hydrometer. With increasing density of the test solution, the scale on the dicarboxylates, prostaglandins, cyclic nucleotides, urate, folate, diuretics, angiotensin-converting-enzyme (ACE) inhibitors, antiviral agents, β-lactam antibiotics, antineoplastics, mycotoxins, sulphate conjugates, glucuronide conjugates, cysteine conjugates, ochratoxin A, non-steroidal anti-inflammatory drugs (NSAIDs) and uraemic toxins. Para-aminohippuric acid Hippurate is the prime organic anion secreted by the kidney and approximately 1 g/day is excreted in the urine. PAH is an amide derivative of the amino acid glycine and para-aminobenzoic acid. It is a model substrate for this process and on the basolateral side of the cell there is a two-stage process (see Fig. 14.9E). The first step is the entry of dicarboxylates (α-ketoglutarate and glutarate) co-transported with sodium. The ubiquitous Na+ pump maintains the low Na+ in the cell, which enables this co-transport to proceed. Then the intracellular dicarboxylate exchanges with an organic anion, in this case PAH, which moves into the cell on the apical (luminal) side of the cell. The PAH is then exported into the lumen on the basolateral side in exchange for another anion, such as chloride, urate or hydroxyl ions, so the PCT can concentrate PAH to a much higher level than in plasma (200–300 times). In plasma (pH 7.4), PAH with a pK of 3.8 is 99% ionised, whereas in urine with a pH of 4.5, 83% is ionised. The non-ionised fraction can diffuse through the lipid cell membrane, so making the urine more acidic and increasing the secretion of PAH into the urine. This leads to a complete clearance of PAH on a single passage through the kidney. In contrast, the excretion of some molecules, such as probenecid, phenobarbital and salicylic acid, can be increased by urinary alkalisation (see Ch. 4). This mechanism is a balance between the pKa, the partition coefficient (Kp) and the pH, so that the excretion of some drugs, such as barbital and urate, are not increased by urinary alkalisation. PAH has been found to enhance the rate of excretion of water, Na+ , K+ and HPO2 − and this is seen in patients receiving massive doses of carbenicillin. This also occurs in starvation where there are increased organic acids derived from fat metabolism (see Ch. 3). PAH is useful for the measurement of renal plasma flow (RPF) because it is secreted primarily by the renal tubules; only 20%–30% is filtered by the glomerulus. PAH is completely filtered from plasma in the nephron and not reabsorbed by the tubules, in a manner identical to inulin. The clearance of PAH is reflective only of RPF to portions of the kidney that deal with urine formation, and thus underestimates actual RPF by approximately 10%. PAH and drug dosage When the GFR falls to 10% or less of normal, hippurate accumulates in the blood and competes for the binding of several drugs, such as salicylate, phenytoin, sulfonamides and furosemide. There will be an increased level of the unbound drug in the plasma with a greater therapeutic effect for a given dose. In contrast, when such patients are dialysed, the hippurate is removed so the protein binding now increases and the therapeutic effect of some drugs will be decreased and the dose must be adjusted to allow for this effect. Efflux transporters and drugs Efflux transporters are active transport systems that extrude drugs out of cells (see Ch. 4). They require energy to function. These efflux transporters have a broad range of specificity so can handle many molecules. The transport proteins can also be induced or upregulated, thereby accounting for the failure of some drugs to continue to act with repeated doses. This effect explains why some anti-cancer agents fail to work after the initial positive response, and may contribute to bacterial multidrug resistance. Clinical box 14.5 Furosemide Furosemide is bound to plasma proteins and is not filtered so only passes into the tubule by these secretion processes. Indometacin, aspirin and probenecid compete with this step, so reduce the diuretic action of this drug, although they do displace it from the protein binding which increases entry into the tubule by filtration (see Ch. 4). Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 16. 658 The renal system 14 Proteinuria Physiologic proteinuria does not exceed 150 mg/24 h for adults and 140 mg/m2 in children. A urine dipstick is highly sensitive in detecting albumin (limit approximately 0.2 g/L). A dipstick allows rough quantification of urine from 0 to ++++. A urine dipstick does not identify globulin fraction of protein and can be negative in Bence Jones proteinuria (free immunoglobulin light chains in urine). Protein quantification is expressed as g/L or g/24 h. Twenty-four- hour urine collections are time consuming and practically difficult; hence an alternative measure, the protein:creatinine ratio (PCR) on a random urine sample, has now been validated, widely accepted and used. A first or early morning urine sample is more accurate (Clinical box 14.6). Proteinuria may be increased by a factor of 2–3 times by strenuous exercise or fever. Other causes of transient proteinuria include urinary tract infection, vaginal mucus, orthostatic proteinuria (occurs after patient has been upright for some time and is not found in early morning urine – this condition is uncommon in patients over 30 years old) and pregnancy. Causes of persistent proteinuria include: • Primary renal disease – this may be glomerular (e.g. glomerulonephritis) or tubular • Secondary renal disease – diabetes mellitus, hypertension, connective tissue diseases, vasculitis, amyloidosis, myeloma, congestive cardiac failure. Renal handling of molecules Simple estimates of renal function can be derived from changes in the way that the kidney handles molecules. The kidney can handle molecules in three ways: • First, a molecule can be simply filtered and then passed unchanged into the urine (Fig. 14.10A) • Second, it can be filtered then reabsorbed as it passes through the PCT, so the final concentration in the urine is less than in plasma (see Fig. 14.10B) • Finally, a molecule can be filtered and then more can be added to the urine by secretion in the PCT, making the concentration in urine higher than in plasma (see Fig. 14.10C). These mechanisms can be studied by the use of a technique called clearance. Water being abstracted from the tubule will alter the concentration in the urine but its effect will depend on the transport of each molecule. Even molecules which are only filtered will be concentrated in the urine by this process. Renal clearance The clearance of a molecule is defined as ‘volume of plasma cleared of that molecule per minute’. Because no molecule is fully cleared hydrometer will float to a higher level, which is related to the ionic content. Plasma has a specific gravity of 1.010 (285 mOsm). Urine can vary from a specific gravity of 1.035 (1400 mOsm), the most concentrated and dark, down to 1.005 (50 mOsm), the most dilute and pale. Note, however, because the density of fluids varies with temperature and hot fluids are less dense, it is essential to allow the urine to cool to the calibrated temperature of the hydrometer. In hot environments, it is necessary to ensure that the hydrometer used is calibrated to the range of climatic temperature. Although not frequently performed, measurement of the specific gravity of a urine specimen can give an indication of the efficiency of the renal control of fluid balance mechanisms (see later). If the specific gravity is 1.035, glycosuria should be considered; when it is 1.040, this indicates the presence of extrinsic osmotic agents (e.g. contrast) Refractometry This is based on measurement of refractory index, which depends on the size and weight of solutes and correlates well with osmolality. Dry chemistry Dry chemistry is incorporated into dipsticks and detects the presence of cations and protons by colour change. Analysing urine The history of urinalysis can be traced back to ancient Egypt, where polyuria and haematuria were mentioned in medical papyri, and, by 400 BC, Hippocrates had observed the changes to the colour and odour of urine and its relation to disease. Healthy urine should be clear and a straw colour. Other colours can indicate the presence of drugs, blood haemoglobin or bilirubin. The odour of urine can reflect chemical conditions: a fruity odour or acetone in diabetes mellitus; a musty odour indicates hepatic disease; and ingestion of various dietary constituents, such as garlic, gives other odours. The various penicillins are excreted via the kidney and can impart a strong odour to the urine. By the end of the 18th century, the chemistry of urinalysis had progressed to various spot tests and then to test papers, which identify specific constituents present in the urine. Table 14.3 sets out the range of tests commonly in use and their purposes. Specialised spectrophotometers can be used to quantify the concentration of various constituents in urine. Table 14.3 Urine tests and purposes Range of tests Uses Specific gravity To monitor drugs in athletes pH 4.8–7.4 Acid–base disturbances Leucocytes Inflammatory disease of the kidney Nitrite Presence of bacteria Protein (albumin) Renal disease Glucose Diabetes mellitus renal threshold 8.3–10 mM Ketones Increased fat degradation, gastrointestinal infection in diabetes mellitus Urobilinogen Liver disease or increased haemolysis Bilirubin Liver damage, hepatitis, cirrhosis Blood Renal and post-renal bleeding Clinical box 14.6 Interpretation of urine protein to urine creatinine ratio Child under age 2 years Normal ratio 0.5 Adults and children over age 2 years Normal ratio 2 mg/mmol correlates with 0.2 g protein/day (i.e. 2 × 10 mg protein/day) Nephrotic range 3.5 (correlates with 3.5 g protein/day) Interpretation of urine albumin to creatinine ratio (ACR) Microalbuminuria: ACR of 2.5–30 mg/mmol (men) and 3.5 to 30 mg/ mmol (women) Macroalbuminuria: ACR of 30 mg/mmol (this is approximately equivalent to PCR 50 mg/mmol, or a urinary protein excretion 0.5 g/24 h). Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 17. Renal function 659 14 as a bolus. Because this molecule is filtered, the level in the blood will rise to a peak value then fall with time, as shown in Fig. 14.11A. The urine is collected for a set period and the concentration of ‘inulin’ in the urine and the volume formed in mL/min (UinV) can be easily determined. The problem, however, remains to find a value of plasma which reflects the average concentration for the period (Pin). Various methods have been used to obtain a mean of this value of plasma concentration, including infusing a dilute ‘inulin’ solution to balance the renal loss as shown by the dotted line in Fig. 14.11A, or calculating the area under the curve, but errors in this value have a large effect on the calculation of Cin. Note that whatever level of ‘inulin’ appears in the blood, the same level is filtered into the urine, so the relationship becomes a straight line with a slope of 45 degrees. Fig. 14.11B shows that the clearance (Cin) of this molecule is independent of the blood level. Values of ‘inulin’ clearance are in the range of 125 ± 30 mL/min for normal male subjects. This is the value taken as ‘normal’ GFR. Again, note that the range of Cin in normal subjects is quite large, i.e. ± 30 of the population mean value of 125, and depends on body size, age and sex. Females have a lower value than males with a mean of approximately 90 mL/min being taken as normal. Infants do not achieve adult GFR until they are approximately 4 years old and cannot fully concentrate their urine until the kidney has matured. Renal function begins to decrease with increasing age (after the age of approximately 65–70 years). Creatinine clearance Creatinine is a breakdown product of muscle metabolism (creatine phosphate) and is usually produced at a constant rate by the body (depending on the muscle mass), so has a constant level in the blood. (Note: creatinine is a di-amino acid and must not be confused with creatine.) This molecule was thought to be a good marker for GFR because it is endogenous, i.e. occurs naturally in the circulation, and the plasma concentration (Pcr) is relatively constant. Serum by the kidney, it is more a concept than a reality. It is a simple way of quantifying the handling by the nephron of various types of molecules. The most useful renal function which can be derived from a clearance measurement is the GFR. If the renal excretion (Ux × V), i.e. the concentration of a molecule in mM in the urine (Ux) multiplied by the volume of urine formed per minute (V), is measured and divided by the concentration of the molecule in plasma (Px), we can gain some idea of how the nephron is handling the molecule. This is termed the clearance of a molecule. The clearance of molecule x is expressed as: C U V P x x x = × ( ) where: Ux = the concentration in the urine in mM Px = the concentration in plasma in mM V = the volume of urine formed per min, i.e. mL/min. The unit of clearance is mL/min. Clearance of molecules that are only filtered If a molecule is filtered and then passes unchanged into the urine, the clearance of such a molecule is an index of the effective GFR of all the nephrons. The concentration of such a molecule will be raised in the urine, as it will remain trapped in the tubule after filtration, where some 99% of water and other constituents of the filtrate are mostly recovered as they pass along the tubule. ‘Inulin’ clearance as an index of GFR In the past, ‘inulin’ (a plant starch) of MW 5200, was used for testing renal clearance as a molecule that is filtered and then passed unchanged into the urine. ‘Inulin’ is now no longer available and polyfructans are used instead. Inulin clearance, however, is still a benchmark against which all other methods are judged, and the term ‘inulin clearance’ is still used. To perform a clearance test with ‘inulin’ (Cin), the bladder is first emptied and the ‘inulin’ injected intravenously Filtration only Reabsorption of water and salts A Filtration plus secretion C Filtration plus reabsorption B Fig. 14.10 Renal handling of molecules. (A) Molecules can be filtered only and not reabsorbed or secreted, but will still have an increased concentration in the urine due to the fact that fluid is recovered along the nephron. (B) Molecules that are filtered and reabsorbed will have a very low concentration in the urine. (C) Molecules that are filtered and secreted will have an elevated concentration in the urine and very low levels in the blood draining from the nephron. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 18. 660 The renal system 14 Urea clearance Urea is also a natural product, but it is reabsorbed and recirculated in the kidney so it gives values three-fifths of GFR; urea clearance, Cu, is approximately 80 mL/min. The ratio of Ccr to Cu can be used to reduce variation. Cu does, however, vary with water intake, so if the water intake is low even more is reabsorbed and the value of Cu falls. Current methods for measuring renal clearance (half-life) Fig. 14.11A shows that the level of ‘inulin’ in plasma when injected as a bolus decreases with time as it is filtered through the kidney. If the kidney is damaged and GFR is depressed, the rate of ‘inulin’ filtration with time will be less, and the blood level will fall more slowly (hatched line in Fig. 14.11A). This fact can then be used as an indication of renal function. An easily measured molecule, such as 51 Cr-EDTA (ethylene diamine tetra-acetic acid, MW 300) is given as a bolus and then the blood level followed for a period by taking serial blood samples. EDTA is a molecule which strongly binds to chromium (Cr). 51 Cr is an isotope which emits gamma rays and is easy to count. Initially the counts in plasma samples will rapidly rise to a maximum. Then decrease over a period. The time can then be taken for the isotope level to fall to half of the maximum, which is the half-life (t1/2) for healthy subjects (see Fig. 14.11A). With the progressive deterioration of renal function the t1/2 gradually increases, indicating loss of filtration capacity, and reflects the number of nephrons which are still functional. This method is quick and cheap and has largely replaced other clearance methods. It has limited clinical use apart from use in estimation of GFR in a potential kidney donor. It can be used in certain groups of renal failure patients with unreliable estimated GFR, e.g. amputees and those with extremes of body weight. Clearance of molecules that are filtered and reabsorbed Clearance of molecules that are filtered and reabsorbed is not used as a test, but gives an idea of one of the most important functions of the kidney (see Fig. 14.10A). Molecules such as glucose have a very low clearance (0.2 mL/min) because they are actively reabsorbed. The normal plasma level is 4–5 mM and only tiny amounts are found in the urine of normal subjects; however, as the blood level of glucose increases a point is reached – the renal threshold – when glucose appears in the urine at the same rate as ‘inulin’, etc. This is the result of the saturation of all the carrier sites; i.e. there is a limited number of sites for uptake and, if there is a large excess of glucose in the blood, they all become occupied and now the molecule passes through the PCT, as if it was only filtered. As can be seen from Fig. 14.12A, once the threshold is reached the behaviour of glucose parallels that of a molecule which is only filtered, such as creatinine. The threshold is not a sharp point but has a ‘splay’ as different nephrons have a slightly different value for threshold. The threshold is approximately 8–10 mM in a healthy subject. After a meal with a high sugar content, this value is exceeded for a short while, which explains why a small amount of glucose is found in the urine of healthy people. The displacement of the glucose response, compared to that of a molecule that is only filtered, is expressed as the tubular maximum, Tm, and represents the total capacity of the kidney to reabsorb glucose. With diabetes mellitus, glucose in the urine is common due to the lack of insulin and high levels of glucose in the plasma, but as the disease progresses, microvascular complications lead to renal damage and a much elevated threshold for glucose. Now, little glucose appears in urine, although the plasma levels may be 20 mM or greater (normal 4–5 mM). This is why urine testing for glucose in diabetes mellitus is currently no longer used and has creatinine is affected by the level of GFR and by factors independent of GFR, including age, gender, race, body size, diet, certain drugs and laboratory analytical methods. This makes it a poor marker of true renal function. Creatinine clearance, Ccr, gives values close to ‘inulin’, i.e. 125 mL/ min, although there is a small component of secretion. However, the error caused by the raised value of urinary creatinine, Ucr, is balanced by a plasma chromogen which raises the value of Pcr, so the errors cancel. Serum creatinine levels may vary from one laboratory to another, depending on the method used to measure. It is usually 60–80 µmol/L in males (higher muscle mass) and 40–60 µmol/L in females (lesser muscle mass). It is simple to measure and is elevated only in renal failure. Creatinine is mostly filtered but is secreted by proximal tubules as well. Maximum Time (minutes) Blood level (mg) Inulin or creatinine Urine excretion (mg/min) Renal failure ‘Inulin’ level in blood IV bolus t 1 2 / t 1 2 / Ideal level if given IV infusion 0 0 5 10 2 4 6 8 10 A B Fig. 14.11 Inulin clearance. (A) Molecules that are filtered only, such as ‘inulin’, can be re-used as an index of GFR. If ‘inulin’ is given as a bolus into the plasma, the level rises rapidly to a maximum, then ‘falls’ off with time as it is filtered. In renal failure, the rate of ‘fall’ is much reduced and by measuring the time to reach a value that was half the maximum, an index of renal function can be derived from the fall off in plasma level. To get a true reading, plasma level ‘inulin’ would have to be infused at a rate to match the filtered loss; as this is not known, this is difficult to achieve. (B) As the urine excretion matches the blood level, it indicates that this molecule is filtered only. IV, intravenous. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 19. Renal function 661 14 Use of clearance methods to assess renal function RBF is approximately 1.2–1.4 L/min, i.e. one-fifth of cardiac output. Thus we can then, by relatively simple methods, obtain the effective GFR and RBF using clearance techniques. The ratio of GFR to RBF is called the filtration fraction (FF) and is approximately 0.10–0.15; i.e. 20% of the plasma passing through the kidney is filtered into the nephron. FF GFR RBF in PAH = = C C With the large number of patients with possible renal failure, it is essential to take a detailed history and to be able to screen patients using blood tests and simple low-cost techniques before proceeding to those which are more complicated and expensive. Advanced clinical tests If signs of renal failure are detected on simple testing, a variety of diagnostic tests can then be used to identify the site of the renal dysfunction, e.g. obstruction, by imaging, ultrasound, nuclear medical imaging, computed tomography scans or the gamma camera. Renal control of fluid balance The mechanisms which balance fluid intake with fluid loss are more precise than those for acid–base and electrolyte balance. The control of these processes resides in an osmoreceptive complex located in the hypothalamus (Fig. 14.13A) and comprises the subfornical organ, the organum vasculosum of the lamina terminalis and the median pre-optic nucleus, all of which input onto the magnocellular neurons of the supraoptic (SO) and paraventricular nuclei (PVN). The SO and PVN neurons can act both as osmoreceptors and also synthesise two peptide hormones – vasopressin and the reproductive hormone oxytocin. Vasopressin Vasopressin (or ADH) is a nonapeptide (nine amino acids) that has two cysteine residues in positions 1 and 6, linked by a disulphide bridge (Fig. 14.13B). It has a short half-life of 15–20 minutes. ADHs evolved very early in evolution and are found in most animal species. In mammals, vasopressin is released from the posterior pituitary in response to a small rise in the osmotic pressure of the plasma usually caused by an increased rate of water loss. There is an inverse relationship between the plasma vasopressin level and the osmolarity of the urine (Fig. 14.13C). Note, however, that although the volume and concentration of urine vary, the net loss of solute does not, and is maintained constant for a given period. There is thus a mechanism by which the water balance is separated from that of solute. Water intake is regulated to maintain a physiological serum osmolality of 285–290 mOsm/kg. Normally, the level of vasopressin in the plasma is in the range 2–4 pg/mL and is rapidly increased as the plasma osmolarity changes. Osmotic threshold for vasopressin release is 280–290 mOsm/kg. Thirst plays an important role in water balance and only a 2%–3% change in plasma osmolarity can produce a strong desire to drink water. This precise matching of the plasma vasopressin level to osmolarity is the central mechanism of water homeostasis (Fig. 14.14A, B). The normal response to a fall in water intake is a rise in plasma osmolarity, and within minutes, an increase in the plasma vasopressin level. Once vasopressin has been synthesised by neurons of the SO and PVN, it is then attached to the transport protein neurophysin as granules, which are then rapidly transported within 30 minutes been replaced by measuring the glucose level in blood with various reagent strips which give an accurate colour change depending on the level of glucose in the blood. This colour is measured by various meters which now can respond in approximately 10 seconds or less. Clearance of molecules that are filtered and secreted Some molecules are both filtered and secreted, such as organic acids and bases, and molecules that are lipid soluble or are toxic and have been converted into glucuronides by the liver (see Ch. 4). With these compounds, more appears in the urine than in the blood as they are secreted into the tubule. As with sugars, this process saturates because there is a finite number of carriers. The process has both a threshold and Tm. The values for clearance of molecules such as PAH are in the region of 650–700 mL/min. Because these compounds are both filtered and secreted, the amount remaining in the blood leaving the nephron is very low and can give an indication of the RPF, i.e. the clearance of PAH, CPAH = RPF. Because the PAH is only present in the plasma, the renal blood flow (RBF) can then be calculated by correction with the haematocrit (Hct), i.e. RBF Hct PAH = − C 1 0 0 2.5 7.5 0 5 5 15 Tm Tm Threshold Splay 10 0 1 2 3 4 Filtration only Filtration only Filtration plus secretion Filtration plus reabsorption Urine excretion (mM/min) Urine excretion (mM/min) Blood level of glucose (mM) Blood level of PAH (mM) 10 15 20 5 5 10 A B Fig. 14.12 Clearance of molecules that are filtered and reabsorbed, such as glucose. (A) Initially no glucose appears in the urine, as it is reabsorbed; however, once the plasma level exceeds the renal threshold, glucose is filtered into the urine. This point is related to the availability of carriers to recover the filtered glucose, which eventually becomes saturated. Different nephrons vary in their saturation level so there is a splay in the threshold level. Once the threshold is exceeded, glucose is just filtered and the line is parallel to that of molecules which are only filtered. The displacement of this line gives an index of the tubular maximum, Tm, for the recovery of glucose. (B) For molecules which are filtered and secreted, the level in the urine is higher than in the plasma. This process will also saturate in most cases. Molecules such as para-aminohippuric acid (PAH) are virtually cleared from the plasma by these processes. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 20. 662 The renal system 14 is steep, and in addition the gradient, can be altered by the fluid volume of the ECF, which will increase or decrease the sensitivity of the response (see Fig. 14.13). Vasopressin can also be released in response to a fall in blood pressure, but the change in blood pressure must be of a much larger magnitude than that of osmolarity. to the posterior pituitary, down microtubules in the axons of the neurohypophyseal tract; here it is stored prior to release. Bursts of action potentials in these axons of the neurohypophyseal tract, in response to a tiny rise in osmotic pressure, cause the release of vasopressin into the bloodstream. However, the slope of this response Cerebellum Pituitary Paraventricular neurons Osmoreceptors Baroreceptor input Vasomotor centre (medulla oblongata) Vagus and glossopharyngeal nerves Total solute excretion Urine osmolarity Urine flow rate Min Max Max 0 Plasma VP A B C Supraoptic neurons Optic chiasm Anterior lobe Posterior lobe VP S S Cys - Tyr - Phe - Gln - Asn - Cys - Pro - Arg - Gly(NH2) Fig. 14.13 Vasopressin secretion. (A) Anatomy of the hypothalamus and pituitary gland (mid-sagittal section) depicting the pathways of vasopressin (VP) secretion. Also shown are pathways involved in regulating VP secretion. Afferent fibres from the baroreceptors are carried in the vagus and glossopharyngeal nerves. The vasomotor centre includes the solitary tract nucleus. The closed box illustrates an expanded view of the hypothalamus and pituitary gland. (B) The amino acid sequence of vasopressin. (C) Relationship between plasma VP levels and urine osmolarity, urine flow rate and total solute excretion. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.
- 21. Renal function 663 14 0 Normal 260 270 280 290 300 310 Plasma osmolarity (mOsm/kg H2O) Max Plasma VP 10% increase in volume/pressure 10% decrease in volume/pressure A 0 260 270 280 290 300 310 Plasma osmolarity (mOsm/kg H2O) Tubular lumen Capillary COOH ATP AMP Cyclic PKA Inactive PKA Active Adenylate cyclase Protein phosphorylation Vesicles with inactive water channels Active water channels Fusion of vesicles with apical cell membrane VP Max Plasma VP (pg/mL) Plasma VP (pg/mL) 0 –30 –20 –10 0 10 20 % Change in blood volume or pressure Max B C Fig. 14.14 Action of vasopressin. Interaction between osmotic and haemodynamic stimuli for vasopressin (VP) secretion. With decreased blood volume and pressure, the osmotic set point is shifted to lower plasma osmolarity values and the slope is increased. An increase in blood volume and pressure has the opposite effect. (A) Changes in VP secretion in response to plasma osmolarity variation. (B) Plasma VP levels in relation to plasma osmolarity and changes in blood volume or pressure. (C) Cellular action of VP. Descargado para luis eduardo mendoza goez (lmendozag@hotmail.com) en University of Cartagena de ClinicalKey.es por Elsevier en junio 09, 2020. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2020. Elsevier Inc. Todos los derechos reservados.