Embed presentation
Downloaded 120 times

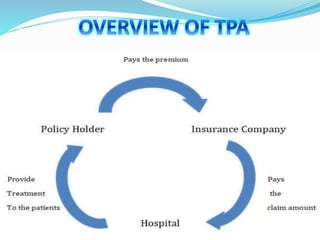


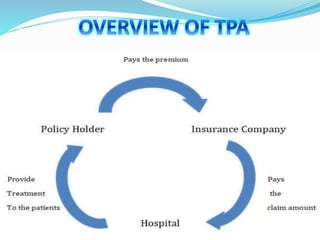
Third party administrators process insurance claims on behalf of insurance companies based on contracts. They play an important role in the health insurance sector by providing better services to policyholders. In India, TPAs are regulated by the Insurance Regulatory and Development Authority and must be licensed. The objective of the study is to better understand the current work of TPAs, suggest improvements, gain exposure to workflows, and streamline processes to benefit all stakeholders.