Onc july atlanta 2011
•Download as PPTX, PDF•
0 likes•501 views
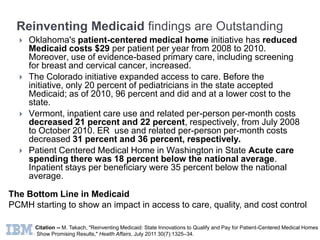
Patient-centered medical home initiatives in several states have shown promising results in improving access to care, quality, and cost control for Medicaid patients. Oklahoma saw a $29 per patient annual reduction in Medicaid costs from 2008-2010 alongside increased use of preventive care. Colorado expanded Medicaid access from 20% to 96% of pediatricians at lower costs. Vermont saw 21-22% decreases in inpatient care use and costs from 2008-2010 alongside 31-36% drops in ER use and related costs. Washington state's acute care spending was 18% below average with 35% fewer inpatient stays per beneficiary. Overall, these initiatives demonstrate that the patient-centered medical home model can positively impact Medicaid programs.
Report
Share
Report
Share
Recommended
Recommended
Steve Skardon Safety Net Summit Presentation, September 23, 2009The Palmetto Project: Putting Innovative Ideas to Work in South Carolina-Stev...

The Palmetto Project: Putting Innovative Ideas to Work in South Carolina-Stev...Health & Medicine Policy Research Group
More Related Content
What's hot
Steve Skardon Safety Net Summit Presentation, September 23, 2009The Palmetto Project: Putting Innovative Ideas to Work in South Carolina-Stev...

The Palmetto Project: Putting Innovative Ideas to Work in South Carolina-Stev...Health & Medicine Policy Research Group
What's hot (20)
The Patient-Centered Medical Home Impact on Cost and Quality: An Annual Revie...

The Patient-Centered Medical Home Impact on Cost and Quality: An Annual Revie...
The Palmetto Project: Putting Innovative Ideas to Work in South Carolina-Stev...

The Palmetto Project: Putting Innovative Ideas to Work in South Carolina-Stev...
Automated Post-Discharge Care: An Essential Tool to Reduce Readmissions

Automated Post-Discharge Care: An Essential Tool to Reduce Readmissions
HIMSS - Real Payer and Provider Collaborations - Final

HIMSS - Real Payer and Provider Collaborations - Final
From Patients to ePatients Driving a new paradigm for online clinical collabo...

From Patients to ePatients Driving a new paradigm for online clinical collabo...
Health Rosetta Case Study - City of Kirkland, Washington

Health Rosetta Case Study - City of Kirkland, Washington
Payment Reform for Primary Care – Minnesota DHS efforts

Payment Reform for Primary Care – Minnesota DHS efforts
The changing landscape of health care in the US -- drivers and outcomes

The changing landscape of health care in the US -- drivers and outcomes
Similar to Onc july atlanta 2011
Cleveland Heartlab 5th Annual Symposium:
Paul Grundy, Better Care, Reducing Costs, Improving Service Patient Centered Medical HomePaul Grundy, Better Care, Reducing Costs, Improving Service Patient Centered ...

Paul Grundy, Better Care, Reducing Costs, Improving Service Patient Centered ...Cleveland HeartLab, Inc.
Similar to Onc july atlanta 2011 (20)
2C Grundy Extracting Value: Patient Centered Medical Home EHiN 2014 

2C Grundy Extracting Value: Patient Centered Medical Home EHiN 2014
National Conference on Health and Domestic Violence. Plenary talk 

National Conference on Health and Domestic Violence. Plenary talk
DQ 3-2Integrated health care delivery systems (IDS) was develope.docx

DQ 3-2Integrated health care delivery systems (IDS) was develope.docx
How to Engage Physicians in Best Practices to Respond to Healthcare Transform...

How to Engage Physicians in Best Practices to Respond to Healthcare Transform...
Where Is Healthcare Going? And How Will We Get There? 

Where Is Healthcare Going? And How Will We Get There?
John lovelace 2011 03 25 public private p artnerships in health dublin mar...

John lovelace 2011 03 25 public private p artnerships in health dublin mar...
Paul Grundy, Better Care, Reducing Costs, Improving Service Patient Centered ...

Paul Grundy, Better Care, Reducing Costs, Improving Service Patient Centered ...
Population health management real time state-of-health analysis

Population health management real time state-of-health analysis
Tipping point: Hospital resilience in a perfect storm

Tipping point: Hospital resilience in a perfect storm
Providing More with Less: Primary Care Bright Spots

Providing More with Less: Primary Care Bright Spots
More from Paul Grundy
More from Paul Grundy (20)
The Patient-Centered Medical Home in the Transformation From Healthcare to He...

The Patient-Centered Medical Home in the Transformation From Healthcare to He...
A systematic review of the challenges to implementation of the patient-centre...

A systematic review of the challenges to implementation of the patient-centre...
Care by design magill retrospective mixed methods analysis sep 21 2011

Care by design magill retrospective mixed methods analysis sep 21 2011
Recently uploaded
Recently uploaded (20)
Goa Call Girl Service 📞9xx000xx09📞Just Call Divya📲 Call Girl In Goa No💰Advanc...

Goa Call Girl Service 📞9xx000xx09📞Just Call Divya📲 Call Girl In Goa No💰Advanc...
Kolkata Call Girls Shobhabazar 💯Call Us 🔝 8005736733 🔝 💃 Top Class Call Gir...

Kolkata Call Girls Shobhabazar 💯Call Us 🔝 8005736733 🔝 💃 Top Class Call Gir...
❤️Call Girl Service In Chandigarh☎️9814379184☎️ Call Girl in Chandigarh☎️ Cha...

❤️Call Girl Service In Chandigarh☎️9814379184☎️ Call Girl in Chandigarh☎️ Cha...
Chandigarh Call Girls Service ❤️🍑 9809698092 👄🫦Independent Escort Service Cha...

Chandigarh Call Girls Service ❤️🍑 9809698092 👄🫦Independent Escort Service Cha...
Call Girl In Indore 📞9235973566📞 Just📲 Call Inaaya Indore Call Girls Service ...

Call Girl In Indore 📞9235973566📞 Just📲 Call Inaaya Indore Call Girls Service ...
❤️Chandigarh Escorts Service☎️9814379184☎️ Call Girl service in Chandigarh☎️ ...

❤️Chandigarh Escorts Service☎️9814379184☎️ Call Girl service in Chandigarh☎️ ...
💚Reliable Call Girls Chandigarh 💯Niamh 📲🔝8868886958🔝Call Girl In Chandigarh N...

💚Reliable Call Girls Chandigarh 💯Niamh 📲🔝8868886958🔝Call Girl In Chandigarh N...
Cardiac Output, Venous Return, and Their Regulation

Cardiac Output, Venous Return, and Their Regulation
Premium Call Girls Dehradun {8854095900} ❤️VVIP ANJU Call Girls in Dehradun U...

Premium Call Girls Dehradun {8854095900} ❤️VVIP ANJU Call Girls in Dehradun U...
Call Girls in Lucknow Just Call 👉👉 8875999948 Top Class Call Girl Service Ava...

Call Girls in Lucknow Just Call 👉👉 8875999948 Top Class Call Girl Service Ava...
Chandigarh Call Girls Service ❤️🍑 9809698092 👄🫦Independent Escort Service Cha...

Chandigarh Call Girls Service ❤️🍑 9809698092 👄🫦Independent Escort Service Cha...
ANATOMY AND PHYSIOLOGY OF REPRODUCTIVE SYSTEM.pptx

ANATOMY AND PHYSIOLOGY OF REPRODUCTIVE SYSTEM.pptx
Independent Bangalore Call Girls (Adult Only) 💯Call Us 🔝 7304373326 🔝 💃 Escor...

Independent Bangalore Call Girls (Adult Only) 💯Call Us 🔝 7304373326 🔝 💃 Escor...
Call girls Service Phullen / 9332606886 Genuine Call girls with real Photos a...

Call girls Service Phullen / 9332606886 Genuine Call girls with real Photos a...
Kolkata Call Girls Service ❤️🍑 9xx000xx09 👄🫦 Independent Escort Service Kolka...

Kolkata Call Girls Service ❤️🍑 9xx000xx09 👄🫦 Independent Escort Service Kolka...
💰Call Girl In Bangalore☎️63788-78445💰 Call Girl service in Bangalore☎️Bangalo...

💰Call Girl In Bangalore☎️63788-78445💰 Call Girl service in Bangalore☎️Bangalo...
Call 8250092165 Patna Call Girls ₹4.5k Cash Payment With Room Delivery

Call 8250092165 Patna Call Girls ₹4.5k Cash Payment With Room Delivery
💚Chandigarh Call Girls Service 💯Piya 📲🔝8868886958🔝Call Girls In Chandigarh No...

💚Chandigarh Call Girls Service 💯Piya 📲🔝8868886958🔝Call Girls In Chandigarh No...
Call Girl in Chennai | Whatsapp No 📞 7427069034 📞 VIP Escorts Service Availab...

Call Girl in Chennai | Whatsapp No 📞 7427069034 📞 VIP Escorts Service Availab...
Onc july atlanta 2011
- 1. ONC and PCMH 2011 Paul Grundy, MD, MPH, FACOEM, FACPM IBM Director Healthcare TransformationPresident Patient Centered Primary Care Collaborative Paul Grundy MD, MPH IBM International Director Healthcare Transformation Trip to Denmark July 10 2009
- 2. Reinventing Medicaid findings are Outstanding Oklahoma's patient-centered medical home initiative has reduced Medicaid costs $29 per patient per year from 2008 to 2010. Moreover, use of evidence-based primary care, including screening for breast and cervical cancer, increased. The Colorado initiative expanded access to care. Before the initiative, only 20 percent of pediatricians in the state accepted Medicaid; as of 2010, 96 percent and did and at a lower cost to the state. Vermont, inpatient care use and related per-person per-month costs decreased 21 percent and 22 percent, respectively, from July 2008 to October 2010. ER use and related per-person per-month costs decreased 31 percent and 36 percent, respectively. Patient Centered Medical Home in Washington in State Acute care spending there was 18 percent below the national average. Inpatient stays per beneficiary were 35 percent below the national average. The Bottom Line in Medicaid PCMH starting to show an impact in access to care, quality, and cost control. Citation -- M. Takach, "Reinventing Medicaid: State Innovations to Qualify and Pay for Patient-Centered Medical Homes Show Promising Results," Health Affairs, July 2011 30(7):1325–34.
- 3. Out in July 2011 BCBS MA 6% decrees cost (NEJM) BCBS Mi 2670 physician (BIG study)
- 4. MGMA: 70% of Practices at Least Interested in Becoming Patient Centered Medical Homes 13 to 20 % are already on the road Some states Michigan, Minnesota, Maryland, RI, VT 50% already are well on the road !! Standard of care in the VA, DOD IBM $ 60 per Member BCBS HI 14.6% ^
- 5. Outside Hospital video clip
- 6. Who was the Shooter’s Doctor? Population management Accountability
- 7. Why Innovate Affordability $30,000 +166% $25,000 $20,000 $15,000 +118% $10,000 $4,918 $5,000 $0 2001 2009 2019 - Employee Payroll Contributions - Employer Cost - Employee Out of Pocket Expenses a The Elephant in the room $28,530 Costs continue their upward climb… …with employers still picking up much of the tab… $10,743
- 8. Health care is a business issue, not a benefits issue
- 9. The Cause? Mostly due to unregulated fee-for-service payments and an over reliance on rescue/specialty care. This is stark evidence that the U.S. health care Industry has been failing us for years “Commonly cited causes for the nation's poor performance are not to blame - it is the failure of the deliver system!!” You the AHC’s - Unaccountable Care Organizations PART of this problem * Peter A. Muennig and Sherry A. Glied Health Affairs Oct. 7, 2010
- 10. Don’t handle your care needs in a BAD MEDICAL NEIGHBORHOOD!! Unaccountable care, lack of organization, DO NOT GO THERE ALONE !! Be wise when you pay for care, KNOW WHAT YOU BUY!!
- 11. Coordination -- we do NOT know how to play as a team “ We don't have a health care delivery system in this country. We have an expensive plethora of uncoordinated, unlinked, micro systems, each performing in ways that too often create sub-optimal performance, both for the overall health care infrastructure and for individual patients." George Halvorson, from “Healthcare Reform Now
- 12. “We do kidney transplants and dialysis more often than anyone, but we need to, because patients are not given the kind of coordinated primary care that would prevent chronic complications of renal and heart disease from becoming acute.” George Halvorson (CEO Kaiser) from “Healthcare Reform Now”
- 13. The Diabetic needs A long-term comprehensive relationship with a Personal Physician empowered with the right tools and linked to their care team.
- 15. Physician directed medical practice – the personal physician leads a team of individuals at the practice level who collectively take responsibility for the ongoing care of patients
- 16. Whole person orientation – the personal physician is responsible for providing for all the patient’s health care needs or arranging care with other qualified professionals
- 17. Care is coordinated and integrated across all elements of the complex healthcare community- coordination is enabled by registries, information technology, and health information exchanges
- 19. The Quadruple AimReadiness, Experience of Care, Population Health, Cost Per Capita Cost Population Health The System Integrator Creates a partnership across the medical neighborhood Drives PCMH primary care redesign Offers a utility for population health and financial management System Integrator Patient Experience Productivity
- 21. You need a place of command and control
- 22. You need a horizontal platform from which to launch vertical weapon systems
- 24. Team-Based HealthcareDelivery Population Health Access to Care Patient is the centerof theMedical Home Advanced IT Systems Patient-Centered Care Decision Support Tools Refocused Medical Training Patient & Physician Feedback Enhancing Health and the Patient Experience Medical Home Model Model adapted from theNNMC Medical Home
- 25. Defining the Care Centered on Patient Superb Access to Care Team Care Patient Engagement in Care Patient Feedback Clinical Information Systems Publically Available Information Care Coordination
- 26. Smarter Healthcare… 36.3% Drop in hospital days 32.2% Drop in ER use 9.6% Total cost 10.5% Inpatient specialty care costs are down 18.9% Ancillary costs down 15.0% Outpatient specialty down Outcomes of Implementing Patient Centered Medical Home Interventions: A Review of the Evidence from Prospective Evaluation Studies in the US, K. Grumbach & P. Grundy, November 16th 2010
- 27. Patient Centered Medical Home in Washington in State provided great example of how states can lower spending by reducing hospital care and expanding access to primary care providers. Acute care spending there was 18 percent below the national average. Inpatient stays per beneficiary were 35 percent below the national average. Ref Health Affairs 7 July 2011 .http://healthaffairs.org/blog/2011/07/07/medicaid-spending-variations-driven-more-by-volume-than-price-says-study-in-new-health-affairs/http://content.healthaffairs.org/content/30/7/1316.full
- 30. Provide care management and coordination by specially-trained team members.
- 31. Use an EHR with decision support.
- 32. Use CPOE for all orders, test tracking, and follow-up.
- 33. Medication reconciliation for every visit.
- 34. Prescription drug decision support.
- 36. Pre-visit planning and after-visit follow-up for care management.
- 37. Offer patient self-management support.
- 38. Provide a visit summary to the patient following each visit.
- 39. Maintain a summary-of-care record for patient transitions.
- 42. The development of care plans.
- 43. Performance outcome measures.
- 44. PCMH in Action Vermont “Blueprint” model A Coordinated Health System Hospitals Community Care Team Nurse Coordinator Social Workers Dieticians Community Health Workers Care Coordinators Public Health Prevention HEALTH WELLNESS PCMH Health IT Framework Specialists Global Information Framework PCMH Evaluation Framework Public Health Prevention Operations
- 45. Vermont Financial Impact Vermont Financial Impact
- 46. Payment reform requires more than one method, you have dials, adjust them!!! fee for health” “fee for outcome” “fee for process” “fee for belonging “fee for service” “fee for satisfaction”
- 47. Reinventing Medicaid: State PCMH Innovations Show Promising Results New Payment Incentives – 17 states evaluated Monthly care management fees. Most of the states studied pay patient-centered medical homes a per-member per-month fee averaging about $3 to $6. PAY FOR HIT Meaningful USE Enhanced fee-for-service payments. Medicaid strategy rewards "well care" more highly than "sick care." Network payments. North Carolina and Vermont pay networks or teams to support patient-centered medical homes. Pay-for-performance. Nebraska, Oklahoma, and Pennsylvania are using performance-based payments. to complement other payments to patient-centered medical homes. Pennsylvania practices that have met certain performance criteria can share in any savings they generate. Medicaid plans and commercial insurers. Seventeen states are participating or plan to participate in multipayer patient-centered medical home initiatives. Eight will add Medicare as a payer in 2011 Citation -- M. Takach, "Reinventing Medicaid: State Innovations to Qualify and Pay for Patient-Centered Medical Homes Show Promising Results," Health Affairs, July 2011 30(7):1325–34.
- 49. PCMH is non-political – the right POV for delivery transformation “We never abandoned advocating new Models of care. We’ve long pushed folks to realize that Delivery reform is the key.” The patient-centered medical home is core. “We included the attached chapter on PCMH in our book. and have a new publication on ACOs coming out in January.”
- 50. OR? …Requires a Smarter Healthcare Workforce Where do you train the Workforce?
- 52. Analytics Maturity Landscape Communication & Culture Breakaway Analytics embraced & integrated into every day decisions & operations Passionate sponsor of analytics Test and Learn Culture Intelligent Operational buy-in to performance analysis driving decisions Robust feedback loop Advanced Analytics Monitoring, Prediction, Action Automated analysis/alert Performance messages widely communicated Performance Metrics Leverage cross- departmental & functional data to derive actionable insight Predictive modeling Single version of truth Integrated information Descriptive Analytics Adaptive Machine Learning Contextual business rules Collaboration & workflow tools to aid planning & info sharing Data warehouses, governance and production reporting Pride in the gut based decision Basic Leverage structured & unstructured data for decision making Real-Time Decision Support Personalized & role based portal Spreadsheets Isolated reporting & analysis systems Significant manual input
- 53. Patients love to see meaningful information about themselves and it take IT tools to If you give patients educational materials with their name on it and with their data analyzed in it, they will read it, pour over it and discuss it with you. If you tear off a generic sheet and give it to them, it often goes in the waste basket. If you give patients an analysis of their health risk AND if you include a “what if” scenario, i.e., what will their health risk be if they make a change; you can prove to them, “if you the healer make a change, it will make a difference to your patient.”
- 55. Really engage your patients find out what they need and become very patient centered
- 56. Integrate value base purchasing with PCMH in your plan designee (understand what the buyer wants)
- 57. Stop teaching the past you are in a world of Data, teams, actionable information
- 58. Integrate Health and Sick care
- 60. I) if quality care exists in your community, use it 2) Demand improved primary care (and be willing to pay for the transformation if in the long run it saves you Money and it does it) Communities need to be taught how to recruit and retain a primary care physician. There is a lot of work that has been done on this. 3) Seek out and use “Patient Centered Medical Homes” for health care 4) Find physicians who are trying to conquered the digital divide 5) Find a doctor comfortable with moving into the future with data, populating management, 6) Demand a focus on quality 7) Demand provides in your community to collaborate, collaborate, collaborate If there is a community health center (CHC), a rural health clinic, and a critical access (or small rural hospital) in your community, encourage collaboration 8) Encourage mental health and primary care to work together (the Brain is connected to the body) 9) Work to build a healthy community integrate health and sick care
