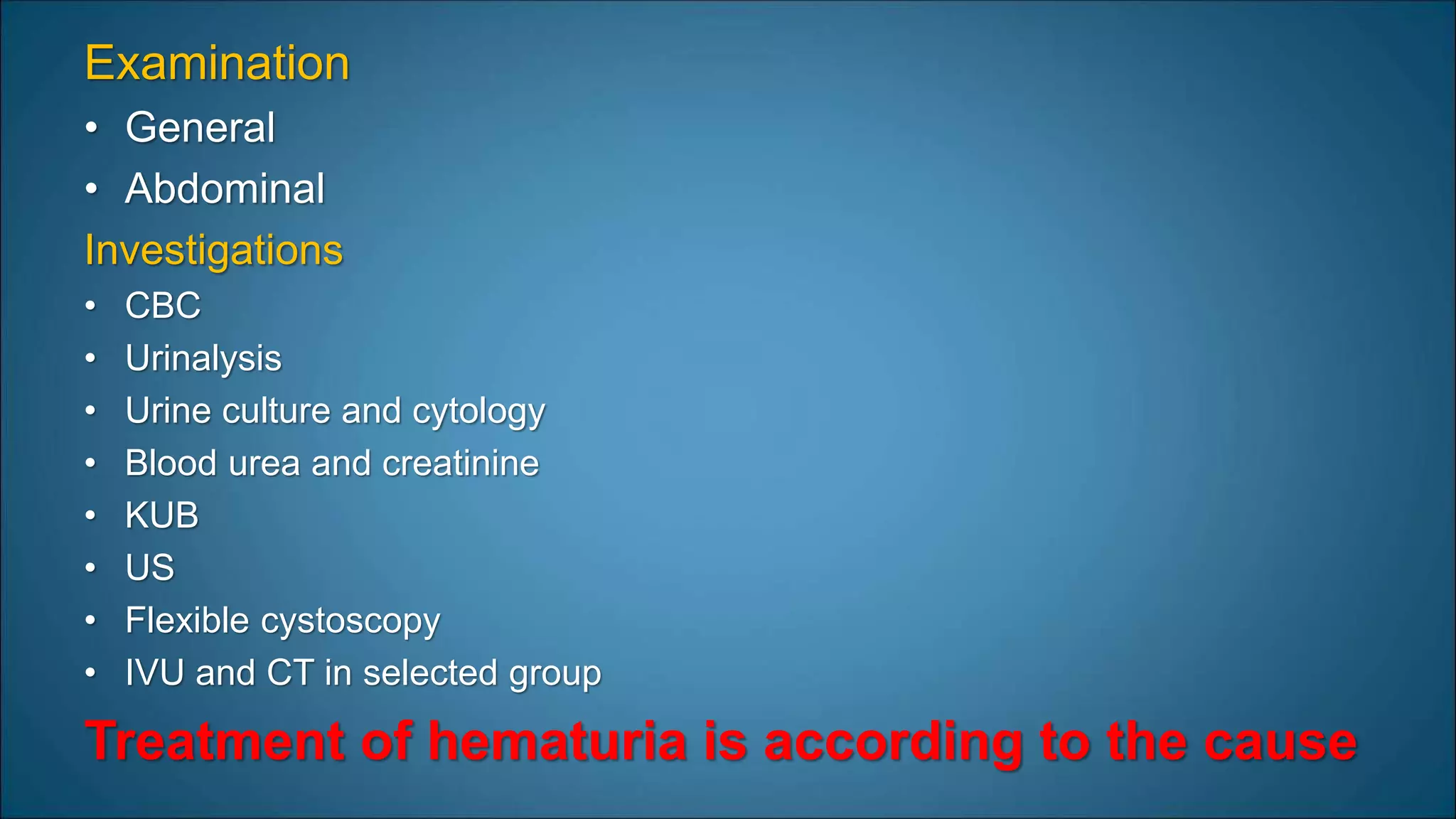
This document discusses various urological emergencies including hematuria, ureteric colic, acute scrotum, priapism, urinary retention, paraphimosis, anuria, pyonephrosis, and Fournier's gangrene. It provides details on the causes, presentations, diagnoses, and management of each condition. For acute scrotum, it describes testicular torsion, epididymo-orchitis, and their signs and symptoms. For priapism, it distinguishes ischemic and non-ischemic types and discusses their causes, evaluations, and treatments. Immediate medical or surgical intervention is often needed to resolve urological emergencies and prevent long-term complications