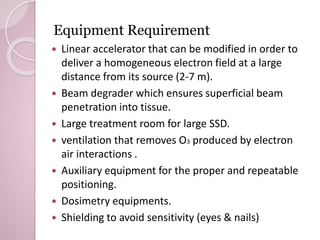
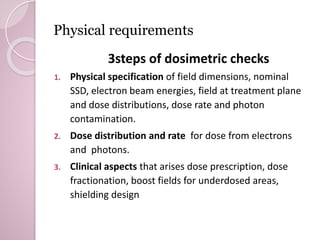
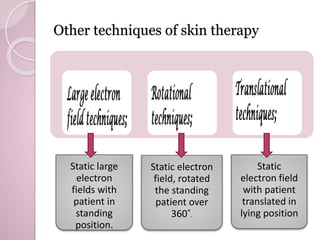
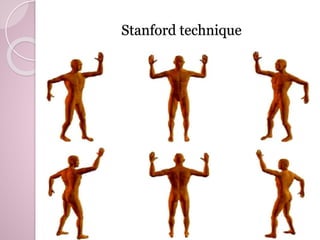
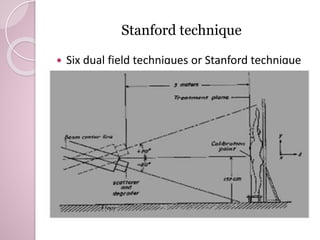
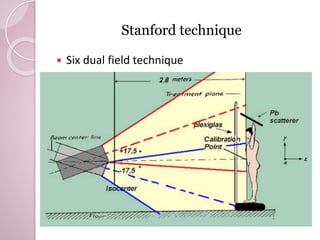
This document reviews techniques for total skin electron beam (TSEB) therapy. It discusses the equipment needed, including a linear accelerator capable of producing large, uniform electron fields at an extended source-to-skin distance. The Stanford technique is described as delivering radiation using six dual electron fields while the patient rotates, allowing treatment in a small room. High dose rates of 2500-3000 cGy/min are recommended to reduce treatment time. Dose prescription for TSEB therapy typically involves delivering 27-40 Gy over 9 weeks at 4 days per week.