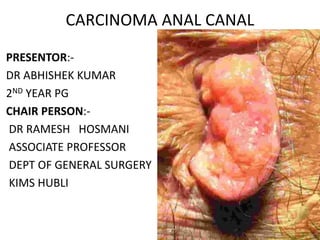
Carcinoma anal canal
- 1. CARCINOMA ANAL CANAL PRESENTOR:- DR ABHISHEK KUMAR 2ND YEAR PG CHAIR PERSON:- DR RAMESH HOSMANI ASSOCIATE PROFESSOR DEPT OF GENERAL SURGERY KIMS HUBLI
- 3. Anatomy
- 5. • The line of fusion of the endodermal and ectodermal parts of anal canal is marked by a line called pectinate line that lies below the anal columns. • This line marks the transition of anal canal lining from simple columnar to stratified squamous epithelium.
- 6. Definition • Surgical : The anal canal is the terminal portion of the intestinal tract it begins at the anorectal junction (the point passing through the levator ani muscles), is about 4 cm long, and terminates at the anal verge. • Anatomical : that extends from the dentate line to the anal verge.
- 7. Anal canal • Begins at ano-rectal junction • Rectal ampulla narrows at ano-rectal junction • From ano-rectal junction canal passes Downwards & Backwards through Pelvic diaphragm • Opens at anal orifice situated in gluteal cleft 4 cms below & in front of tip of coccyx.
- 11. Relations • Anterior : Perineal body In male – bulb of penis & urethra In female – Lower part of post. wall of vagina • Posterior: Ano-coccygeal raphe Fibro-fatty tissue between peri-anal skin & raphe • Lateral: Ischio-rectal fossa and its contents (inferior rectal vessels an pudendal nerve.
- 13. Interior of Anal canal • Divided into 3 areas • 1 Anorectal Ring Upper (15 mm) • 2 Dentate line Intermediate (15 mm) • 3. White line of Hilton Lower (8 mm) • 4.Anal verge
- 14. Hilton’s line • It is a contrast between bluish pink area above and black skin below • The line is represented by inter- sphincteric groove at the lower end of the internal sphincter • Indicates lower end of internal sphincter • Anal intermuscular septum is attached carrying the fibres of levator ani and longitudinal muscle of rectum
- 15. Sphincters of anal canal- Internal sphincter • Involuntary sphincter • Thickening of circular muscle of lower part of rectum • Surrounds upper 3/4th of anal canal • Lower end corresponds with Hilton’s line • Middle corresponds with pectinate line • Externally separated from ext. sphin. Muscle by Conjoint sheath derived from levator ani and longitudinal muscles of rectum • Nerve supply: Sup.Hypogastric & pelvic splanchnic
- 16. External Sphincter • Triple-loop system of Shafik. The top loop arises and inserts on the pubis and is made up of the deep external sphincter and puborectalis. The middle loop attaches to the coccyx (superficial external sphincter). The lower loop inserts in the anterior perianal skin (subcutaneous external sphincter). • Nerve supply:Inf. Rectal br. Of pudendal n, Perineal br. of 4th sacral n.
- 18. •Upper anal canal Via channels around rectum into pelvic and pre aortic nodes •Lower anal canal Below dentate line Inguinal nodes
- 19. Nerve supply Somatic innervation •Pudendal nerve(S2–S4) •Inferior rectal n: sensory &motor to muscles & mucosa below dentate line •Perineal n: sensory & motor to perineal region
- 20. Autonomic innervation •Sympathetics from thoraco-lumbar segments via sup. hypo-gastric plexus& hypogastric nn. •Parasympathetics from S2–S4 (nervi erigentes) •Unite in inf. hypogastric plexus •Distributed to pelvic viscera & sexual organs
- 22. Nerve supply. • Internal sphincter sympathetic (L-5) & parasympathetic nerves (S-2, S-3, and S-4) • External sphincter inferior rectal branch of the pudendal nerve (S-2 ,S-3) the perineal branch of S-4 • Levator ani sacral roots on its pelvic surface (S-2, S-3, and S-4) perineal branch of the pudendal nerve
- 25. Supporting structures in continence.
- 26. Epidemiology How Common Is This Cancer?
- 27. Incidence
- 32. Risk Factors for Anal Cancer Strong Evidence1 • History of receptive anal intercourse • HPV Infection (anogenital warts) • History of cervical, vulvar, or vaginal cancer • More than 10 sexual partners • History of STD • Immunosuppression after solid-organ transplantation Moderately strong evidence1 • Cigarette smoking • Long-term use of corticosteroids • HIV infection Populations in which risk factors are more prevalent have higher incidences of anal cancer.2 Anal intercourse is a risk factor but is not required for anal HPV infection or cancer development in men or women.3 1. Ryan DP NEJM 2000; 342(11):792-800. 2. Daling JR et al. Cancer 2004;101(2):270-280. 3. Goodman MT JID 2010;201:(9)1331-1339.
- 33. HPV 1.Villiers Virology 2004;324:17-27. Most common among HIV+ Men: 6, 16, 18, 31 Vandersnoek et al., 2005 n=286 HIV+ Men HIGH-RISK: 16, 18, 26, 31, 45, 54, 55, 56, 64 INTERMEDIATE-RISK: 33, 35, 39, 52, 58 LOW-RISK: 6, 11, 42, 43, 44
- 34. HPV Infection • High-risk HPV type-16 detected in almost 80-90% cases of SCC anus. (to a lesser extent, types 18, 31, 33, 35, and others.) • 80% of anal cancers demonstrated more than one HPV genotype. • Incidence 15 times higher in homosexual men. • Mostly sexually transmitted, and cancer risk increased in women with history of receptive anal intercourse. • Women with high-grade cervical or vulvar dysplasia are more susceptible to develop anal cancer, as cervical or vulvar HPV infection escalates anal HPV infection risk. Grulich AE, Poynten IM, Machalek DA, et al. The epidemiology of anal cancer. Sex Health 2012;9:504–508. Machalek DA, Poynten M, Jin F, et al. : a systematic review and meta-analysis. Lancet Oncol 2012;13:487–500.
- 37. HIV Infection • Anal cancer incidence in HIV patients is estimated to be twice that of HIV-negative patients. • HIV-positive patients with anal cancer tended to develop earlier recurrences than HIV-negative patients by 20 months, although the median survival ( 34 vs 39 months ) were similar (CHAMP Study). • Highly active antiretroviral therapy (HAART) has resulted in patients with HIV living longer and the development of related malignancies. • In contrast to other HIV-associated malignancies, the incidence of anal cancer has actually risen following implementation of HAART.
- 38. • According to NCI, rise in anal cancer incidence during 1980 to 2005 was predominantly seen in males with HIV, relative to their female counterparts • Among men, incidence rates increased by 3.4% annually overall and by 1.7% annually in men without HIV infection • Among women, anal cancer increased 3.3% annually overall and by 3.3% annually in those without HIV infection. North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD), 1996-2007 Shiels MS, Pfeiffer RM, Chaturvedi AK, et al. Impact of the HIV epidemic on the incidence rates of anal cancer in the United States. J Natl Cancer Inst 2012;104:1591–1598.
- 39. • In a meta analysis of 53 studies, prevalence of both high risk anal HPV subtypes (74 versus 34 percent) and anal cancer (45.9 versus 5.1 per 100,000 men) was significantly higher among HIV positive compared with HIV negative MSM.* • Without controlling for receptive anal intercourse and prior HPV infection, it is difficult to discern the true effect of HIV on the incidence of anal cancer. • It is possible that HIV infection interacts with HPV to predispose to anal cancer(significant immunosuppression (CD4 count below 200/microL)-- increased HPV replication & Infection with more than one type of HPV). *Machalek DA, Poynten M, Jin F, et al. Anal human papillomavirus infection and associated neoplastic lesions in men who have sex with men: a systematic review and metaanalysis. Lancet Oncol 2012; 13:487.
- 40. Treatment Points Specific to HIV+ • Pre-treatment CD4 count predicts outcome & tolerance of chemoradiation1 – CD4 >200 similar to general pop – CD4 <200 sig more toxicity from Tx…closer monitoring • HAART better tolerance of chemoradiation2 improved local tumour control2 1. Hoffman et al. Significance of pretreatment CD4 count on outcome and treatment tolerance of HIV-positive patients with anal cancer. Int J Rad Oncol Biol Phys 1999;44:127-31. 2. Place et al. Outcome analysis of HIV patients with anal squamous cell carcinoma. Dis Colon Rectum 2001;44:506-12.
- 41. Screening & Prevention • No published guidelines that recommend screening of the general population • There are high-risk groups that may benefit from such, most prominently patients infected with HIV Rationale for screening for SIL High incidence of the anal cancer within the proposed screening population (i.e., HIV-positive patients) available screening tests are effective and cost-efficient early detection can change the outcome of the disease. The availability of effective treatments that can ablate HSIL significant morbidity and mortality associated with anal cancer if it is not prevented by effective screening and treatment. Gimenez F, Costa-e-Silva IT, Daumas A, et al. Arq Gastroenterol 2011;48:136–145.
- 42. • The initial recommended screening test is an “anal Pap smear” that evaluates cells in the anal canal for abnormal cytology through swabbing. • Patients with abnormal cytology should then be evaluated by high-resolution anoscopy, which facilitates the visualization of abnormal lesions, allowing biopsy and/or removal.
- 47. HRA images • A. Normal • B. high-grade dysplasia; i)fine irregular punctation ii)coarse irregular punctuation iii)prominent and dilated linear vessels • C. mosaic pattern with punctuation. • D. AIN with ulcer. Biopsy showed AIN 3.
- 48. High-Resolution Anoscopy • Because AIN shares many of the pathogenic features of cervical CIN, a technique similar to colposcopy has been successfully transferred to the anus as high-resolution anoscopy (HRA). • This technique is based on the principle that with the application of acetic acid to dysplastic tissue exhibits distinct changes and patterns in the anal mucosa similar to the changes seen with cervical CIN. • After application of 3% acetic acid to the anal canal and perianal skin, tissues that harbor AIN turn acetowhite. • Acetic acid sets the background upon we can identify the characteristic vascular changes of LGAIN and HGAIN. HGAIN, in addition to being acetowhite, tend to be flat and exhibit vascular punctation and mosaicism, whereas LSILs are generally raised lesions that have warty vessels.
- 49. • Lugol's solution may be applied in areas of diagnostic uncertainty. Areas that do not take up Lugol's are considered at high risk for harboring HSIL. • HRA-directed biopsies of lesions can be performed in the office or operation theatre. • HRA directed ablative procedures can be performed for HGAINs.
- 50. Anal Intraepithelial Neoplasia (AIN) • Anal and cervical canal share embryologic, histologic, and pathologic characteristics • Both develop from embryonic cloacal membrane, and are sites of fusions of endodermal and ectodermal tissue to form squamocolumnar epithelial junction • Both display metaplastic and dysplastic changes related to HPV infection
- 51. AIN-multifocal process associated with HPV, analogous to cervical dysplasia Scholefield JH, Castle MT, Watson NF. Malignant transformation of high-grade anal intraepithelial neoplasia. Br J Surg 2005;92:1133–1136.
- 52. • Once disease has reached grade III AIN, it rarely regresses. • Its estimated that approximately 1% of AIN III patients progress to invasive malignancy, annually. • Incidence of progression of AIN III is substantially increased in patients who are immunocompromised. • Prevalence of AIN among HIV-negative homosexual men is high (>36%), and almost universal among HIV-positive homosexual men. Perez,Principles and Practices of Radiation Oncology,6th edition
- 53. HG‐AIN • histologic grades AIN 2 and 3 • abnormal basaloid cells, characterized by an increased nuclear to cytoplasmic ratio, replace more than one‐half of the epithelium • true precursor of invasive anal squamous cell carcinoma LG‐AIN • histologic grade AIN 1 • 20 to 25 percent of the epithelium is replaced by abnormal cells • may spontaneously regress
- 55. Pathology
- 56. As a result, four distinct categories of tumors arise in the anal region: • Tumors that develop from any of three types of mucosa lining anal canal are termed anal canal cancers. • Tumors arising in transitional or squamous mucosa are SCCs and behave similarly (most series reporting outcomes of “anal cancer” refer exclusively to these tumors). • Adenocarcinomas arising from glandular elements are rare but share similar natural history to rectal adenocarcinomas; they are treated similarly.
- 57. • Tumors arising within hair bearing skin at or distal to mucocutaneous junction are referred as anal margin cancers. However, preferred term is perianal skin cancers. • Primary rectal SCCs(very rare), can be difficult to distinguish from anal cancers, and should be treated as anal cancer. • Determination of site of origin that overlap anorectal junction can be problematic. For staging purposes, such tumors are classified as rectal cancers if their epicenter is located >2 cm proximal to dentate line, and as anal canal cancers if <2 cm from the dentate line.
- 58. • The vast majority of anal canal tumors are classified as SCC ( 85-90 %) • It encompasses tumors previously described as – Basaloid – Cloacogenic – transitional – mucoepidermoid – verrucous mucoepidermoid varieties • From treatment standpoint, these all approached as SCC. • Majority of are nonkeratinizing, tumors arising below dentate line often display keratinizing properties. • 10% to 15% are adenocarcinomas, most of which arise from anal glands or within anal fistulae.
- 59. • Bowen's disease (SCC in situ) can occur within perianal skin as in other areas of non sun exposed skin. • Paget disease of the anus(intraepithelial adenocarcinoma) can be of two types: 1. primary cutaneous malignancy with sweat gland differentiation 2. lesion with adjacent squamous epithelium involvement by lateral intramucosal spread from underlying adenocarcinoma of rectum or perianal glands. • Anal Melanomas should be treated according to same principles commonly applied to this tumor at other sites.
- 60. Clinical Presentation • Most common presentation - bleeding from the anus. • Symptoms of anal cancer can be diverse and include – Pain – sensation of a mass – itching – anal discharge – Tenesmus – sense of fullness – lump in the anal canal. • Extensive lesions may present with incontinence, passage of gas or stool from vagina, or significant change in bowel habits. • 20% of patients are initially asymptomatic. • Any mass should be biopsied for a diagnosis.
- 61. Clinical staging is performed by a combination of clinical, endoscopic, and radiographic examinations • Detailed history including an assessment of anal sphincter function as well as HIV risk factors. • Digital rectal examination to identify – Tumor location & extent – fixation to sphincter complex or – adjacent organs such as vagina and prostate. • Anoscopy provides – information about extent of mucosal spread, including relationship to the dentate line, and – facilitates biopsy
- 62. • It may be necessary to examine patients under anesthesia secondary to pain and sphincter muscle spasms. • Female patients should undergo a gynecologic examination to determine vaginal involvement and to exclude other HPV-associated cancers. Examination of Inguinal nodes • Of all patients presenting with palpable inguinal lymph nodes, only 50% are malignant; therefore, fine-needle aspiration is often recommended in suspected cases, and a positive result may guide radiation field design and dose. • Complete blood counts with serum biochemistry including HIV/CD-4 levels in the presence of risk factors
- 63. Imaging • MRI (external phased-array coils on high-magnetic-field scanners) - imaging modality of choice Significant advantages I. Native multiplanar capability II. Superior soft-tissue differentiation III. Biological noninvasiveness IV. Optimal safety profile of gadolinium based contrast agents.
- 64. For evaluation of primary • Display low-to intermediate T1 signal intensity and positive enhancement after intravenous gadolinium contrast. • Display intermediate T2signal intensity, lower to that of normal ischioanal fat and almost always superior to internal reference standard represented by uninvolved anal sphincters and gluteal muscles • Sensitivity of MRI (& EAUS) approach 90– 100 %, with high concordance regarding tumour size.
- 65. For nodal evaluation • Short-axis threshold values of 8 mm, 5 mm and 10 mm have been suggested for pelvic, perirectal and inguinal lymph nodes, respectively • Additional features include loss of normal bean-shape and fatty hilum, internal T1 and T2 signal heterogeneity with central necrosis, and inhomogeneous enhancement • In 2010 ESMO recommended MRI as primary imaging modality to accurately stage SCAC, taking into account maximum tumour diameter, possible invasion of adjacent organs and nodal involvement
- 66. Endoanal ultrasound: Endosonography of anal canal • Diagnostic test of choice for evaluation of anal sphincter anatomy and identification of sphincter defects associated with fecal incontinence • EAUS is used to stage and follow up anal neoplasms. • Endoanal ultrasound has been used to assess tumor depth and sphincter involvement, but has not affected treatment plans and, thus, presently, ultrasound staging is not routinely recommended. • Anatomy of anal canal is imaged sonographically at three levels (upper, mid, and distal anal canal).
- 69. • Lesions of anal canal appear as hypoechoic areas on EAUS, and size and extent can be detailed. • Effective in initial evaluation • EAUS staging (uTNM) of anal canal cancers corresponds to TNM staging • EAUS is useful in detecting residual tumor as well as early local recurrence after treatment. • Currently,EAUS is part of most surveillance programs for anal cancer.
- 70. Modified endoscopic staging system • Tarantino and Bernstein • Emphasized depth of penetration over tumor size • used to distinguish early lesions amenable to less aggressive treatment. • shown in a prospective, multicenter study to be superior to clinical staging in predicting local recurrence
- 71. • CECT -used to evaluate distant disease and inguinal adenopathy • FDG-PET/CT -can address all three staging criteria(Grigsby et al):demonstrate the extent of the primary tumor; detect lymph node metastases; and reveal any sites of distant metastases • NCCN guidelines recommend PET/CT as a part of standard pre- treatment workup, but PET-CT does not replace a diagnostic CT scan
- 72. • Pre-treatment PET/CT upstaged 9-37.5% and down staged 0-25% of patients with anal cancer • Can be used for radiation planning as it clearly defines sites of metabolically active tumor. Radiation treatment fields changed in 3.7-33.3% of patients. • Sensitivity of CT for nodal metastases in pelvic and inguinal region is 40-68%. By contrast, PET/CT showed higher specificity (80- 90%) and sensitivity (70-90%) in detection of nodal and distant metastases
- 73. • Post-treatment PET/CT is indicated to determine response to therapy and it is highly predictive of long-term clinical outcomes • Recently considered for follow-up after radio- and chemo‐ therapy • Finally, PET-CT scans have prognostic value as well, with significant correlation between metabolic response posttreatment and progression-free as well as OS
- 75. AJCC Staging – Anal Canal & Anal margin Cancers • The definitions of TNM and the stage groupings have not changed from the sixth edition. • The classification applies to carcinomas only; melanomas, carcinoid tumours, and sarcomas are not included. American Joint Committee on Cancer • 2010 , AJCC 7th edition
- 76. T Staging • T X : Primary tumour cant be assessed • T 0 : No evidence of primary tumour • Tis : Carcinoma in situ (Bowen's disease, high-grade squamous and anal intraepithelial lesions) • T 1 : Tumor 2 cm or less in greatest dimension • T 2 : Tumor more than 2 cm but not more than 5 cm in greatest dimension T1 T2 2-5 cm
- 77. • T 3 : Tumor more than 5 cm in greatest dimension ANAL CANAL • T 4 : Tumor of any size that invades adjacent organ(s); e.g., vagina, urethra, bladder* • *Direct invasion of the rectal wall, perirectal skin, subcutaneous tissue, or the sphincter muscle(s) is not classified as T4 ANAL MARGIN • T 4 : Tumour invades deep extradermal structures ( i.e, cartilage, skeletal muscle or bone) >5 cm
- 78. LN Staging • N X : regional lymph nodes cannot be assessed • N 0 : no regional lymph node metastasis ANAL CANAL • N 1 : metastasis in perirectal lymph node(s) • N 2 : metastasis in unilateral internal iliac and/or inguinal lymph node(s)
- 79. • N 3 : metastasis in perirectal and inguinal lymph nodes and/or bilateral internal iliac and/or inguinal lymph nodes ANAL MARGIN • N 1 : metastasis in perirectal lymph node(s) • M Staging • M X : Distant metastasis cant be assessed • M 0 : No distant metastasis • M 1 : Distant metastasis
- 80. LN Involvement • Lymphatic drainage and nodal involvement of anal cancers depend on the location of the primary tumor. • Tumors above the dentate line spread primarily to the anorectal, perirectal, and paravertebral nodes • Tumors below the dentate line spread primarily to the superficial inguinal nodes. • The regional lymph nodes are as follows Perirectal – Anorectal – Perirectal – Lateral sacral Internal iliac (hypogastric) Inguinal – Superficial • All other nodal groups represent sites of distant metastasis.
- 81. Changes in staging AJCC 8th edn • Tumours of anal margin and perianal skin defined as within 5cm of the anal margin are now classified with carcinomas of the anal canal • T categories are unchanged • N0 No regional lymph node metastasis • N1 Metastasis in regional lymph node(s) • N1a Metastases in inguinal, mesorectal,and/or internal iliac nodes • N1b Metastases in external iliac nodes • N1c Metastases in external iliac and in inguinal, mesorectal and/or internal iliac nodes • M categories are unchanged
- 82. • Lymphatic invasion occurs relatively early. • Overall risk of regional nodal involvement at diagnosis - about 25%. • Pelvic lymph node metastases found in as many as 30% of patients treated by abdominoperineal resection. • Inguinal metastases were detected clinically in up to approximately 20% of patients at initial diagnosis and were present subclinically in further 10% to 20%. • Nodal metastases were associated with 30% of cancers confined to the sphincter muscles. • Ortholan C, Resbeut M, Hannoun-Levi JM, et al. Anal canal cancer: management of inguinal nodes and benefit of prophylactic inguinal irradiation (CORS-03 study). Int J Radiat Oncol Biol Phys 2012;82(5):1988–1995. • Bilimoria KY, Bentrem DJ, Rock CE, et al. Outcomes and prognostic factors for squamous cell carcinoma of the anal canal: Analysis of patients from the National Cancer Data Base. Dis Colon Rectum 2009;52:624–631.
- 83. Stage Grouping
- 84. Anal melanoma staging • Staged on a clinical basis, focusing on loco-regional and distant spread • Stage I is local disease only, Stage II is a local disease with increased thickness and ulcerations, Stage III is local disease with involvement of regional lymph nodes, and Stage IV shows distant metastatic disease
- 86. Prognostic Factors 1.Tumour factors • T and N stages are most important prognostic factors • 5-year OS for stage I, II, IIIA, IIIB, and IV are 69.5%, 68.1%, 45.6%, 39.6%, and 15.3%, respectively RTOG 98-11 study- tumor size (>5 cm), involved lymph nodes (N+), and male sex were associated with worse 5-yr DFS and OS EORTC 22861 study- skin ulceration, lymph node involvement, and male sex were independent variables associated with LRF and OS • histologic subtypes have not been shown as substantial prognostic factors.(study by Schlienger et al - no significant difference in survival among cloacogenic, well-differentiated, and moderately or poorly differentiated anal carcinomas.
- 87. 2.Patient factors • Performance status • Gender • Patients who continue to smoke tobacco- greater risk of local relapse. • HIV-positive patients- impaired tolerance of RT and chemotherapy. – high viral load – low lymphocyte CD4-positive counts.
- 88. 3.Biochemical & Molecular factors p53 • overexpressed with a range of 34% to 100%. • Wong et al. described that increased p53 expression was associated with worse local–regional control and DFS p21 • lack of p21 expression is associated with poor prognosis in SCCA. • Holm et al. reported that lack of p21 expression was associated with reduced OS • Nilsson et al. reported that absence p21 expression was responsible for increased LRF. • Ki-67, nuclear factor kappa B, SHH, and Gli-1 are associated with DFS
- 89. Treatment Topical therapy • For small lesions (<1 cm at base) • Bichloroacetic or Trichloroacetic acid • topical 5‐fluorouracil Immune modulation • Imiquimod (ALDARA) ‐ can result in pathological resolution of AIN in HIV positive MSM on HAART Infrared coagulation • For lesions that are too large for TCA • direct application of a 1.5 second pulse of irradiation in the infrared range to dysplastic anal epithelium • results in tissue destruction to depth of approximately 1.5 mm
- 90. Imiquimod • A topical immunomodulator, acts on the Toll-like receptor 7 of the humoral immune system resulting in the secretion of various proinflammatory cytokines and activation of both humoral and cell-mediated immunity. • In a series by Wieland U et al 28 HIV-positive men with high- risk HPV types who were treated with imiquimod 3 times a week for 16 weeks, 17 showed a complete clinical and pathologic response. Of the patients with HGAIN, 78% had a complete response, with a concomitant decrease in HPV DNA. Two with LGAIN progressed to HGAIN.
- 91. • Imiquimod may be safely recommended for treatment of patients with LGAIN and HGAIN with higher CD-4 lymphocyte counts. • Close follow-up is required given the high recurrence rate.
- 92. TCA and BCA • Topical 85% trichloroacetic acid (TCA) or bichloroacetic acid are directly cytotoxic therapies that destroy tissue by chemical coagulation of proteins. • There has been a single report by Singh JC et al of TCA treatment in 54 patients with AIN. • The study included a mixture of immunosuppressed patients, 65% of whom were HIV-infected. Patients were treated with topical TCA at intervals of 1–2 months for up to four applications
- 93. • A median of two treatments was required for patients who had no evidence of AIN at follow-up HRA examination • When analyzed on a per lesion basis, 73% of AIN-1 patients and 71% of AIN-2/3 patients had no evidence of AIN on follow-up HRA examination. • The authors concluded that TCA, because of its ease of use, low cost, and good safety profile, was a reasonable first-line therapy for patients with two or fewer AIN lesions.
- 94. Topical 5 FU • In a prospective trial (Richel O et al )from Europe, 46 HIV-infected MSM were enrolled, approximately 75% of whom had multifocal HGAIN. • The purpose of this pilot study was to evaluate the safety and efficacy of treatment with 5% 5- FU for all grades of AIN. • 18 participants (39%) had complete clearance of AIN and 8 (17%) had a partial response. 17 participants (37%) did not respond.
- 95. • These data taken together demonstrate the efficacy of 5-FU, but the optimal dose, frequency of administration, and duration of treatment are uncertain. • Authors concluded that 5-FU works well, but only for patients who are motivated enough to tolerate the side effects for treatment of extensive and often severely symptomatic AIN.
- 96. Anoscopy directed lesion ablation • Large or circumferential lesions • Electrocautery ablation • The use of high‐resolution anoscopy may minimize complications • High rate of local recurrence, even with complete ablation, mandates careful surveillance
- 97. HRA directed Infrared Coagulation • Goldstone recognized that the standard surgical techniques had excessive morbidity and were unsuitable for treating multifocal disease, which is increasingly being identified in immunosuppressed patients. • Infrared coagulation, which has been used successfully for treatment of internal hemorrhoids and condyloma, was offered for treating AIN. • Infrared coagulation ablation offers important advantages for patients being treated for AIN. Infrared coagulation requires no anorectal preparation, and is performed as an outpatient procedure under local anesthesia.
- 98. HRA guided electrocautery ablation • HRA-guided electrocautery was initially described as an operating room technique for extensive HGAIN disease. • There is only one study by Goldstone et al, wherein 232 patients were treated with HRA guided Electrocautery ablation. At final evaluation 83% of HIV-negative patients and 69% of HIV-positive patients were free of HGAIN • Goldstone et al compared his results using HRA-guided electrocautery ablation with infrared coagulation of HRA, and concluded that the outcome of electrocautery ablation was similar to infrared coagulation.
- 99. Treatment • Until the late 1970s, the conventional treatment for anal canal cancer was an APR. • Nigro et al. challenged this practice with a report of 3 patients with squamous cell cancer of the anal cancer who following preoperative treatment with 30 Gy plus concurrent fluorouracil (5-FU) and mitomycin-C were found to have a pathologic complete response at the time of surgery.
- 100. Role of surgery • Surgery for the initial diagnosis and staging of anal canal tumors should be limited to a biopsy of the primary tumor and evaluation of the inguinal lymph nodes. • Clinically enlarged inguinal lymph nodes should be aspirated. If the cytology is nondiagnostic or demonstrates only benign disease, an open excisional biopsy of 1 or 2 lymph nodes is recommended. • Under no circumstances should a formal lymph node dissection be performed for the initial evaluation of suspicious nodes, as it can increase the morbidity of radiation and has no therapeutic value.
- 101. EVOLUTION OF TREATMENT MODALITIES • Local and locally advanced AC • Initially, non-metastatic tumors of the anal canal were treated with abdominoperineal resection (APR) and permanent colostomy, with a five-year survival of 40% to 70% and a perioperative mortality of 3%. In 1974, Nigro et al achieved complete pathological response in 3 patients using a combination of radiation therapy (30 Gy) and chemotherapy that included mitomycin C (MMC) and 5-fluorouracil (5-FU).
- 102. nnorn
- 112. Role of Sentinal lymph node biopsy • Some authors have suggested a routine SLN evaluation as a staging technique. • A systematic review of 16 published series evaluating outcome of SLN biopsy of inguinal nodes included 323 patients, and success in identifying SLN was 86%.
- 113. Adenocarcinoma of Anal canal • Adenocarcinoma arises from the columnar epithelium of the anal canal and its incidence is low accounting for less than 5 % of all anal malignancies. • Extension of rectal cancer into the anal canal is the more common presentation. Occasionally, adenocarcinoma may occur in patients with ulcerative colitis or Crohn disease who have ileal pouch-anal anastomosis. • APR should be offered for early-stage disease.(T1, T2 and N0) • For locally advanced disease (T3 or any T with N + ), a multimodality approach should be considered.
- 114. Melanoma of Anorectal region • Anorectal melanoma is rare and accounts for less than 3 % of all malignant melanomas and less than 1 % of all anal canal tumors. • The 5 -year OS rate is generally less than 20 % . The initial stage at presentation largely determines OS. • Ross et al. from the M. D. Anderson Cancer Center reviewed a series of 32 patients with melanoma treated with either APR or local resection. • Local recurrence was lower in the APR group (29 % for APR; 5 8 % for local excision) . However, there was no difference in OS between the two groups ( 19 . 5 months for APR; 18 .9 months for local resection ) . • Most authors recommend local excision of anorectal melanoma if adequate margins could be achieved.
- 115. Perineal reconstruction- VRAM Flap
- 116. Role of Vaccination • A promising strategy for the prevention of anal dysplasia and malignancy is HPV vaccination. • Two vaccines (Cervarix and Gardasil) are now approved by the U.S. Food and Drug Administration and have been shown to protect against cervical cancer in women. • The quadrivalent HPV vaccine Gardasil has demonstrated efficacy for prevention of HPV 6-, 11-, 16-, and 18-related genital warts and has been shown to protect against cancers of the anus, vagina, and vulva. * Palefsky JM, Giuliano AR, Goldstone S, et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N Engl J Med 2011;365:1576–1585.
- 118. • In a large, double blind study, (Palefsky et al) – 602 healthy homosexual men were randomized to receive the quadrivalent HPV vaccine versus placebo. • Significantly reduced rates of (36-month median follow-up) – high-grade anal dysplasia – high-risk HPV infection in the vaccinated group. • With limited availability and suboptimal outcomes of AIN screening programs, vaccination may reflect the best long-term approach for reducing anal cancer risk * Palefsky JM, Giuliano AR, Goldstone S, et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N Engl J Med 2011;365:1576–1585
- 119. • FDA has approved Gardasil for prevention of HPV-caused cervical, vulvar, vaginal, and anal cancers; precancerous cervical, vulvar, vaginal, and anal lesions; and genital warts in males and females ages 9 through 26 • Vaccines are given through a series of three injections into muscle tissue over a 6- month period(at 0,1 &6 month). • In October 2016, the FDA approved a 2-dose schedule for boys and girls initiating vaccination with Gardasil at ages 9 to 14 years (the second dose is to be administered 6–12 months after the first). • Those initiating the HPV vaccination series at older ages (including teens who begin getting vaccinated after they turn 15 years old) or who are immunocompromised should still be vaccinated according to the 3-dose schedule.
- 120. • CDC & ACIP has developed the following recommendations regarding HPV vaccination : initiation of routine HPV vaccination at age 11 or 12 years (the vaccination series can be started beginning at age 9 years) vaccination of females aged 13 through 26 years and of males aged 13 through 21 years who have not been vaccinated previously or who have not completed the 3-dose vaccination series. Males aged 22 through 26 years may be vaccinated As of October 2016, CDC and ACIP also now recommend that 11- and 12-year-olds receive two doses of HPV vaccine at least 6 months apart rather than the previously recommended three doses.
- 122. Summary • Knowledge of Anatomy is essential in treating anorectal disease especially for treating benign conditions. • With increase in immunosuppressed population, the incidence and prevelance of AIN is increasing, the natural history of which is unknown, diverse treatment options are available with varying results. • APR is offered for treating residual and recurrent localised anal canal squamous cell carcinoma post Chemo-RT. • T1 N0 WD Anal margin carcinoma can be treated with WLE. • Adenocarcinoma primarily treated with APR. • Melanoma primarily treated with wide excision or APR.
