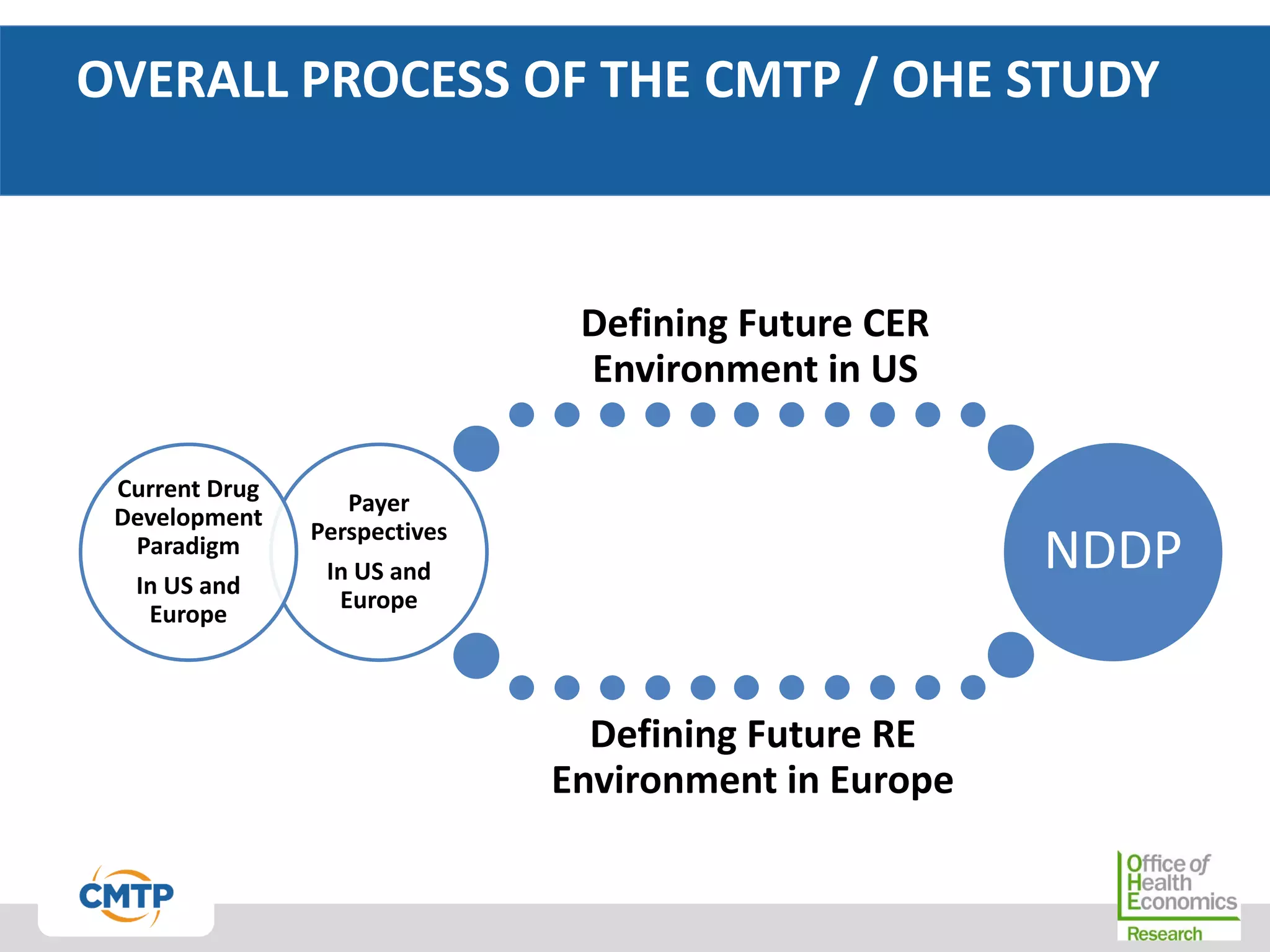
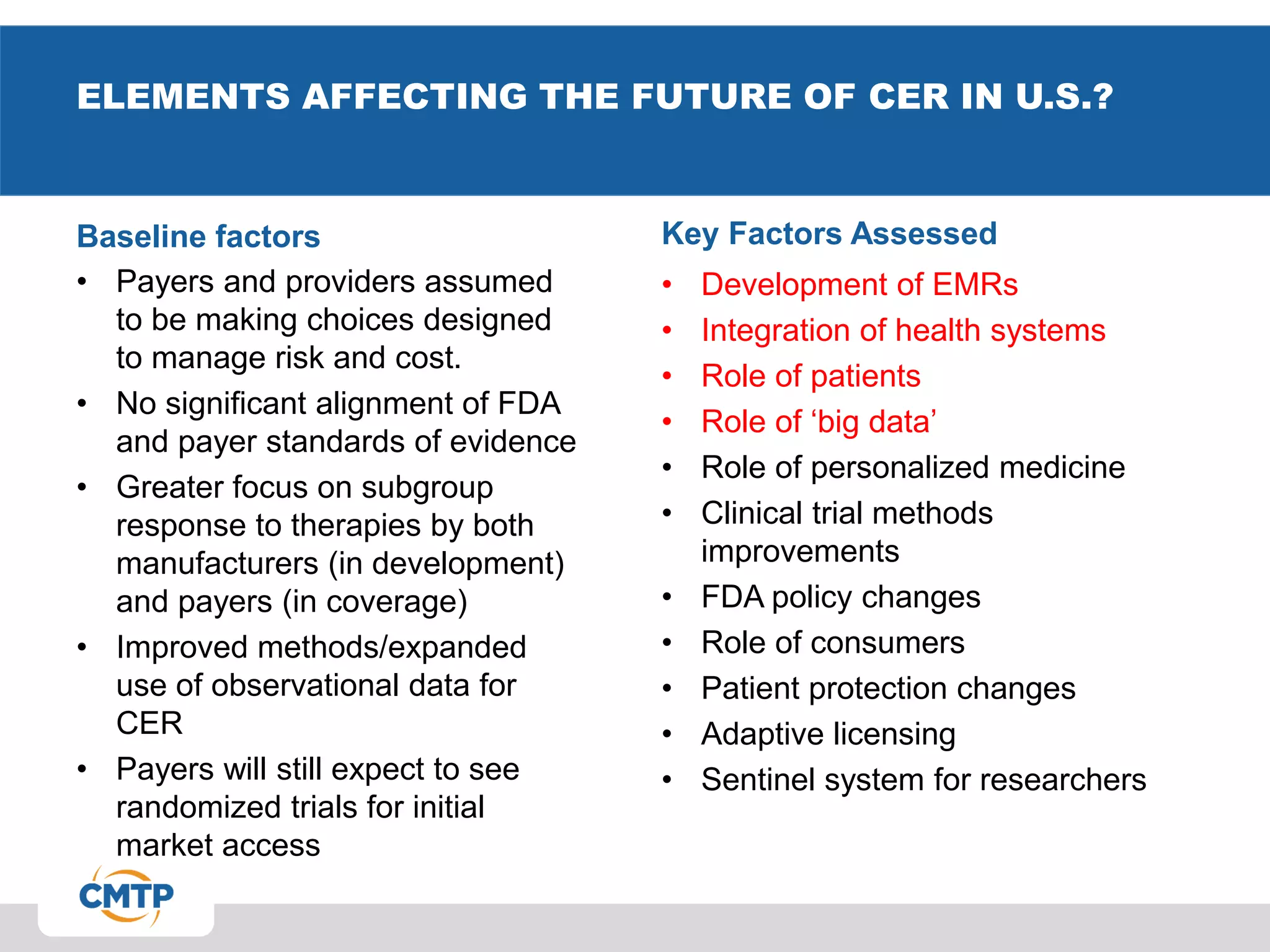
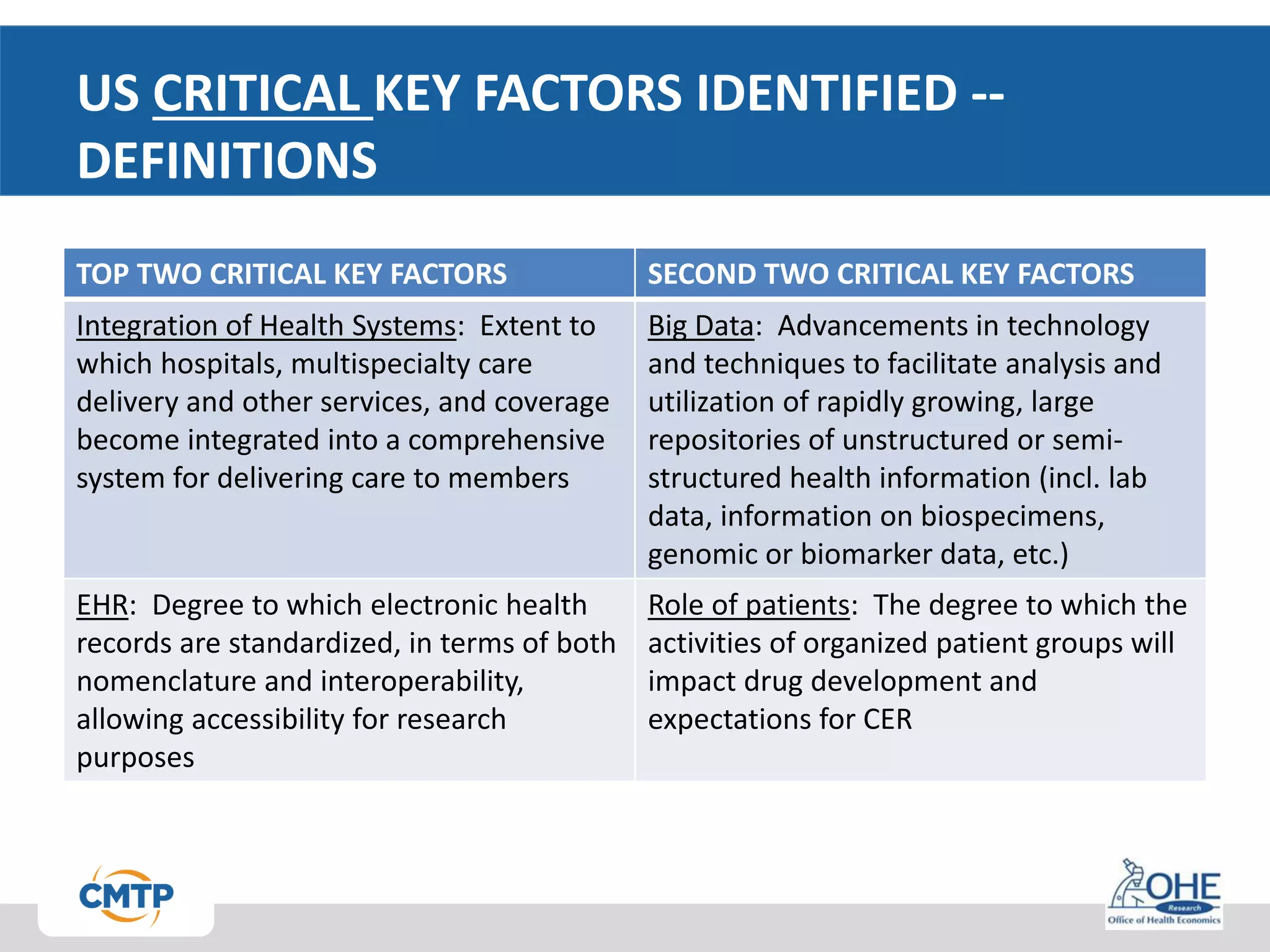
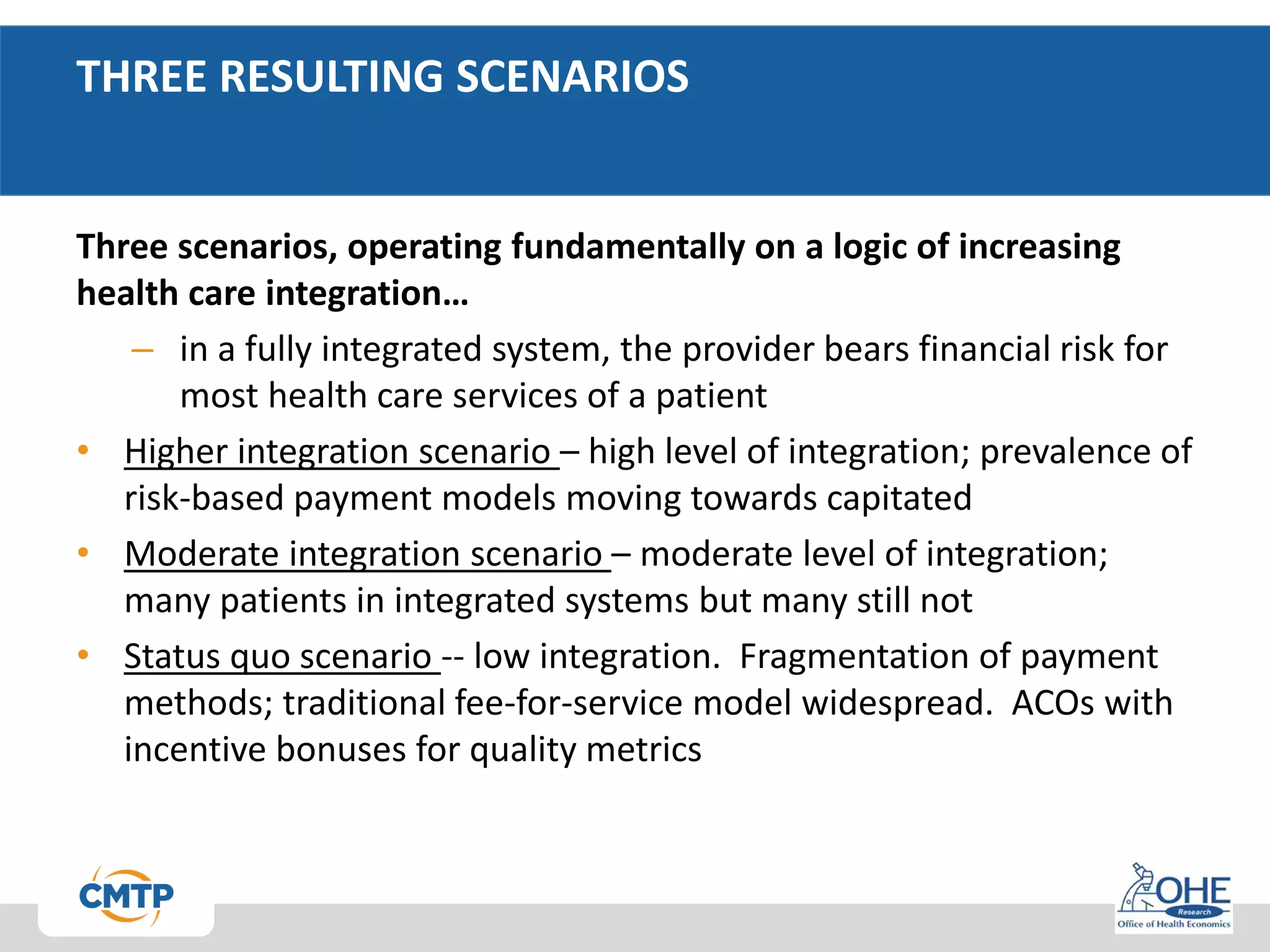
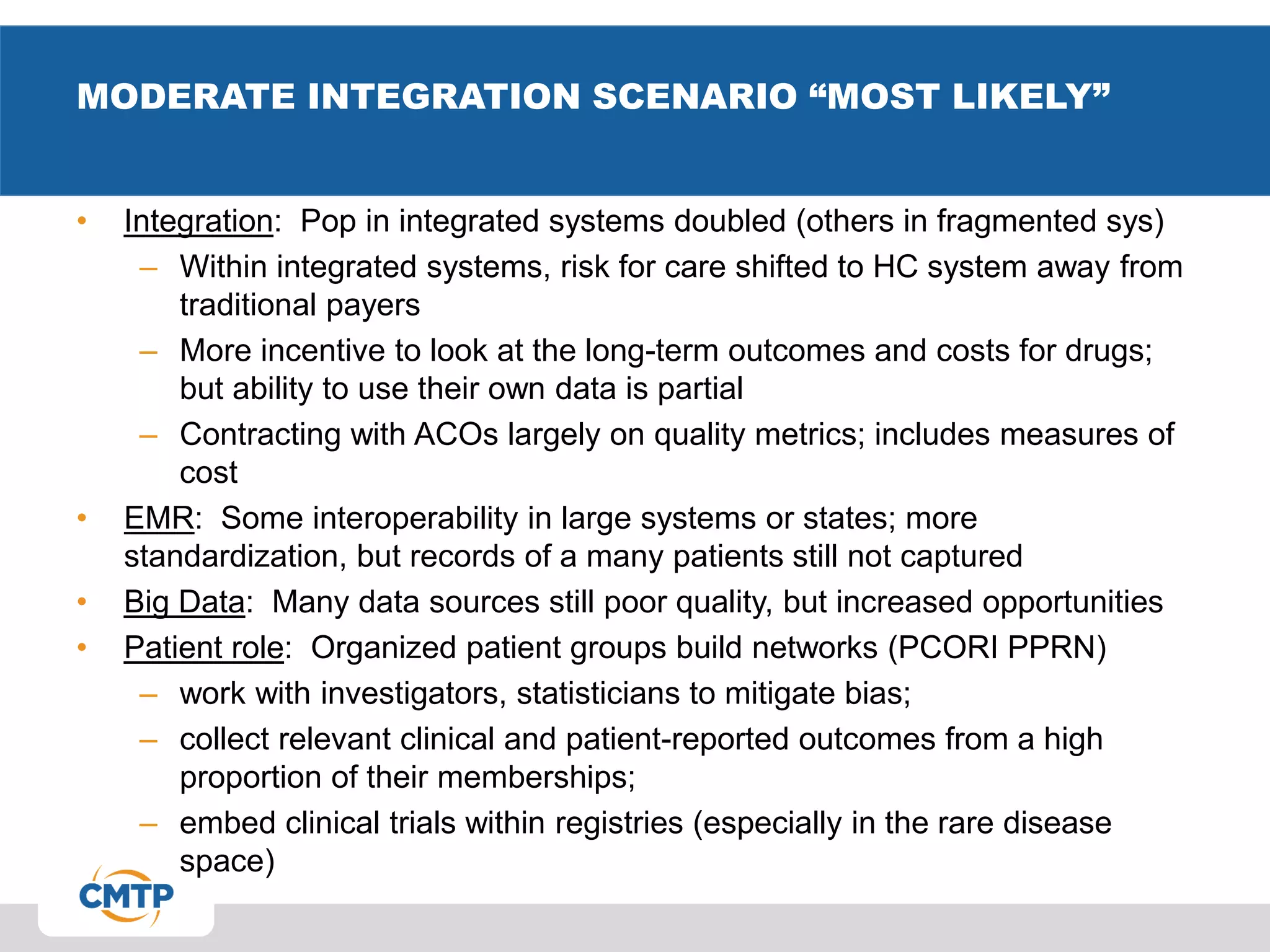
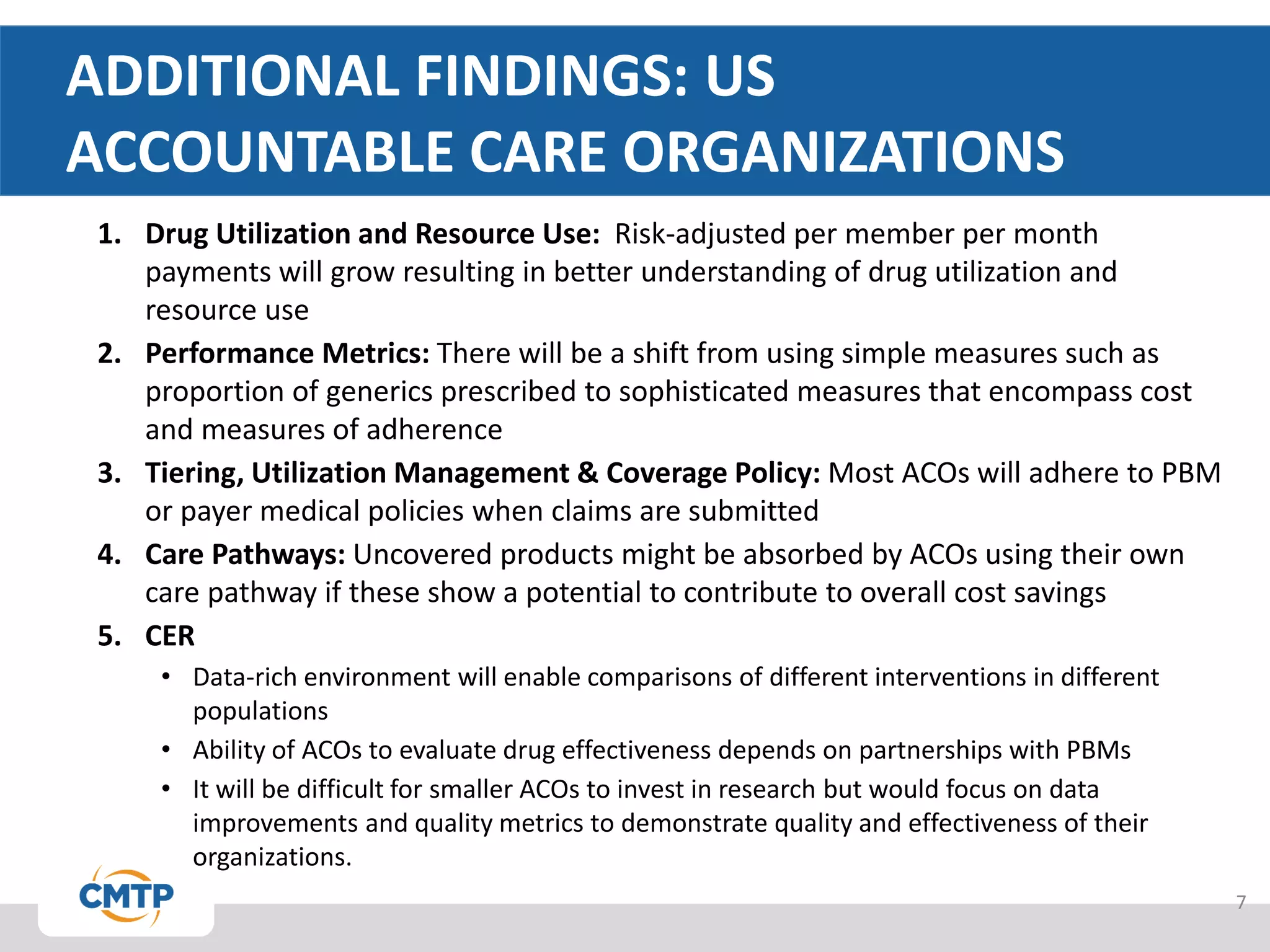
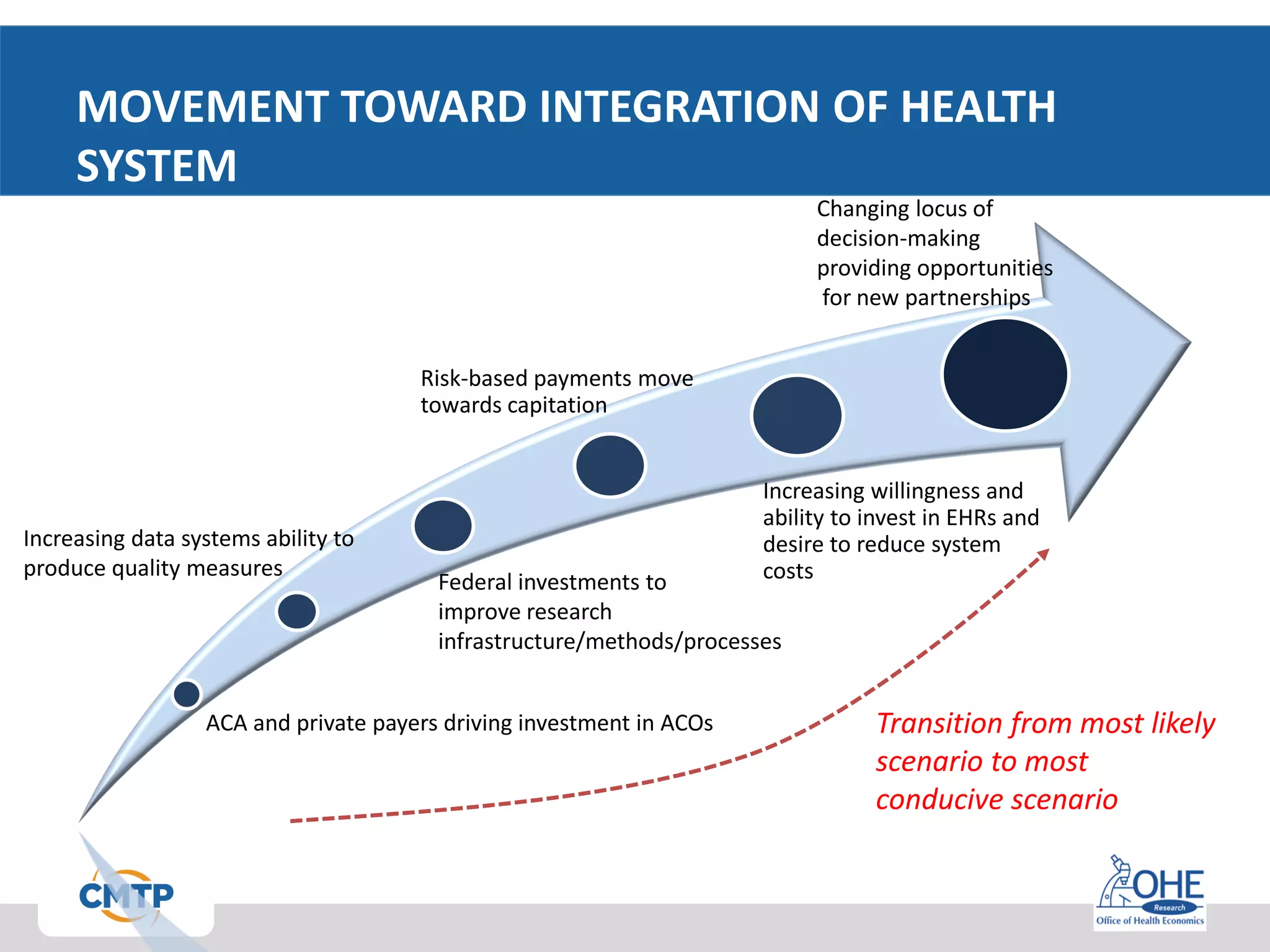
This document discusses scenario-building methods to define the future of clinical evidence requirements in the US drug development and healthcare systems. It identifies key factors like integration of health systems, use of big data, and patient roles that could impact clinical evidence requirements. Three potential scenarios are described ranging from a status quo system to a fully integrated system. The "moderate integration" scenario is deemed most likely, featuring some increased system integration, standardized electronic health records, growing big data opportunities, and more organized patient groups. Accountable care organizations are also examined, finding they may evaluate drug effectiveness and cost-effectiveness as risk-based payments increase and care pathways are established.