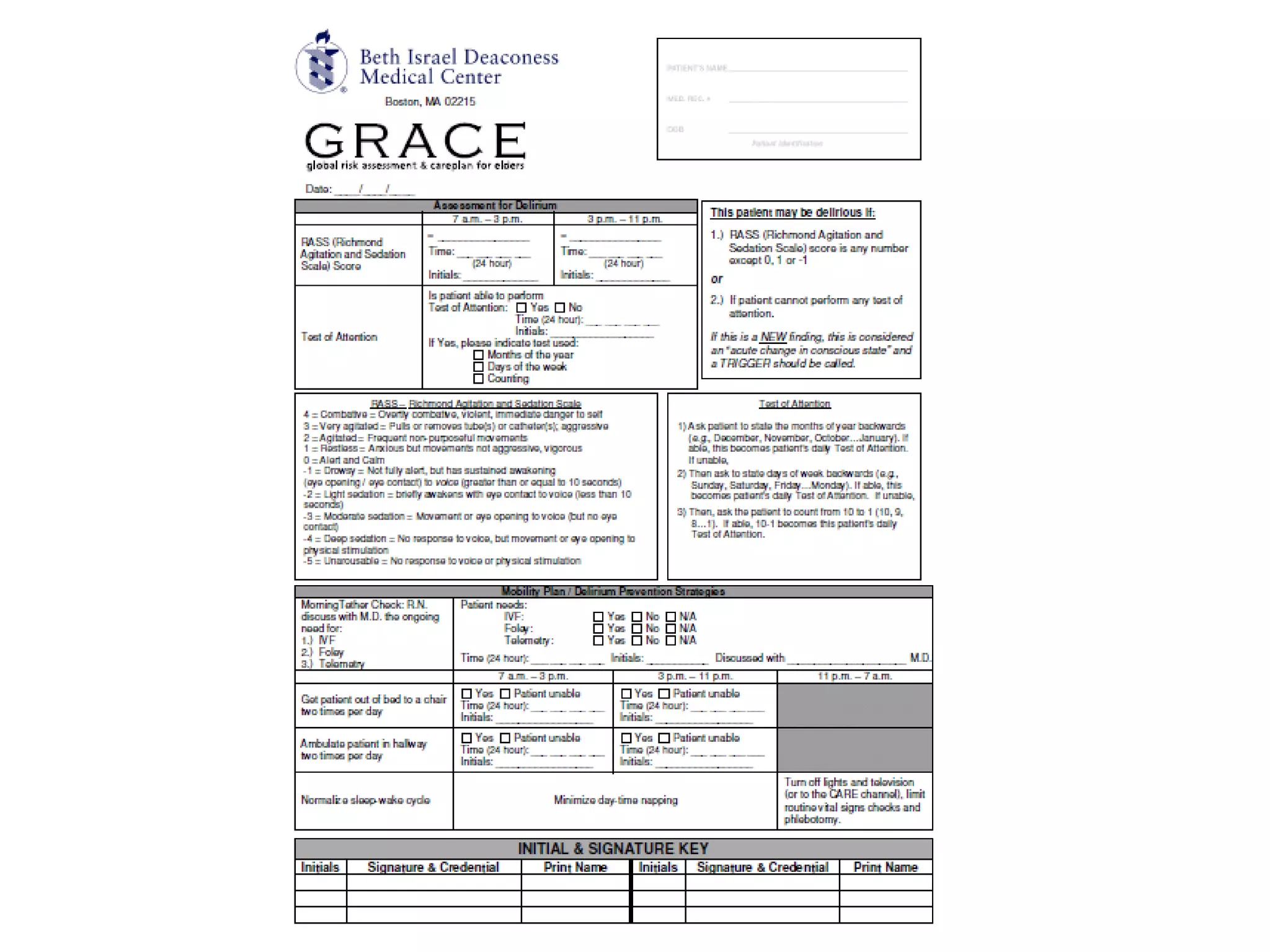
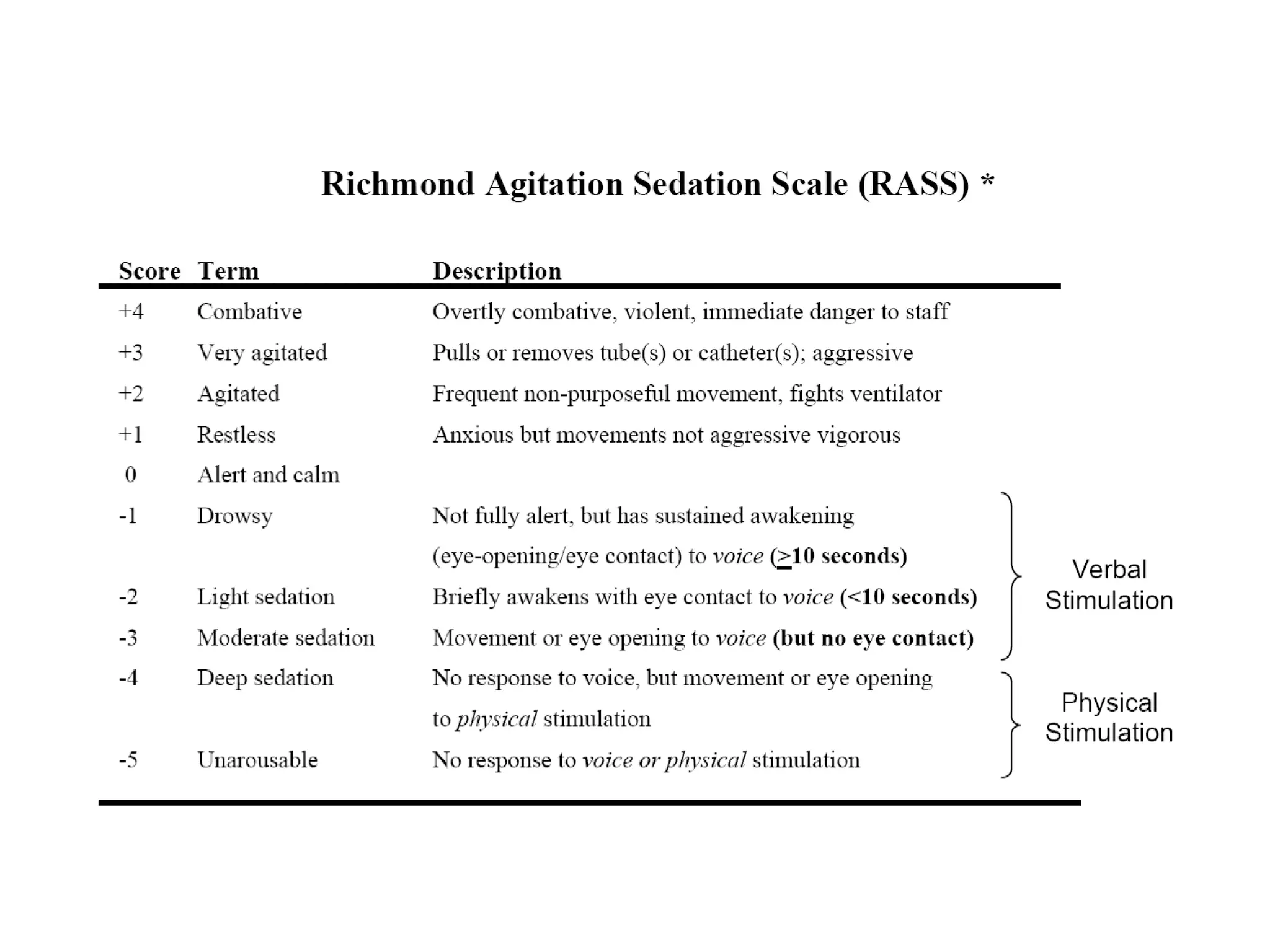
The Grace Initiative aims to address the unique concerns of vulnerable elderly patients in hospitals by identifying and preventing delirium, maintaining function, and optimizing resources. It includes a three-pronged approach focusing on bedside assessment, mobility protocols, and a sleep protocol, specifically designed for patients aged 80 and older. Nurses will play a central role in implementing this program, utilizing the bedside Grace flow sheet for daily assessments and monitoring.









![Thank you! Melissa Mattison, MD [email_address] Pager 90141 Angela Botts, MD [email_address] Pager 31458 Daniele Olveczky, MD [email_address] Pager 38743 Julie Moran, MD jamoran @bidmc.harvard.edu Pager 33000 Christine Kristeller, RN [email_address] Pager 39232 Questions:](https://image.slidesharecdn.com/gracerollout-091101064257-phpapp01/75/Grace-Rollout-36-2048.jpg)