More Related Content Similar to Nrgastro.2011.196 (20) More from Elsa von Licy (20) 1. REVIEWS
Hepatocellular carcinoma: insight from
animal models
Yan Li, Zhao-You Tang and Jin-Xuan Hou
Abstract | Hepatocellular carcinoma (HCC) ranks as the third most common cause of death from cancer
worldwide. Although major risk factors for the development of HCC have been defined, many aspects of
the evolution of hepatocellular carcinogenesis and metastasis are still unknown. Suitable animal models
are, therefore, essential to promote our understanding of the molecular, cellular and pathophysiological
mechanisms of HCC and for the development of new therapeutic strategies. This Review provides an overview
of animal models that are relevant to HCC development, metastasis and treatment. For HCC development,
this Review focuses on transgenic mouse models of HBV and HCV infection, which provide experimental
evidence that viral genes could initiate or promote liver carcinogenesis. Animal models of HCC metastasis
provide platforms to elucidate the mechanisms of HCC metastasis, to study the interaction between the
microenvironment and HCC invasion and to conduct intervention studies. In addition, animal models have
been developed to investigate the effects of new treatment modalities. The criteria for establishing ideal HCC
animal models are also discussed.
Li, Y. et al. Nat. Rev. Gastroenterol. Hepatol. 9, 32–43 (2012); published online 25 October 2011; doi:10.1038/nrgastro.2011.196
Introduction
Department of
Oncology, Zhongnan
Hospital of Wuhan
University, 169 Donghu
Road, Wuhan 430071,
China (Y. Li, J.‑X. Hou).
Liver Cancer Institute
and Zhongshan
Hospital, Fudan
University, Key
Laboratory of
Carcinogenesis and
Cancer Invasion (Fudan
University), Ministry of
Education, China, 136
Yi Xue Yuan Road,
Shanghai 200032,
China (Z.‑Y. Tang).
Hepatocellular carcinoma (HCC) is one of the most
common types of cancer worldwide. Indeed, of the
748,300 new liver cancer cases and 695,900 liver-cancerrelated deaths estimated to have occurred in 2008, 70–85%
are believed to have been caused by HCC.1 In addition,
half of the total liver-cancer-related deaths and new cases
are thought to have occurred in China, rendering HCC
the top priority in China’s anticancer campaign.1
Liver carcinogenesis is a multistep process: the presence of specific risk factors promotes gene damage,
which leads to a cascade of molecular and cellular
deregulations that ultimately result in transformation
of hepatocytes (Figure 1). In China and sub-Saharan
Africa, the most important risk factors for HCC are
HBV infection and exposure to environmental toxins
including aflatoxin B1 and diethylnitrosamine.2,3 By contrast, HCV infection, alcohol-related liver cirrhosis and
nonalcoholic fatty liver disease are the most important
risk factors for HCC in developed countries and other
low-risk areas. 2,4,5 Globally speaking, however, viral
hepatitis is the single most important cause of HCC, particularly the HBV and HCV subtypes, which are jointly
responsible for up to 80% of HCC cases worldwide.6,7
Moreover, a population-based, long-term, prospective
cohort study has provided convincing evidence that an
elevated serum HBV DNA level (≥10,000 copies/ml) is a
strong independent risk factor for HCC.8 Similarly, clinical and epidemiological data also suggest that HCV is an
independent cause of HCC.9
Correspondence to:
Z.‑Y. Tang
zytang88@163.com
Competing interests
The authors declare no competing interests.
32 | JANUARY 2012 | VOLUME 9
Establishing successful animal models of HCC is,
therefore, crucial for both basic and translational studies
of HCC. A wide range of HCC animal models are currently available, which have provided researchers with
the opportunity to assess tumor–host interactions,
perform drug screening, mimic the complex multistep
process of liver carcinogenesis, and conduct various
therapeutic experiments. No model, however, is ideal for
all purposes. Consequently, investigators should make
a knowledgeable selection from the currently available
models, or construct new models, on the basis of several
key criteria (Box 1).
This Review focuses on the insights obtained from
animal models of liver carcinogenesis associated with
viral hepatitis. An exhaustive evaluation of all HCC
animal models in current use is beyond the scope of this
article, although several interesting reviews on this topic
have been published elsewhere.10–13 In this article, we
focus on the animal models that are relevant to studies
of HCC development, metastasis and treatment.
Models of HCC development
Transgenic mouse models of HBV or HCV infection have
provided reliable experimental proof that viral genes
could initiate or promote liver carcinogenesis.
HBV transgenic mouse models
Multiple transgenic mice models that express specific
fragments of the HBV genome have been generated
for the study of HBV-induced liver carcinogenesis.
These transgenes are usually under the control of either
the HBV promoter, or liver-specific host promoters,
www.nature.com/nrgastro
© 2011 Macmillan Publishers Limited. All rights reserved
2. REVIEWS
including those for albumin or metallothionein. Most
HBV transgenic mouse models focus on the HBx gene,
which encodes HBV X protein (HBx)—a transcriptional
transactivator that stimulates expression of a broad range
of proto-oncogenes, including c‑fos, c‑myc and c‑jun.14,15
Activation of these proto-oncogenes shifts transforming
growth factor β signaling from tumor-suppressive
to oncogenic pathways 16 that stimulate hepatocyte
proliferation,17 inhibit apoptosis,18 upregulate protein
degradation,19 and induce genetic instability and DNA
repair mechanisms.19
Kim et al. 20 investigated the role of the HBx gene
in the development of HCC using a transgenic CD1
mouse model (Table 1). In contrast to wild-type CD1
mice, which do not normally develop spontaneous liver
tumors and have a lifespan of approximately 24 months,
the majority of HBx transgenic mice died from clear
cell HCC at 11–15 months of age. Interestingly, male
mice died earlier than female mice owing to a faster
rate of HCC progression. Multifocal areas of altered
hepatocytes with high levels of HBx protein were found
in the transgenic mice 4 months after birth, and by
months 8–10 these altered hepatocytes had developed
into adenomas that expressed high levels of HBx protein
and α‑fetoprotein (AFP). Expression of these proteins
remained high until the mice died.
Two features differed in the findings from this animal
model compared with clinical settings—cirrhosis and
inflammation were absent in the preneoplastic stages,
which signifies a direct contribution of the HBx protein
to carcinogenesis.20 Proteomic analysis of liver tissue in
the early stages of HCC (dysplasia and adenoma) from
HBx transgenic mice21 (Table 1) identified 22 proteins
with altered expression levels, the majority of which were
involved in the crucial metabolic processes of glyco
lysis and lipogenesis.22 These observations indicate that
considerable metabolic changes occur in the early stages
of liver carcinogenesis.22 Another proteomics study 23
looked at fully developed HCC tissue from HBx transgenic mice24 (Table 1) and found persistent upregulation
of the ubiquitin–proteasome and lysosomal pathways.23
These findings indicate the continual presence of cell
injury, leading to protracted production of reactive
oxygen species (ROS) and liver regeneration.
The two most prominent theories of carcinogenesis are
the one-hit theory, in which a carcinogen both initiates
and promotes cancer formation, and the two-hit theory, in
which the first causative factor initiates cell transformation
and a second one promotes transformed cells to develop
into cancer.25 The HBx transgenic mouse studies suggest
that the expression of the HBx gene itself directly, and
independently of other factors, causes HCC; these results,
therefore, support the one-hit theory of carcinogenesis.26
Lakhtakia et al.27 constructed an HBx15–c-myc transgene model in C57BL/6xSJL mice to determine whether
the presence of HBx plus an oncogene would result in
substantially accelerated HCC progression (Table 1).
The transgene comprised an HBx gene fragment that
led to expression of a truncated HBx protein (X1558–154),
which is sufficient to provide the crucial transactivating
Key points
■■ Suitable animal models are necessary to provide information on the molecular,
cellular and pathophysiological mechanisms of hepatocellular carcinoma (HCC)
■■ Transgenic mouse models have provided reliable experimental evidence
suggesting that viral hepatitis genes could have a primary role in initiating or
promoting liver carcinogenesis
■■ Nonviral factors, including oncogenes and environmental carcinogens, might
only have a secondary role in liver carcinogenesis, but they could considerably
accelerate the transformation of hepatocytes
■■ An animal model of metastatic human HCC that incorporates the effects of
variation in metastatic potential would provide a unique tool for the study of
HCC metastasis
■■ Animal models of HCC could be useful for developing and testing novel
therapeutic modalities
function, along with the mouse c‑myc oncogene. The
transgenic mice exhibited a considerable increase in liver
size and weight, which was most noticeable 5 months
after birth. As noted in the HBx transgenic mouse study
by Kim et al.,20 mice in this model also had no cirrhosis or inflammation in the preneoplastic stages.27 c‑myc
expression was predominantly cytoplasmic, and more
noticeable in neoplastic nodules than in the surrounding
normal liver cells. This model, therefore, suggests that
synergism occurs between the HBx gene and c‑myc in
HCC development,27 and so supports the two-hit theory:
after the first hit by HBx protein, the second hit by c‑myc
considerably shortens the liver carcinogenesis process, by
as much as 4 months.
In contrast to the HBx transgenic mouse models, transgenic mice that express the viral S gene, which encodes
HBV surface antigen (HBsAg), do develop distinctive
inflammation and HCC, especially male mice.24,28 Chisari
et al.28,29 developed an HBV transgenic mouse model,
designated Tg (Alb‑1 HBV) Bri44, which undergoes a
distinct form of liver carcinogenesis (Table 1). These
mice have been engineered to contain HBV genomic
sequences that encode HBx, HBsAg, and pre‑S proteins
(the viral S gene, which encodes the viral capsid protein
HBsAg, contains three in-frame start codons that allow
three peptides of different lengths [pre‑S1+S, pre‑S2+S,
and S respectively] to be transcribed from the same gene).
These transgenic mice do not spontaneously develop
tumors. At 1 month after birth, Tg (Alb‑1 HBV) Bri44
mice have normal liver histology. By month 2, however,
discrete areas of hepatocellular necrosis and inflamma
tion occur, and by month 3, progressive hepato yte
c
damage, Kupffer cell hyperplasia and mononuclear cell
infiltration can be observed, which mimics the features
of chronic hepatitis in humans.29–32 By months 4–6,
these degenerative alterations30 are followed by cell lar
u
damage caused by an active inflammatory response
and elevated compensatory hepatocyte proliferation,32
which constitutes a precancerous state. By months 7–9,
adenomas develop, which in 33% of cases are of the clear
cell type.31 By month 12, typical HCC with trabecular
histology is present.28 Neoplastic lesions progressively
grow to macroscopic nodules that can be observed in all
animals by months 16–18.
NATURE REVIEWS | GASTROENTEROLOGY HEPATOLOGY
© 2011 Macmillan Publishers Limited. All rights reserved
VOLUME 9 | JANUARY 2012 | 33
3. REVIEWS
HBV
Hepatocytes
HBV surface antigen filaments
HBV protein
Peroxisome proliferation
Endoplasmic reticulum
Transactivation
No inflammation
Glucose and fatty acid metabolism disturbance
Lipid droplets
Cell injury and inflammation
Diethylnitrosamine
aflatoxin
Oxidative stress
Steatosis
Alcohol
Reactive
oxygen
species
Gene damage
Multiple random
mutations in hepatocytes
Signaling pathway
disturbance
Adenoma
HCC
Steatosis
Lipid droplets
Electron transfer
system disturbance
Mitochondria
Cytoplasm
Nuclei
Hepatocytes
Core protein
HCV
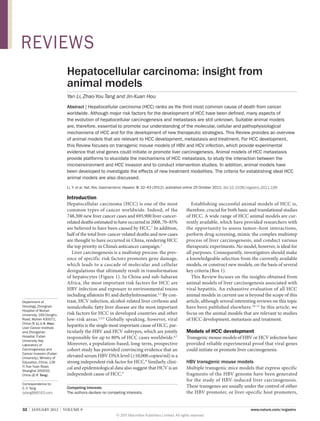
Figure 1 | Model of liver carcinogenesis based on evidence obtained from transgenic mice. Viral factors exert a dominant
role in HCC development through promotion of the central mechanism of increased oxidative stress and ROS generation.
This mechanism leads to a vicious cycle of injury, DNA damage and liver regeneration, which render hepatocytes at an
increased risk of transforming mutations. External factors, including exposure to chemicals and alcohol, have only a
secondary role in the development of HCC. Red boxes indicate major factors or events. Blue boxes indicate secondary
factors. Solid arrows indicate major processes, and dashed arrows indicate minor processes. Abbreviation: HCC,
hepatocellular carcinoma.
Overexpression of the large HBV envelope poly
peptide in mice initiates a process of hepatocyte injury,
inflammation, and regenerative hyperplasia that renders
large numbers of hepatocytes at risk of developing
transforming mutations.28 Interestingly, HBV envelope
protein was found in all hepatocytes from these animals
by months 2–7, however, it was not expressed in all adenomas, nor in any HCCs. AFP levels also increased with
the develop ent of adenomas and HCCs. This model,
m
therefore, mimics many of the pathological events that
occur before the development of HCC in humans with
chronic HBV infection, and provides a useful tool to
study the processes of carcinogenesis and progression of
34 | JANUARY 2012 | VOLUME 9
HCC following HBV infection. Again, this model also
supports the one-hit hypothesis, as HBV acts as a complete carcinogen that causes HCC by initiating a complex
series of events in response to chronic hepatocyte injury.
To study the dysregulatory events that occur during
early liver carcinogenesis, Barone et al.33 compared the
gene expression profile of 3‑month-old Tg (Alb‑1 HBV)
Bri44 transgenic mice with 3‑month-old wild-type
animals. Microarray data on a total of 12,600 genes
showed that the expression of 45 genes was significantly different in the transgenic mouse—25 genes were
upregulated and 20 genes downregulated. The products
of many of the upregulated genes have immunological
www.nature.com/nrgastro
© 2011 Macmillan Publishers Limited. All rights reserved
4. REVIEWS
functions, suggesting that the accumulation of viral
proteins results in hepatocyte damage and an immune
response. 28,32,34 Moreover, several of the genes with
altered expression were associated with apoptosis, such
as upregulation of the gene encoding the antiapoptotic
protein NuprI35 and downregulation of the gene encoding the proapoptotic protein Bnip3.36 This finding supports the conclusion that dysregulation of apoptosis,
which facilitates the escape of ‘abnormal’ cells from
death, could be a mechanism through which HBV
promotes HCC development.27
In a similar fashion, Sell et al.37 constructed HBsAg
transgenic C57BL/6 mice (Table 1). The 50‑4 strain of
these mice had a high HBsAg content in hepatocytes,
premalignant changes, nodules, adenomas and HCC;
exposure to diethylnitrosamine or aflatoxin accelerated
the development of HCC, and produced considerably
more tumor nodules in the liver. This model demonstrates that the HBsAg protein itself could be both an
initiator and a promoter of hepatocyte transformation,
and that the addition of environmental carcinogens
consider bly accelerates this process.
a
HCV transgenic mouse models
Several HCV transgenic mouse model systems have been
established that are based on the structure of the HCV
genome (Table 2). Currently, transgenic mice expressing
HCV structural proteins (core, E1, E2 and p7) or nonstructural proteins (NS2, NS3, NS4A, NS4B, NS5A and
NS5B) individually or in various combinations are available.38 These proteins are designed to be constitutively
expressed under the control of liver-specific promoters.
Koike et al. established HCV envelope gene (E1 and
E2)39 and core gene40,41 transgenic models, in which the
expression of each gene is under the control of the same
enhancer or promoter (Table 2). Only mice engineered
to express HCV core gene developed HCC.40 As early
as 3 months of age, HCV core gene transgenic mice
developed hepatic steatosis—a histological feature of
chronic HCV infection. In mice aged up to 12 months,
steatosis slowly progressed without neoplastic changes.
At month 16, one-quarter of the male transgenic mice
of the C21 line had developed HCC, but no female mice
of the C21 line had developed tumors. Moreover, the
livers of transgenic mice aged over 12 months exhibited morpho ogical changes, including hepatic nodules
l
filled with eosinophilic cells containing fat droplets, suggesting an age-dependent increase in oxidative stress.
In this study,40 therefore, transgenic mice at ages 6, 12
and 16 months represent the early, medium, and late
stages of liver carcinogenesis, respectively. A proteomics
study of HCV core gene transgenic mice42 found that in
animals over 6 months of age, the expression of apoptosis-promoting proteins was suppressed. In animals over
12 months of age, expression of proteins related to cellular respiration, the electron-transfer system and antioxidative pathways was significantly upregulated. Finally,
in animals aged over 16 months, expression of proteins
related to defense, oxidation, and apoptosis was also
significantly suppressed. This fluctuating expression of
Box 1 | Criteria for the selection and design of animal models of HCC
■■ The model should faithfully and stably reproduce the key biological behaviors of
HCC. For example, there should be clear and distinctive stages of hepatocyte
degeneration, regeneration, proliferation and transformation in spontaneous
models of HCC
■■ The model should help to reliably and reproducibly evaluate key molecular and
cellular events in HCC development and progression
■■ The model should adequately reflect the full range of interactions between the
tumor and the host, and between the primary tumor and metastases
■■ The model should mimic the human tumor microenvironment
■■ The model should be affordable and easy to manipulate
Abbreviation: HCC, hepatocellular carcinoma.
proteins could explain the stages of liver carcinogenesis.
At the initial lesion stage (6 months), major changes are
decreased apoptosis and increased β‑oxidation. At the
precancer stage (12 months), the most prominent change
is the shift from mitochondrial respiration to aerobic
glyco ysis associated with malignant transformation. At
l
the final cancer stage (16 months), the most characteristic changes are markedly decreased biological functions including respiration, protein synthesis, defense
and metabolism.
Another HCV transgenic mouse model has provided
convincing evidence to support the direct carcinogenic
role of viral proteins in HCC (Table 2).43 This work established full-length HCV polyprotein (FL‑N) and HCV
structural protein (S‑N) transgenic models. Adenomas
and HCCs developed in these animals from month 13.
Major histopathological features in the liver of both
FL‑N and S‑N transgenic mice included the absence of
inflammatory cell infiltrate, prominent microvesicular
and macrovesicular centrilobular steatosis, adenoma
and HCC of mixed histological types accompanied by
hepatic fibrosis. Once again, this work confirmed the
pre-eminent role of HCV structural proteins in HCC
development, although nonstructural proteins could also
contribute to liver carcinogenesis.43
Kamegaya et al. 44 developed HCV transgenic
mouse models with a common genetic background
(FVB×C57BL/6) that expressed either core E1–E2 genes
or the HCV core gene alone (Table 2). To accelerate HCC
development in these mice, which have a low susceptibility to tumors, they also received intra eritoneal injecp
tions of diethylnitrosamine once a week for 3 weeks.
Interestingly, although similar numbers of liver tumors
developed in all three groups of mice (wild-type diethylnitrosamine-treated controls and both transgenic
models), the core E1–E2 transgenic mice developed
significantly larger tumors (approximately 4 mm in dia
meter) than wild-type or transgenic mice expressing the
HCV core gene only (approximately 1 mm in diameter).
Key histopathological features of livers from core E1–E2
mice included well- ifferentiated HCC, mild steatosis,
d
no inflammation and no fibrosis. Of particular note is
the finding that E1 and/or E2 protein might accelerate
liver carcinogenesis by suppression of apoptosis rather
than by enhanced proliferation.
NATURE REVIEWS | GASTROENTEROLOGY HEPATOLOGY
© 2011 Macmillan Publishers Limited. All rights reserved
VOLUME 9 | JANUARY 2012 | 35
5. REVIEWS
Table 1 | Mouse models of HCC development resulting from HBV infection
Mouse model
Transgenes expressed
Morphological signs of HCC development
Reference
CD1
HBx gene plus transcription
enhancer
Month 4: high expression of HBx protein
Months 8–10: adenoma formation and high expression of HBx and AFP
Months 11–15: death of male mice from clear cell HCC
Kim et al.
(1991)20
C57BL/6xDBA
HBx gene, the HBV
transcriptional enhancer
and a portion of the pre C–C
sequence
Month 4: high expression of HBx protein
Month 6: small neoplastic nodules form. High expression of HBx and PCNA
Months 11–18: grossly identified HCC formation and high expression of HBx and PCNA
Month 17: metastatic mesenteric mass formation. High expression of HBx and PCNA
Yu et al. (1999)21
Transgenic
C57BL/6 (p21HBsAg or
p21-HBx)
HBsAg or HBx genes
Month 5: significantly elevated levels of serum glutamic-pyruvic transaminase in
p21-HBsAg transgenic mice
Up to month 12: half of the mice had steatosis without inflammatory or neoplastic
changes
Months 15–24: most male but no female p21-HBsAg mice developed HCC
Months 18–24: both male and female p21-HBx mice developed HCC
Wang et al.
(2004)24
Transgenic
C57BL/6xSJL
HBx15–c-myc
HBx gene encoding amino
acids 58–154 plus c‑myc
Week 1: increased mitosis, nuclear pleomorphism and multiple nuclei in hepatocytes
Months 2–3: focal necrosis; proliferation of Kupffer cells
Months 4–5: distinct adenomas; multifocal, well-differentiated HCC with a trabecular
pattern. Significant increase in liver size and weight
Weeks 24–32: microscopic HCC developed
Weeks 28–32: gross HCC developed
Lakhtakia et al.
(2003)27
Transgenic
(Alb‑1 HBV)
Bri44
Pre‑S, HBsAg, HBx genes
Months 2–7: high expression of HBV envelope protein
Month 4: moderately severe chronic hepatitis occurrence
Month 6: regenerative nodules and oval cell hyperplasia development
Month 8: liver cell adenomas formation and high expression of AFP
Months 12–20: HCC development and high expression of AFP
Dunsford et al.
(1990);28 Chisari
et al. (1985);29
Toshkov et al.
(1994);31 Huang
et al. (1995)32
Female
C57BL/6
linage 50-4
HBsAg gene
Months 3–15: elevated serum AFP level
Month 15: transgenic mice exposed to aflatoxin and diethylnitrosamine developed
adneomas or carcinomas. No adenomas or carcinomas developed in transgenic mice
not exposed to a carcinogen
Sell et al.
(1991)37
Abbreviations: AFP, α-fetoprotein; HBx, HBV X protein; HBsAg, HBV surface antigen; HCC, hepatocellular carcinoma; PCNA, proliferating cell nuclear antigen.
Models of HCC metastasis
Metastasis is a fundamental biological behavior of HCC
and the main cause of treatment failure. HCC is prone to
both intrahepatic and extrahepatic metastasis. In a clinical
setting, the most common site of distant spread is the lung,
owing to dissemination of tumor cells via the bloodstream,
hemodynamic features of the liver and the intrinsic biological characteristics of the tumor, such as increased
prolifera ion, invasion and motility 45 (Figure 2a).
t
Our research group has developed several mouse
models of spontaneous HCC metastasis. Preliminary
studies, in which tumor tissue from 30 patients with
HCC were orthotopically implanted into athymic
BALB/c mice, resulted in identification of a HCC xenograft model with high metastasic potential (LCI‑D20).46
Our subsequent studies using the LCI‑D20–BALB/c
model system led to the development of MHCC97
cells, which develop lung metastases when inoculated
orthotopically into BALB/c nude mice.47 From this cell
line, two subclone variants with high (MHCC97H) and
low (MHCC97L) metastatic potential were also established. MHCC97H cell clones were then subjected to
three, six and nine rounds of in vivo selection of a high
potential to metastasize, to produce three HCC cell lines
(HCCLM3, HCCLM6 and HCCLM9) with a greater
metastatic potential than MHCC97H (Figure 2b).48,49 As
the MHCC97 cell line, MHCC97L cell clone, MHCC97H
cell clone, HCCLM3, HCCLM6 and HCCLM9 cell lines
are derived from the same original tumor tissue model
36 | JANUARY 2012 | VOLUME 9
(LCI‑D20), together they make a ‘spontaneous stepwise
metastasis model system’. In addition, as all of the cell
lines originated from one genetic background, comparisons of gene or protein expression profiles from tumor
cells with different metastatic potentials could help
to discover metastasis-related markers. For example,
overexpression of cytokeratin 19 (CK19) is associated
with high metastatic potential,50 and this protein has
also been identified as a progenitor-cell marker in a rat
HCC model.51
Of practical importance, the MHCC97–BALB/c
model system could help to validate metastasis-related
or recurrence-related tumor biomarkers. Several important signaling pathways and candidate markers have been
identified at the gene49 and protein level.50 We found that
several key molecules, including X‑linked inhibitor of
apoptosis protein,52 calpain small subunit 1 (Capn4),53
programmed cell death 1 ligand 1 (PD-L1),54 CD24,55
CD15156 and β‑catenin57 were overexpressed in highly
metastatic cell lines including HCCLM3 and HCCLM6,
and these molecules could, therefore, be candidate biomarkers for future investigation in diagnostic studies
and as targets for therapy. Tumor nodules consisting of
CD90+ cells appeared in nude mice 3 months after sub
cutaneous injection of 500 cells from either MHCC97L
or MHCC97H cell lines, suggesting that CD90 is a potential marker of liver cancer stem cells.58 This model system
could also provide a platform for drug screening. For
example, the antitumor and antimetastatic effects of
www.nature.com/nrgastro
© 2011 Macmillan Publishers Limited. All rights reserved
6. REVIEWS
Table 2 | Mouse models of HCC development resulting from HCV infection
Transgenes expressed
Morphological signs of HCC development
Reference
HCV envelope gene
(E1–E2)
Months 0–24: no adenoma or HCC development and high expression of envelope protein
Months 1–18: absence of envelope proteins in the sera of mice
Koike et al.
(1995)39
HCV core gene
Month 3: mice transgenic for HCV core genes developed hepatic steatosis
Month 12: steatosis slowly progressed without neoplastic change
12 months: liver morphology indicated an age-dependent increase in oxidative stress
Month 16: male mice—25.9% of C21 line and 30.8% of C49 line developed HCC.
Female mice—0% of C21 line and 14.3% of C49 line developed HCC
Moriya et al.
(1998);40
Koike et al.
(2002)41
HCV polyprotein (FL‑N)
or structural protein
(S‑N)
10 months: moderate to severe steatosis developed and increased with age
≥13 months: HCC developed in FL‑N/35 strain without hepatic fibrosis
18 months: HCC developed in S‑N/863 strain without hepatic fibrosis
Lerat et al.
(2002)43
HCV core gene or core
E1–E2 gene
Months 0–21: no HCC or adenoma development in transgenic mice with the
FVBxC57BL/6 background
Week 20: after initial treatment with diethylnitrosamine, both transgenic and
nontransgenic mice had growth retardation
Week 32: both transgenic and nontransgenic mice developed HCC after initial treatment
with diethylnitrosamine
Kamegaya
et al.
(2005)44
Abbreviation: HCC, hepatocellular carcinoma.
IFN‑α were found using an animal model 10 years ago59
and verified by a randomized controlled trial, in which
IFN‑α treatment prolonged overall survival for patients
after curative resection.60
Whether a tumor will undergo local and distant spread
is defined by determinants of the tumor cells such as proliferating activities and the ability of the tumor cells to
respond to growth and survival signals derived from its
microenvironment.61 Our animal model suggests that
the lung is the most common organ of distant meta
stasis from HCC,62 which corresponds with data from
the clinic.63 Three key factors account for the success of
this model. First, HCC cells with the highest metastatic
potential were selected and inoculated into a maximally
favorable microenvironment for metastatic behavior. To
this end, a histologically intact intrahepatic meta tasis
s
from an HBV-positive Chinese patient with HCC was
taken as the donor tumor to construct the LCI‑D20
model. Second, the donor tumor tissues were implanted
into the livers of recipient nude mice. This maneuver
ensures that the tumor has a similar histological environment to that inside the human body, which facilitates the
display of its metastatic behavior. Third, tumor subclones
were selected in vivo by several cycles of sampling lung
metastases derived from these orthotopic xenografts and
inoculating them into the livers of further nude mice.
This process favors the enrichment of tumor cells with
the greatest potential for spontaneous metastasis.
The LCI-D20 model system has been very useful for
studying the fundamental properties and practical problems of HCC. With regard to the long-standing debate
over ‘nature versus nurture’ as the driver of cancer meta
stasis, our clinical studies found that genetic changes
favoring metastasis (nature) had already occurred in
primary HCC tumors, even those at very early stages of
development.64 By contrast, studies in our animal models
have provided convincing evidence that environmental
factors favoring the selection of cell clones with higher
metastatic potentials (nurture) have a larger role than
early genetic changes in driving HCC cells to become
increasingly metastatic. Of note, this animal model
differs from the clinical situation, as HCC cells undergo
several cycles of optimized in vivo selection, which might
account for disparities between the mouse model and the
clinical picture in humans. HCC metastasis, therefore,
is likely to involve the evolutionary interplay of nature
and nurture.
Animal models of spontaneous HCC development
and metastasis can be used to study the mechanism
of HCC progression as well as the best mode of intervention. Futakuchi et al.65 have established a rat model
of in vivo HCC lung metastasis based on sequential
intraperitoneal injection of diethylnitrosamine and
administration of drinking water containing the carcino
gen N‑nitrosomorpholine for 16 weeks, by which time
all animals had developed HCC. By week 23, lung meta
stasis had occurred in 100% of these animals. A subsequent modification of this protocol produced a less
aggressive disease model, in which the rats survived for
a longer period and developed moderate lung metastasis,
making these animals easier to maintain and facilitating both delivery of treatments66 and study of the multi
step and multifactorial evolutionary process of HCC
lung metastasis.67
Experimental models of HCC metastasis are also very
useful for the study of the fundamental mechanisms of
cancer spread. In investigations focused on the character
istics of circulating tumor cells, Scatton et al.68 established
an experimental model of HCC metastasis, in which
the Mahlavu human HCC cell line was introduced into
NOD–SCID mice by subcapsular injection, tail vein injection or direct infection into bone marrow. These models
have produced some interesting findings. First, when
Mahlavu cells were injected into the liver sub apsular
c
region to construct an orthotopic HCC model, the
primary tumor continuously produced large numbers of
circulating tumor cells, in a manner dependent on tumor
size. Moreover, the circulating tumor cells remained
viable in the bloodstream for over 60 days without producing any observable metastasis in other organs. Second,
NATURE REVIEWS | GASTROENTEROLOGY HEPATOLOGY
© 2011 Macmillan Publishers Limited. All rights reserved
VOLUME 9 | JANUARY 2012 | 37
7. REVIEWS
a
b
Pulmonary alveoli
Type I
epithelial cell
HCC intrahepatic lesion
Endothelial
cell
Nude mice liver
LCI-D20: metastasis to liver, lung, lymph
Cell culture
MHCC97: liver and lung metastasis
Type II
epithelial cell
Basal lamina
Cell clone
MHCC97L: lung metastasis 40%
Hepatic veins
Central
veins
Lung
metastasis
Vena
cava
Hepatic sinusoid
Hepatic cord
In vivo selection
Round 3: HCCLM3
In vivo selection
Bile
canaliculi
Kupffer
cell
MHCC97H: lung metastasis 100%
Metastasis
Subcutaneous
tumor
Endothelial
cell
Round 6: HCCLM6
In vivo selection
Primary tumor
Liver tumor
Round 9: HCCLM9
Figure 2 | Theoretical basis for, and description of, a mouse model of HCC incorporating a variation in the propensity for lung metastasis. a | In
humans, a primary HCC tumor metastasizes to the lung via the bloodstream. Experimental models of HCC that employ orthotopic implantation of
intact tumor tissue into nude mice optimally mimic human primary HCC, as the tumor microenvironment is also transplanted, and are a good model
of metastasis because the liver and lung microenvironments create favorable conditions for the growth of metastatic cells. b | A stepwise model of
HCC lung metastasis was established by sequential transplantation and cell clone selection. MHCC97 cells contain heterogeneous
subpopulations. By cloning culture technique, two subclones designated as MHCC97L with 40% spontaneous lung metastasis rate, and MHCC97H
with 100% spontaneous lung metastasis rate, were derived from MHCC97 cells. MHCC97H cells were subjected to three, six and nine rounds of
in vivo pulmonary metastasis selection, to produce cells with increasing numbers of lung metastasis nodules and shorter nude mice survival.
This in vivo selection signifies the enrichment of metastasis-prone mechanisms. Abbreviation: HCC, hepatocellular carcinoma.
when Mahlavu cells were injected into the tail vein, most
tumor cells remained circulating in the bloodstream for
up to 120 days, albeit without producing any increase in
secondary metastases. Third, when directly injected into
the bone marrow, the Mahlavu cells stayed at the injection
site where they proliferated but showed little tendency to
circulate in the blood or metastasize. Subsequent experiments using these cells and similar protocols confirmed
that circulating Mahlavu cells mainly originated from
the primary liver tumor, and that the number of circulating cells was directly proportional to the primary tumor
size.69 From this series of experiments, the key message
of academic and clinical importance is that the primary
tumor is the major source of circulating tumor cells,
which can remain viable in the bloodstream for an unexpectedly long time unless the primary tumor is brought
under effective control (for example, by hepatectomy,
which considerably reduces the number of circulating
tumor cells) or the host defense mechanism is powerful
enough to curb the spread of tumor cells.
Models of HCC treatment
The only potentially curative options for patients with
HCC are partial hepatectomy (resection) or liver transplantation. However, most patients with HCC are not
eligible for resection or transplantation owing to the
presence of advanced disease, and these individuals have
a poor prognosis (1-year survival of approximately 17.5%
38 | JANUARY 2012 | VOLUME 9
and 2‑year survival of 7.3%).70 In addition, even after
resection, the recurrence rate of HCC remains high, which
leads to poor cure rates and poor long-term survival.
Other treatments used in patients with HCC include
chemotherapy, radiotherapy, transarterial chemo
embolization (TACE), 71,72 radiofrequency ablation
(RFA), percutaneous alcohol injection73,74 and adjuvant
interferon therapy.75,76 In addition, various emerging
options, such as gene-based treatments and targeted
therapies, are under investigation as potential treatments
for HCC. Various animal models have been developed
for investigating the effects of each of these therapies.
Treatment modalities in clinical use
New chemotherapeutic agents
Most experiments to test the effects of potential drug
treatments in animal models of HCC involve the subcutaneous implantation of human hepatoma cells.
Although researchers have expressed doubts and criticisms about the validity of using effects on tumor xenografts to predict clinical activity,77 such human tumor
xenografts have proven useful in the development of
cytotoxic agents and mechanism-based cytostatic drugs
(drugs directed at specific abnormalities that drive the
malignant phenotype).78,79 A standard operating procedure should be followed for all xenograft experiments to
minimize the limitations of these models and maximize
their efficacy.78
www.nature.com/nrgastro
© 2011 Macmillan Publishers Limited. All rights reserved
8. REVIEWS
The National Cancer Institute has analyzed the usefulness of xenograft models in the development of cytotoxic drugs. Of the 33 agents that had cytotoxic activity
in more than one-third of xenograft models tested, 15
(45%) were later proven to be clinically active, and 10—
metho rexate, chlorambucil, 5‑fluorouracil, cisplatin,
t
paclitaxel, vinblastine, irinotecan, docetaxel, doxorubicin
and cyclophosphamide—were subsquently developed
into the now ‘standard’ anticancer drugs.80
A subcutaneous xenograft HCC model was used for
the evaluation of chemotherapeutic agents by Huynh
et al.,81 who established seven different primary HCC
cell lines and corresponding subcutaneous xenograft
models. Several key signaling pathways such as the Raf–
mitogen-activated protein kinase–extracellular signal
regulated kinase (Raf–MAPK–ERK) signaling pathway
involved in HCC development and progression were
elucidated in these models, which also provided valuable information for the design of molecular targeted
agents. For instance, this model system has been used to
assess the ability of small molecules, acting either alone
or in combination with chemotherapeutic and biologic
agents, to target these key signaling pathways in HCC.
Small molecule inhibitors and combinations of agents
that act on the Raf–MAPK–ERK pathway that have been
investigated using these models include AZD6244 plus
doxorubicin,82 bevacizumab plus rapamycin,83 brivanib
alaninate, 84 everolimus, 85 sunitinib, 86 sorafenib plus
rapamycin,87 AZD6244 plus rapamycin88 and AZD6244
plus sorafenib.89 These studies provide strong evidence
to support clinical investigations of these drugs and all
are currently part of phase II clinical trails in patients
with HCC.79,90
In terms of replicating the tumor microenvironment
and organ selectivity of human HCC, an orthopic model
is superior to subcutaneous xenograft models (Box 2).
Establishing high-quality orthotopic models is, however,
technically more challenging than the construction of
subcutaneous xenograft models. Conventional techniques of intrahepatic tumor implantation involve direct
placement of tumor fragments or injection of free tumor
cells. These techniques have the major disadvantage of
possible inadvertent tumor seeding along the needle
track or into the bloodstream, which could considerably
compromise the validity of studies of treatment efficacy.
To avoid such problems, Yang et al. 91 developed
a modi ied surgical technique, in which a piece of
f
Gelfoam ® (Pharmacia Upjohn Company, North
Peapack, USA) is inserted into the liver incision after
delivery of HCC cells. The Gelfoam® both facilitates
hemostasis and forms a pocket that secures the injected
tumor cells. This modified orthotopic model fully displays the progression of HCC from local tumor growth,
through adjacent organ invasion, ascites, and eventually
spontaneous pulmonary metastasis. The most prominent feature of this model is the substantially reduced
rate of early pulmonary metastasis compared with that
in models based on direct intrahepatic implantation of
either tumor cells or tumor fragments. This technical
modification could, therefore, help to avoid artificial
Box 2 | Advantages of orthotopic over subcutaneous models of HCC
■■ Maximum mimicry of clinical settings, including tumor location, liver damage
and biochemical changes
■■ Allow expression of specific genes and proteins
■■ Allow the development of advanced and metastatic disease
■■ Support an interaction between the tumor and host, in particular between
tumor cells and microenvironment
■■ Generate the possibility for testing liver-directed hepatocellular carcinoma
therapy
Abbreviation: HCC, hepatocellular carcinoma.
metastasis. The rat HCC model of Yang et al.91 has been
successfully used to evaluate several molecular targeted
drugs, including the mTOR inhibitor, sirolimus, and the
vascular epidermal growth factor receptor (VEGFR)
inhibitor, gefitinib, both of which can be used either
alone or in combination with the traditional cytotoxic
agent, doxorubicin.92–94
To reproduce the extensive liver disease that is associated with advanced HCC metastasis our group developed
another orthotopic mouse model. 95 HCC cells transfected with vectors carrying the gene for the β‑subunit
of human choriogonadotropin (β-hCG) were injected
into the left liver lobe of SCID mice. In this model, urine
levels of β‑hCG can be used as a surrogate marker of
tumor burden. This model supports the efficacy of treatments for advanced HCC based on an anti-angiogenic
drug combined with metronomic chemotherapy—a sustained, chronic and low-dose cancer chemotherapy—as
a survival benefit for the mice was only achieved when
the angiogenic drug and metronomic chemotherapy
were combined.95
HCC patients often also have liver cirrhosis, a feature
that is absent from most animal models of HCC. Schiffer
et al.96 have nonetheless established an experimental rat
model of cirrhosis that gives rise to HCC. Rats received
weekly intraperitoneal injections of diethylnitrosamine
for 16 weeks, followed by a 2‑week wash-out period
to allow recovery from acute necrosis. This treatment
caused cirrhosis in 14 weeks and led to multifocal HCC
in 18 weeks. The importance of this model is that it has
been used to demonstrate that gefitinib, which blocks
epidermal growth factor receptor (EGFR) activity, is
useful as a chemopreventive agent because it blocks
the transition from cirrhosis to HCC. Similarly, Huang
et al.97 used modified versions of this protocol to accelerate the development of rat HCC (from 16–18 weeks to
9–12 weeks). By adjusting the concentration of diethylnitrosamine solution in proportion to the body weight
of the animals, the animals could be induced to develop
either HCC alone, or HCC and liver cirrhosis simultaneously. This model could be suitable to evaluate the
effects of treatment strategies that target both cirrhosis
and HCC.
New TACE modalities
Although several animal models are available, that
described by Yang et al. is perhaps the most suitable for
NATURE REVIEWS | GASTROENTEROLOGY HEPATOLOGY
© 2011 Macmillan Publishers Limited. All rights reserved
VOLUME 9 | JANUARY 2012 | 39
9. REVIEWS
evaluating the efficacy of TACE for HCC treatment, as
these rats develop poorly differentiated tumors with a
hypervascular property.91 Qian et al.98 used this model
to investigate the therapeutic effect of TACE using polylactide-co-glycolide microspheres (PLCG), which have
an improved half-life and tissue compatibility compared with present embolic agents. By combining PLCG
TACE with mitomycin, the tumor growth rate decreased
more than eightfold. The same model was also used to
compare TACE alone with TACE combined with other
approaches, such as immunotherapy (OK‑432, an anti
tumor reagent with direct cytotoxic and cytostatic
activity) and antiangiogenic therapy (TNP‑470, which
selectively inhibit endothelial proliferation). Both the
combination therapies led to significantly retarded
tumor growth versus TACE alone.99
Investigational treatment modalities
Radiolabeled vesicles
In an effort to develop novel radiotherapy techniques
for HCC that have enhanced efficacy and reduced
radiation-induced liver disease, Vanpouille-Box et al.100
generated biomimetic lipid nanocapsules of 50 nm in
diameter loaded with 188Re. These nanocapsules can
penetrate deeply into tumor blood vessels because of
their nanometric scale. This study used a rat model of
diethylnitrosamine-induced HCC, which demonstrated
that administration of 188Re nanocapsules containing
a radiation dose of 80 mBq could improve the median
survival of treated animals by 100% and reduce tumor
mass by 50%, while keeping liver enzyme levels within
twofold of the upper limit of normal values. This study
has provided proof-of-principle evidence that tumorselective internal radiotherapy is a feasible strategy for
HCC treatment.
Gene therapy
Gene therapy might provide an alternative treatment
modality for established HCC. Graepler et al.101 transferred the genes for soluble vascular endothelial growth
factor (VEGF) receptor 1 (sFlt‑1) and endostatin into rat
Morris hepatoma (MH) cells, which secrete high levels of
VEGF but do not normally express sFlt‑1. MH cells engineered to express both sFlt‑1 and endostatin were then
injected subcutaneously into ACI rats, which blocked
the activity of VEGF and retarded tumor growth. These
results provide evidence that angiostatic gene therapy
might be a feasible strategy for the treatment of established HCC. Thereafter, several other gene therapy strategies were used to treat HCC in subcutaneous models,
including combined suicide/cytokine gene therapy
(HSV-TK/hIL‑2),102 human plasminogen fragment containing five kringle regions (Plgk1‑5),103 DC40 ligand
(CD40L)104 and TNF-related apoptosis-inducing ligand
(TRAIL) combined with cisplatin,105 all of which provide
potential treatement approaches for human HCC.
As the vascularization of rabbit liver tumors is similar
to that of human liver tumors, a rabbit VX2 tumor
model106 has been used in preclinical studies of liver
tumor imaging, chemotherapy and tumor etiology. Gu
40 | JANUARY 2012 | VOLUME 9
et al.107 developed a transarterially administered gene
therapy consisting of TACE and an adenoviral vector
carrying the p53 tumor suppressor gene, which showed
significant suppression of tumor growth in the orthotopic VX2 model. To evaluate the antitumor effects of
the liver-cancer-specific oncolytic adenovirus Ad5WS2
in vivo, Hsieh et al. 108 established a syngeneic HCC
model by orthotopic injection of ML‑1 mouse HCC cells.
Ad5WS2 significantly increased mice survival, compared
with control and liver-cancer-nonspecific adenovirustreated animals. Moreover, Ad5WS2-treated mice only
experienced a transient and slight increase in alanine
aminotransferase (ALT) levels, in contrast to a significantly longer and higher increase in ALT levels in livercancer-nonspecific adenovirus treated animals. This
study brings hope to the possibility of HCC-targeted
oncolytic gene therapy.
Irreversible electroporation
To investigate the feasibility of using irreversible electro
poration as a liver-directed ablation technique for the
treatment of HCC, Guo et al.109 established an orthotopic
rat model of HCC by injection of the N1‑S1 hepatoma
cell line into the hepatic capsule of the rat. Using serial
MRI scans and follow-up histopathological analyses
to study the effect, the authors found that irreversible
electro oration led to a reduction in tumor size of 32%
p
in one-dimensional maximum diameter, compared with
a 110% increase in untreated animals. No major adverse
effects were reported. The results suggest that irreversible electroporation could be a safe and effective targeted
ablation of liver tumors.
RNA interference
Therapies for HCC based on RNA interference (RNAi)
have shown promising preclinical results, and might be
developed into another potentially curative therapeutic
approach.110,111 However, almost all in vivo studies have
employed subcutaneous xenograft models to evaluate
the efficiency of RNAi-mediated HCC prevention and
therapy,112–114 which raises concerns that the findings do
not reflect the true clinical situation. This Review, therefore, focuses on findings in an orthotopic animal model
of HCC (Box 2). Lin et al.115 used an orthotopic model of
HCC to investigate the effect of an RNAi-based therapy
utilizing an antisense oligonucleotide (cantide) targeted
against human telomerase reverse transcriptase on tumor
growth in vivo. In this model, a highly metastatic tumor
(HCM‑Y89) derived from a human HCC surgical specimen was xenografted into nude mice. Compared with
controls, cantide could substantially reduce tumor weight
by up to 69%, reduce liver tumor relapse by up to 37.5%,
and reduce lung metastasis by up to 58%. This orthotopic
HCC model has also been employed to evaluate the anticancer effects of antisense oligonucleotides against survivin116 producing up to 61% tumor weight reduction,
and type I insulin-like growth factor receptor 117 producing up to 72% tumor growth inhibition and up to 50%
reduction in lung metastasis. Several unique features of
these studies merit further comment. First, the tumor
www.nature.com/nrgastro
© 2011 Macmillan Publishers Limited. All rights reserved
10. REVIEWS
xenografts consisted of pieces of previously frozen tumor
tissue, which were implanted into the left lobe of the livers
of recipient mice. The preservation of tumor tissue in
liquid nitrogen rather than as a cell line retains the tumor
microenvironment and, therefore, ensures that optimal
conditions for displaying the full range of the tumor’s
biological behaviors are maintained.77 Second, using an
orthotopic rather than a subcutaneous xenograft model
of HCC makes the study design as close to the clinical
situation as possible, thereby increasing a study’s credibility. Third, this model enables detailed investigation of
major issues relevant to HCC treatment, including reductions in the size of the primary tumor, decreases in postoperative tumor recurrence and pulmonary metastasis,
and decreases in serum AFP levels. These studies provide
proof-of-principle evidence that RNAi-based therapy is a
promising strategy for HCC treatment.
Conclusions
Animal models of HCC have contributed to our
improved understanding of liver carcinogenesis and
progression, as well as to the design of comprehensive
treatment strategies. From the HBV and HCV transgenic mouse models described in this Review, several
features are clear. First, tumor development is slower
in models based on HBV or HCV gene transfer alone
than in models based on transfer of HCV or HBV genes
in combination with other genes or chemical exposure.
Second, HBV and HCV transgenic mice do not develop
liver cirrhosis, suggesting that this symptom observed in
patients with HCC could be attributed to factors other
than the virus itself. Third, ROS generation and steatosis have a major role in the development of HCC, but
1.
Jemal, A. et al. Global cancer statistics. CA
Cancer J. Clin. 61, 69–90 (2011).
2. Parkin, D. M. The global health burden of
infection-associated cancers in the year 2002.
Int. J. Cancer 118, 3030–3044 (2006).
3. Ming, L. et al. Dominant role of hepatitis B virus
and cofactor role of aflatoxin in
hepatocarcinogenesis in Qidong, China.
Hepatology 36, 1214–1220 (2002).
4. El-Serag, H. B. Mason, A. C. Rising incidence of
hepatocellular carcinoma in the United States.
N. Engl. J. Med. 340, 745–750 (1999).
5. El-Serag, H. B. Epidemiology of hepatocellular
carcinoma in USA. Hepatol. Res. 37 (Suppl. 2),
S88–S94 (2007).
6. Tsai, W. L. Chung, R. T. Viral
hepatocarcinogenesis. Oncogene 29,
2309–2324 (2010).
7. Perz, J. F., Armstrong, G. L., Farrington, L. A.,
Hutin, Y. J. Bell, B. P The contributions of
.
hepatitis B virus and hepatitis C virus infections
to cirrhosis and primary liver cancer worldwide.
J. Hepatol. 45, 529–538 (2006).
8. Chen, C. J. et al. Risk of hepatocellular carcinoma
across a biological gradient of serum hepatitis B
virus DNA level. JAMA 295, 65–73 (2006).
9. Liang, T. J. Heller, T. Pathogenesis of
hepatitis C‑associated hepatocellular carcinoma.
Gastroenterology 127, S62–S71 (2004).
10. Heindryckx, F., Colle, I. Van Vlierberghe, H.
Experimental mouse models for hepatocellular
carcinoma research. Int. J. Exp. Pathol. 90,
367–386 (2009).
this might not be due to inflammatory cell infiltration.
These features suggest that the virus itself could both initiate and promote carcinogenesis, whereas other factors,
including exposure to carcinogens, have a secondary
role (Figure 1). Thus, HBV and HCV transgenic mouse
models provide plausible evidence that a one-hit mechanism of carcinogenesis could be the predominant pattern
of HCC development.
In the era of molecular medicine, increasing attention
has been focused on the identification of key pathways
and mediators to enable the development of targeted and
individualized cancer treatments. In the rapidly evolving
field of HCC model construction, cutting-edge technologies, such as proteomics (and various other ‘omics’ techniques), RNAi, microRNA and molecular imaging will
be used to establish target-specific or signal-pathwayspecific models, for the study of disease mechanisms
and to pinpoint treatment in the era of individualized
medicine. Such models are expected to be the major
future direction of HCC study. Meanwhile, technical
specifications and unified procedures are important
challenges for the establishment of stable yet dynamic
animal models of HCC.
Review criteria
We searched for articles focusing on original research into
animal models of HCC, with a particular emphasis on their
potential application in HCC development, metastasis
and treatment. A PubMed search was performed using
the search terms “animal model” and “hepatocellular
carcinoma”. All papers identified were English-language
full-text papers. We also searched the reference lists of
identified articles for further relevant papers.
11. Wu, L., Tang, Z. Y. Li, Y. Experimental models of
hepatocellular carcinoma: developments and
evolution. J. Cancer Res. Clin. Oncol. 135,
969–981 (2009).
12. Fausto, N. Campbell, J. S. Mouse models of
hepatocellular carcinoma. Semin. Liver Dis. 30,
87–98 (2010).
13. Aravalli, R. N., Steer, C. J., Sahin, M. B.
Cressman, E. N. Stem cell origins and animal
models of hepatocellular carcinoma. Dig. Dis.
Sci. 55, 1241–1250 (2010).
14. Kalra, N. Kumar, V. c‑Fos is a mediator of the
c‑myc‑induced apoptotic signaling in serumdeprived hepatoma cells via the p38 mitogenactivated protein kinase pathway. J. Biol. Chem.
279, 25313–25319 (2004).
15. Singh, M. Kumar, V. Transgenic mouse models
of hepatitis B virus-associated hepatocellular
carcinoma. Rev. Med. Virol. 13, 243–253 (2003).
16. Murata, M. et al. Hepatitis B virus X protein
shifts human hepatic transforming growth factor
(TGF)-beta signaling from tumor suppression to
oncogenesis in early chronic hepatitis B.
Hepatology 49, 1203–1217 (2009).
17. Gearhart, T. L. Bouchard, M. J. The hepatitis B
virus X protein modulates hepatocyte
proliferation pathways to stimulate viral
replication. J. Virol. 84, 2675–2686 (2010).
18. Zhao, J. et al. Epigenetic silence of
ankyrin‑repeat‑containing,
SH3‑domain‑containing, and proline‑rich‑regioncontaining protein 1 (ASPP1) and ASPP2 genes
promotes tumor growth in hepatitis B virus-
NATURE REVIEWS | GASTROENTEROLOGY HEPATOLOGY
© 2011 Macmillan Publishers Limited. All rights reserved
19.
20.
21.
22.
23.
24.
25.
26.
positive hepatocellular carcinoma. Hepatology
51, 142–153 (2010).
Cheng, B., Zheng, Y., Guo, X., Wang, Y. Liu, C.
Hepatitis B viral X protein alters the biological
features and expressions of DNA repair
enzymes in LO2 cells. Liver Int. 30, 319–326
(2010).
Kim, C. M., Koike, K., Saito, I., Miyamura, T.
Jay, G. HBx gene of hepatitis B virus induces
liver cancer in transgenic mice. Nature 351,
317–320 (1991).
Yu, D. Y. et al. Incidence of hepatocellular
carcinoma in transgenic mice expressing the
hepatitis B virus X‑protein. J. Hepatol. 31,
123–132 (1999).
Kim, S. Y. et al. Proteomic analysis of liver tissue
from HBx-transgenic mice at early stages of
hepatocarcinogenesis. Proteomics 9,
5056–5066 (2009).
Cui, F. et al. The up-regulation of proteasome
subunits and lysosomal proteases in
hepatocellular carcinomas of the HBx gene
knockin transgenic mice. Proteomics 6,
498–504 (2006).
Wang, Y. et al. HBsAg and HBx knocked into the
p21 locus causes hepatocellular carcinoma in
mice. Hepatology 39, 318–324 (2004).
Knudson, A. G. Jr. Mutation and cancer:
statistical study of retinoblastoma. Proc. Natl
Acad. Sci. USA 68, 820–823 (1971).
Huebner, R. J. Todaro, G. J. Oncogenes of RNA
tumor viruses as determinants of cancer. Proc.
Natl Acad. Sci. USA 64, 1087–1094 (1969).
VOLUME 9 | JANUARY 2012 | 41
11. REVIEWS
27. Lakhtakia, R. et al. Hepatocellular carcinoma in
a hepatitis B ‘x’ transgenic mouse model:
a sequential pathological evaluation.
J. Gastroenterol. Hepatol. 18, 80–91 (2003).
28. Dunsford, H. A., Sell, S. Chisari, F. V.
Hepatocarcinogenesis due to chronic liver cell
injury in hepatitis B virus transgenic mice.
Cancer Res. 50, 3400–3407 (1990).
29. Chisari, F. V. et al. A transgenic mouse model of
the chronic hepatitis B surface antigen carrier
state. Science 230, 1157–1160 (1985).
30. Chisari, F. V. et al. Structural and pathological
effects of synthesis of hepatitis B virus large
envelope polypeptide in transgenic mice. Proc.
Natl Acad. Sci. USA 84, 6909–6913 (1987).
31. Toshkov, I., Chisari, F. V. Bannasch, P. Hepatic
preneoplasia in hepatitis B virus transgenic
mice. Hepatology 20, 1162–1172 (1994).
32. Huang, S. N. Chisari, F. V. Strong, sustained
hepatocellular proliferation precedes
hepatocarcinogenesis in hepatitis B surface
antigen transgenic mice. Hepatology 21,
620–626 (1995).
33. Barone, M. et al. Gene expression analysis in
HBV transgenic mouse liver: a model to study
early events related to hepatocarcinogenesis.
Mol. Med. 12, 115–123 (2006).
34. Nakamoto, Y., Guidotti, L. G., Kuhlen, C. V.,
Fowler, P. Chisari, F. V. Immune pathogenesis
of hepatocellular carcinoma. J. Exp. Med. 188,
341–350 (1998).
35. Su, S. B. et al. Overexpression of p8 is
inversely correlated with apoptosis in
pancreatic cancer. Clin. Cancer Res. 7,
1320–1324 (2001).
36. Ray, R. et al. BNIP3 heterodimerizes with Bcl‑2/
Bcl‑X(L) and induces cell death independent of
a Bcl‑2 homology 3 (BH3) domain at both
mitochondrial and nonmitochondrial sites.
J. Biol. Chem. 275, 1439–1448 (2000).
37. Sell, S., Hunt, J. M., Dunsford, H. A.
Chisari, F. V. Synergy between hepatitis B virus
expression and chemical hepatocarcinogens in
transgenic mice. Cancer Res. 51, 1278–1285
(1991).
38. Koike, K., Moriya, K. Matsuura, Y. Animal
models for hepatitis C and related liver
disease. Hepatol. Res. 40, 69–82 (2010).
39. Koike, K. et al. Expression of hepatitis C virus
envelope proteins in transgenic mice. J. Gen.
Virol. 76 (Pt 12), 3031–3038 (1995).
40. Moriya, K. et al. The core protein of hepatitis C
virus induces hepatocellular carcinoma in
transgenic mice. Nat. Med. 4, 1065–1067
(1998).
41. Koike, K., Moriya, K. Kimura, S. Role of
hepatitis C virus in the development of
hepatocellular carcinoma: transgenic approach
to viral hepatocarcinogenesis. J. Gastroenterol.
Hepatol. 17, 394–400 (2002).
42. Ichibangase, T., Moriya, K., Koike, K. Imai, K.
A proteomics method revealing disease-related
proteins in livers of hepatitis-infected mouse
model. J. Proteome Res. 6, 2841–2849 (2007).
43. Lerat, H. et al. Steatosis and liver cancer in
transgenic mice expressing the structural and
nonstructural proteins of hepatitis C virus.
Gastroenterology 122, 352–365 (2002).
44. Kamegaya, Y. et al. Hepatitis C virus acts as a
tumor accelerator by blocking apoptosis in a
mouse model of hepatocarcinogenesis.
Hepatology 41, 660–667 (2005).
45. Li, Y. et al. Stepwise metastatic human
hepatocellular carcinoma cell model system
with multiple metastatic potentials established
through consecutive in vivo selection and
studies on metastatic characteristics. J. Cancer
Res. Clin. Oncol. 130, 460–468 (2004).
42 | JANUARY 2012 | VOLUME 9
46. Sun, F. X. et al. Metastatic models of human liver
cancer in nude mice orthotopically constructed
by using histologically intact patient specimens.
J. Cancer Res. Clin. Oncol. 122, 397–402 (1996).
47. Tian, J. et al. New human hepatocellular
carcinoma (HCC) cell line with highly metastatic
potential (MHCC97) and its expressions of the
factors associated with metastasis. Br. J. Cancer
81, 814–821 (1999).
48. Li, Y. et al. Establishment of cell clones with
different metastatic potential from the
metastatic hepatocellular carcinoma cell line
MHCC97. World J. Gastroenterol. 7, 630–636
(2001).
49. Li, Y. et al. Establishment of a hepatocellular
carcinoma cell line with unique metastatic
characteristics through in vivo selection and
screening for metastasis-related genes through
cDNA microarray. J. Cancer Res. Clin. Oncol. 129,
43–51 (2003).
50. Ding, S. J. et al. From proteomic analysis to
clinical significance: overexpression of
cytokeratin 19 correlates with hepatocellular
carcinoma metastasis. Mol. Cell. Proteomics 3,
73–81 (2004).
51. Andersen, J. B. et al. Progenitor-derived
hepatocellular carcinoma model in the rat.
Hepatology 51, 1401–1409 (2010).
52. Shi, Y. H. et al. Expression of X‑linked
inhibitor‑of‑apoptosis protein in hepatocellular
carcinoma promotes metastasis and tumor
recurrence. Hepatology 48, 497–507 (2008).
53. Bai, D. S. et al. Capn4 overexpression underlies
tumor invasion and metastasis after liver
transplantation for hepatocellular carcinoma.
Hepatology 49, 460–470 (2009).
54. Gao, Q. et al. Overexpression of PD‑L1
significantly associates with tumor
aggressiveness and postoperative recurrence in
human hepatocellular carcinoma. Clin. Cancer
Res. 15, 971–979 (2009).
55. Yang, X. R. et al. CD24 is a novel predictor for
poor prognosis of hepatocellular carcinoma after
surgery. Clin. Cancer Res. 15, 5518–5527
(2009).
56. Shi, G. M. et al. CD151 modulates expression of
matrix metalloproteinase 9 and promotes
neoangiogenesis and progression of
hepatocellular carcinoma. Hepatology 52,
183–196 (2010).
57. Liu, L. et al. Activation of β‑catenin by hypoxia in
hepatocellular carcinoma contributes to
enhanced metastatic potential and poor
prognosis. Clin. Cancer Res. 16, 2740–2750
(2010).
58. Yang, Z. F. et al. Significance of CD90+ cancer
stem cells in human liver cancer. Cancer Cell 13,
153–166 (2008).
59. Wang, L. et al. High-dose and long-term therapy
with interferon-alpha inhibits tumor growth and
recurrence in nude mice bearing human
hepatocellular carcinoma xenografts with high
metastatic potential. Hepatology 32, 43–48
(2000).
60. Sun, H. C. et al. Postoperative interferon alpha
treatment postponed recurrence and improved
overall survival in patients after curative
resection of HBV-related hepatocellular
carcinoma: a randomized clinical trial. J. Cancer
Res. Clin. Oncol. 132, 458–465 (2006).
61. Paget, S. The distribution of secondary growths
in cancer of the breast. 1889. Cancer Metastasis
Rev. 8, 98–101 (1989).
62. Tang, Z. Y. et al. A decade’s studies on
metastasis of hepatocellular carcinoma.
J. Cancer Res. Clin. Oncol. 130, 187–196 (2004).
63. Yuki, K., Hirohashi, S., Sakamoto, M., Kanai, T.
Shimosato, Y. Growth and spread of
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
hepatocellular carcinoma. A review of 240
consecutive autopsy cases. Cancer 66,
2174–2179 (1990).
Ye, Q. H. et al. Predicting hepatitis B viruspositive metastatic hepatocellular carcinomas
using gene expression profiling and supervised
machine learning. Nat. Med. 9, 416–423
(2003).
Futakuchi, M. et al. Establishment of an in vivo
highly metastatic rat hepatocellular carcinoma
model. Jpn J. Cancer Res. 90, 1196–1202
(1999).
Futakuchi, M., Ogawa, K., Tamano, S.,
Takahashi, S. Shirai, T. Suppression of
metastasis by nuclear factor kappaB inhibitors
in an in vivo lung metastasis model of
chemically induced hepatocellular carcinoma.
Cancer Sci. 95, 18–24 (2004).
Yoshino, H. et al. Modification of an in vivo lung
metastasis model of hepatocellular carcinoma
by low dose N.‑nitrosomorpholine and
diethylnitrosamine. Clin. Exp. Metastasis 22,
441–447 (2005).
Scatton, O. et al. Fate and characterization of
circulating tumor cells in a NOD/SCID mouse
model of human hepatocellular carcinoma.
Oncogene 25, 4067–4075 (2006).
Scatton, O. et al. Generation and modulation of
hepatocellular carcinoma circulating cells: a new
experimental model. J. Surg. Res. 150, 183–189
(2008).
Cabibbo, G. et al. A meta-analysis of survival
rates of untreated patients in randomized
clinical trials of hepatocellular carcinoma.
Hepatology 51, 1274–1283 (2010).
Zhong, J. H. Li, L. Q. Postoperative adjuvant
transarterial chemoembolization for participants
with hepatocellular carcinoma: a meta-analysis.
Hepatol. Res. 40, 943–953 (2010).
Wang, W., Shi, J. Xie, W. F. Transarterial
chemoembolization in combination with
percutaneous ablation therapy in unresectable
hepatocellular carcinoma: a meta-analysis. Liver
Int. 30, 741–749 (2010).
Zhou, Y. et al. Meta-analysis of radiofrequency
ablation versus hepatic resection for small
hepatocellular carcinoma. BMC Gastroenterol.
10, 78 (2010).
Germani, G. et al. Clinical outcomes of
radiofrequency ablation, percutaneous alcohol
and acetic acid injection for hepatocelullar
carcinoma: a meta-analysis. J. Hepatol. 52,
380–388 (2010).
Shen, Y. C. et al. Adjuvant interferon therapy
after curative therapy for hepatocellular
carcinoma (HCC): a meta-regression approach.
J. Hepatol. 52, 889–894 (2010).
Singal, A. K., Freeman, D. H. Jr Anand, B. S.
Meta-analysis: interferon improves outcomes
following ablation or resection of hepatocellular
carcinoma. Aliment. Pharmacol. Ther. 32,
851–858 (2010).
Newell, P Villanueva, A., Friedman, S. L.,
.,
Koike, K. Llovet, J. M. Experimental models of
hepatocellular carcinoma. J. Hepatol. 48,
858–879 (2008).
Kelland, L. R. Of mice and men: values and
liabilities of the athymic nude mouse model in
anticancer drug development. Eur. J. Cancer 40,
827–836 (2004).
Newell, P Villanueva, A. Llovet, J. M.
.,
Molecular targeted therapies in hepatocellular
carcinoma: from pre-clinical models to clinical
trials. J. Hepatol. 49, 1–5 (2008).
Johnson, J. I. et al. Relationships between drug
activity in NCI preclinical in vitro and in vivo
models and early clinical trials. Br. J. Cancer 84,
1424–1431 (2001).
www.nature.com/nrgastro
© 2011 Macmillan Publishers Limited. All rights reserved
12. REVIEWS
81. Huynh, H., Soo, K. C., Chow, P. K., Panasci, L.
Tran, E. Xenografts of human hepatocellular
carcinoma: a useful model for testing drugs.
Clin. Cancer Res. 12, 4306–4314 (2006).
82. Huynh, H., Chow, P. K. Soo, K. C. AZD6244
and doxorubicin induce growth suppression
and apoptosis in mouse models of
hepatocellular carcinoma. Mol. Cancer Ther. 6,
2468–2476 (2007).
83. Huynh, H. et al. Bevacizumab and rapamycin
induce growth suppression in mouse models of
hepatocellular carcinoma. J. Hepatol. 49,
52–60 (2008).
84. Huynh, H. et al. Brivanib alaninate, a dual
inhibitor of vascular endothelial growth factor
receptor and fibroblast growth factor receptor
tyrosine kinases, induces growth inhibition in
mouse models of human hepatocellular
carcinoma. Clin. Cancer Res. 14, 6146–6153
(2008).
85. Huynh, H. et al. RAD001 (everolimus) inhibits
tumour growth in xenograft models of human
hepatocellular carcinoma. J. Cell. Mol. Med. 13,
1371–1380 (2009).
86. Huynh, H. et al. Sunitinib (SUTENT, SU11248)
suppresses tumor growth and induces
apoptosis in xenograft models of human
hepatocellular carcinoma. Curr. Cancer Drug
Targets 9, 738–747 (2009).
87. Huynh, H. et al. Sorafenib and rapamycin
induce growth suppression in mouse models of
hepatocellular carcinoma. J. Cell. Mol. Med. 13,
2673–2683 (2009).
88. Huynh, H. AZD6244 (ARRY‑142886) enhances
the antitumor activity of rapamycin in mouse
models of human hepatocellular carcinoma.
Cancer 116, 1315–1325 (2010).
89. Huynh, H. et al. AZD6244 enhances the antitumor activity of sorafenib in ectopic and
orthotopic models of human hepatocellular
carcinoma (HCC). J. Hepatol. 52, 79–87
(2010).
90. Park, J. W. et al. Phase II, open-label study of
brivanib as first-line therapy in patients with
advanced hepatocellular carcinoma. Clin.
Cancer Res. 17, 1973–1983 (2011).
91. Yang, R. et al. A reproducible rat liver cancer
model for experimental therapy: introducing a
technique of intrahepatic tumor implantation.
J. Surg. Res. 52, 193–198 (1992).
92. Semela, D. et al. Vascular remodeling and
antitumoral effects of mTOR inhibition in a rat
model of hepatocellular carcinoma. J. Hepatol.
46, 840–848 (2007).
93. Piguet, A. C. et al. Inhibition of mTOR in
combination with doxorubicin in an
experimental model of hepatocellular
carcinoma. J. Hepatol. 49, 78–87 (2008).
94. Piguet, A. C. et al. Everolimus augments the
effects of sorafenib in a syngeneic orthotopic
model of hepatocellular carcinoma. Mol. Cancer
Ther. 10, 1007–1017 (2011).
95. Tang, T. C., Man, S., Lee, C. R., Xu, P
.
Kerbel, R. S. Impact of metronomic UFT/
cyclophosphamide chemotherapy and
antiangiogenic drug assessed in a new
preclinical model of locally advanced orthotopic
hepatocellular carcinoma. Neoplasia 12,
264–274 (2010).
96. Schiffer, E. et al. Gefitinib, an EGFR inhibitor,
prevents hepatocellular carcinoma development
in the rat liver with cirrhosis. Hepatology 41,
307–314 (2005).
97. Huang, K. W. et al. Dual therapeutic effects of
interferon‑α gene therapy in a rat hepatocellular
carcinoma model with liver cirrhosis. Mol. Ther.
16, 1681–1687 (2008).
98. Qian, J. et al. Application of
poly‑lactide‑co‑glycolide‑microspheres in the
transarterial chemoembolization in an animal
model of hepatocellular carcinoma. World J.
Gastroenterol. 9, 94–98 (2003).
99. Maataoui, A. et al. Transarterial
chemoembolization alone and in combination
with other therapies: a comparative study in an
animal HCC model. Eur. Radiol. 15, 127–133
(2005).
100. Vanpouille-Box, C. et al. Lipid nanocapsules
loaded with rhenium‑188 reduce tumor
progression in a rat hepatocellular carcinoma
model. PLoS ONE 6, e16926 (2011).
101. Graepler, F. et al. Combined endostatin/sFlt‑1
antiangiogenic gene therapy is highly effective in
a rat model of HCC. Hepatology 41, 879–886
(2005).
102. Stefani, A. L. et al. Systemic efficacy of
combined suicide/cytokine gene therapy in a
murine model of hepatocellular carcinoma.
J. Hepatol. 42, 728–735 (2005).
103. Schmitz, V. et al. Plasminogen fragment K1–5
improves survival in a murine hepatocellular
carcinoma model. Gut 56, 271–278 (2007).
104. Iida, T. et al. Adenovirus-mediated CD40L gene
therapy induced both humoral and cellular
immunity against rat model of hepatocellular
carcinoma. Cancer Sci. 99, 2097–2103 (2008).
105. Wang, Y. et al. The efficacy of combination
therapy using adeno-associated virus-TRAIL
targeting to telomerase activity and cisplatin in a
mice model of hepatocellular carcinoma.
J. Cancer Res. Clin. Oncol. 136, 1827–1837
(2010).
106. Ramirez, L. H. et al. Pharmacokinetics and
antitumor effects of mitoxantrone after
intratumoral or intraarterial hepatic
administration in rabbits. Cancer Chemother.
Pharmacol. 37, 371–376 (1996).
107. Gu, T. et al. Trans-arterial gene therapy for
hepatocellular carcinoma in a rabbit model.
World J. Gastroenterol. 13, 2113–2117 (2007).
NATURE REVIEWS | GASTROENTEROLOGY HEPATOLOGY
© 2011 Macmillan Publishers Limited. All rights reserved
108. Hsieh, J. L. et al. Transthyretin-driven oncolytic
adenovirus suppresses tumor growth in
orthotopic and ascites models of hepatocellular
carcinoma. Cancer Sci. 100, 537–545 (2009).
109. Guo, Y. et al. Irreversible electroporation therapy
in the liver: longitudinal efficacy studies in a rat
model of hepatocellular carcinoma. Cancer Res.
70, 1555–1563 (2010).
110. Romano, P
. R., McCallus, D. E. Pachuk, C. J.
RNA interference-mediated prevention and
therapy for hepatocellular carcinoma. Oncogene
25, 3857–3865 (2006).
111. Arbuthnot, P Thompson, L. J. Harnessing the
.
RNA interference pathway to advance treatment
and prevention of hepatocellular carcinoma.
World J. Gastroenterol. 14, 1670–1681 (2008).
112. Li, H. et al. Use of adenovirus-delivered siRNA to
target oncoprotein p28GANK in hepatocellular
carcinoma. Gastroenterology 128, 2029–2041
(2005).
113. Cho-Rok, J. et al. Adenovirus-mediated transfer
of siRNA against PTTG1 inhibits liver cancer cell
growth in vitro and in vivo. Hepatology 43,
1042–1052 (2006).
114. Salvi, A., Arici, B., Alghisi, A., Barlati, S.
De Petro, G. RNA interference against urokinase
in hepatocellular carcinoma xenografts in nude
mice. Tumour Biol. 28, 16–26 (2007).
115. Lin, R. X., Tuo, C. W., Lu, Q. J., Zhang, W.
Wang, S. Q. Inhibition of tumor growth and
metastasis with antisense oligonucleotides
(Cantide) targeting hTERT in an in situ human
hepatocellular carcinoma model. Acta
Pharmacol. Sin. 26, 762–768 (2005).
116. Sun, Y., Lin, R., Dai, J., Jin, D. Wang, S. Q.
Suppression of tumor growth using antisense
oligonucleotide against survivin in an orthotopic
transplant model of human hepatocellular
carcinoma in nude mice. Oligonucleotides 16,
365–374 (2006).
117. Lin, R. X. et al. Inhibition of hepatocellular
carcinoma growth by antisense oligonucleotides
to type I insulin-like growth factor receptor
in vitro and in an orthotopic model. Hepatol. Res.
37, 366–375 (2007).
Acknowledgments
The authors receive funding from the Science Fund for
Creative Research Groups of the National Natural
Science Foundation of China (No. 20921062), and
the Fundamental Research Funds for the Central
Universities of Ministry of Education of China (No.
4103005; both to Y. Li).
Author contributions
Y. Li, Z.‑Y. Tang and J.‑X. Hou jointly researched data
for the article, wrote the manuscript, and made
substantial contributions to discussions of the
content. In addition, Z.‑Y. Tang reviewed and edited
the manuscript before submission.
VOLUME 9 | JANUARY 2012 | 43