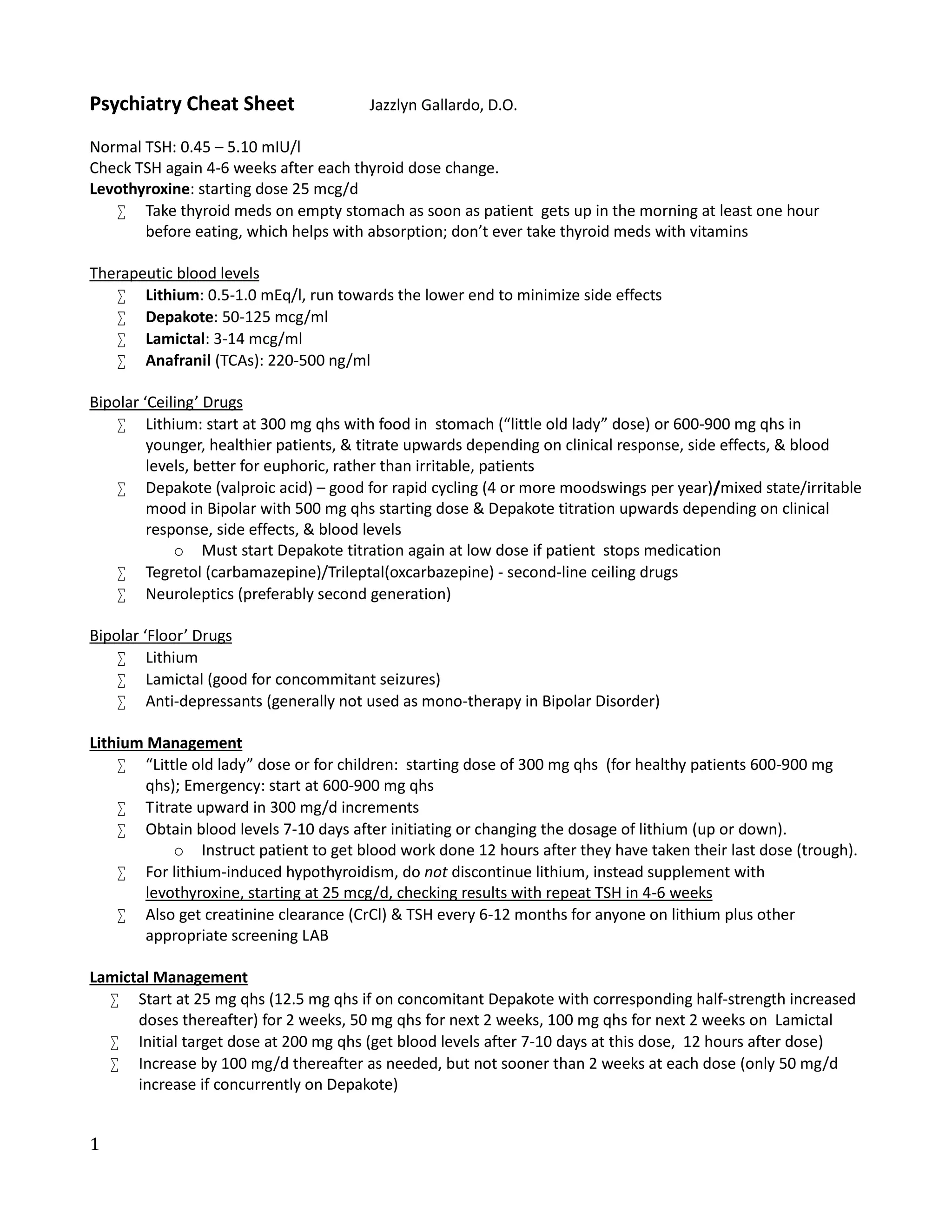
This document provides a summary of medication guidelines for psychiatry. It lists normal thyroid levels and guidelines for adjusting levothyroxine doses. It also outlines therapeutic blood levels, starting doses, and monitoring for medications used to treat bipolar disorder like lithium, Depakote, Lamictal and antidepressants. Additional sections cover medication groups, terminology, pearls and toxicities to consider when prescribing psychiatric medications.