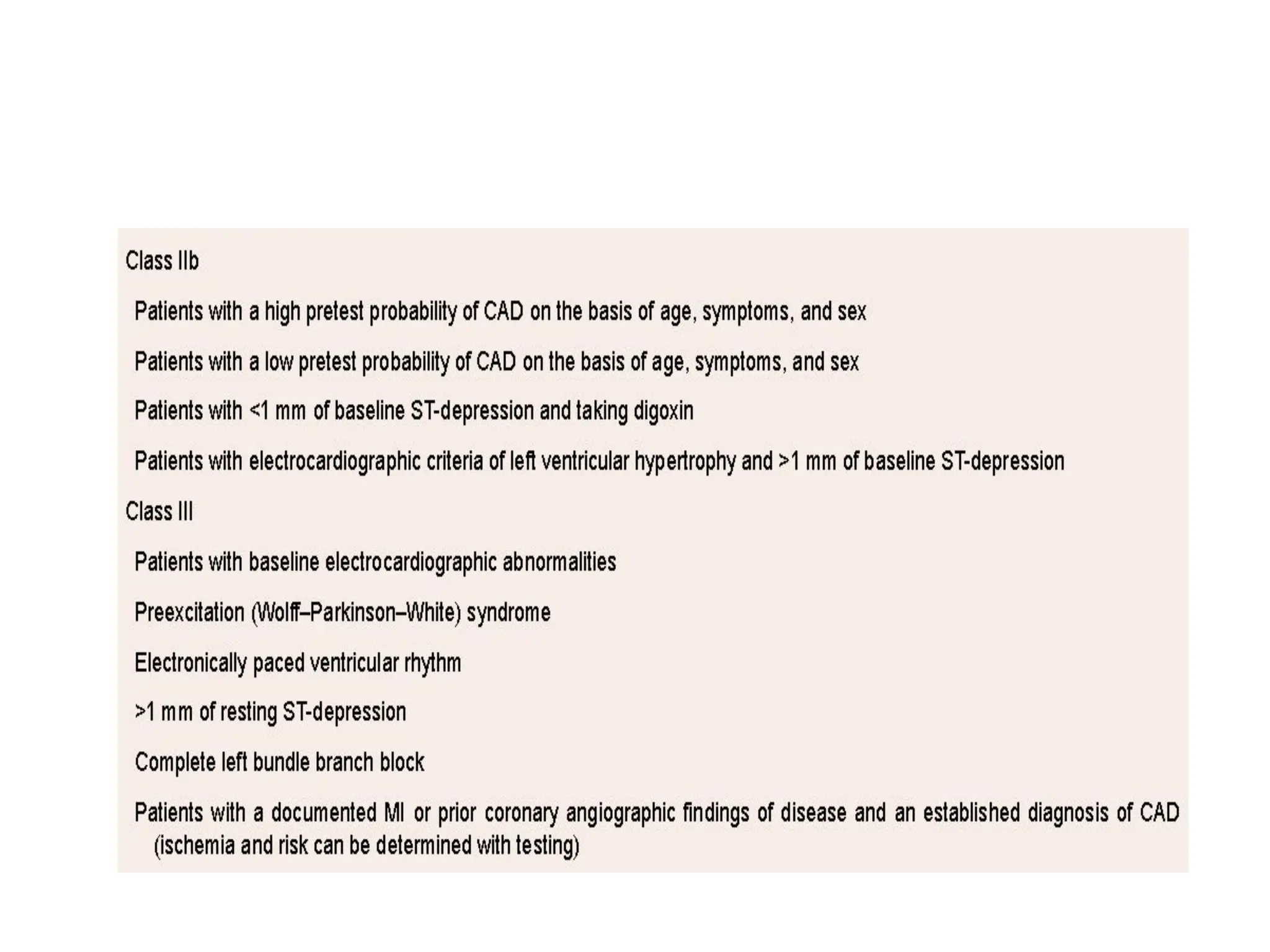
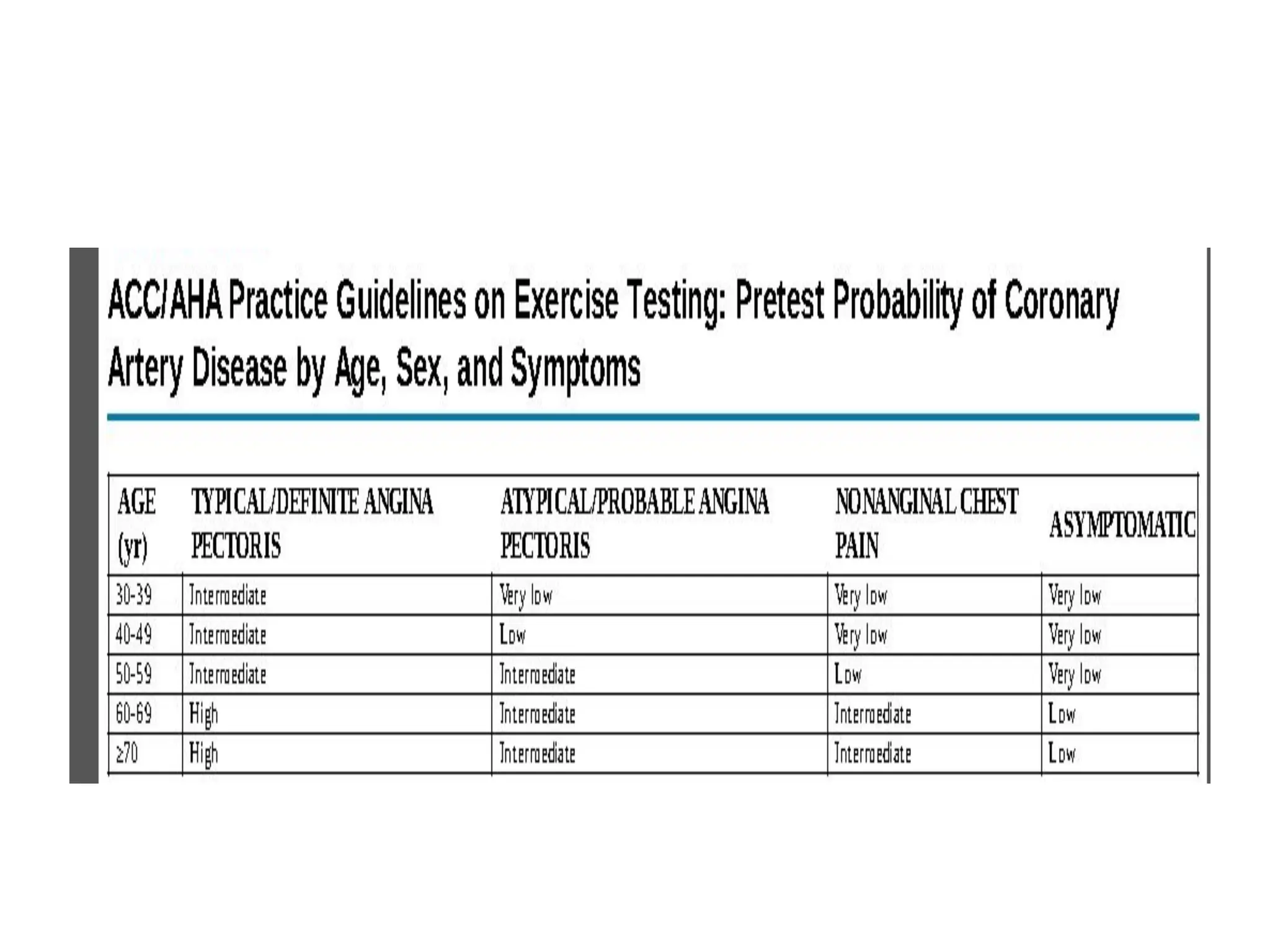
The document details the purposes and guidelines for exercise testing, particularly focusing on its role in diagnosing coronary artery disease (CAD), evaluating physical capacity, and predicting cardiovascular events. It includes contraindications, patient preparation, assessment protocols, monitoring during tests, and interpretations of electrocardiographic data. Additionally, it addresses complications, functional capacity markers, and prognostic tools such as the Duke treadmill score and heart rate recovery metrics.






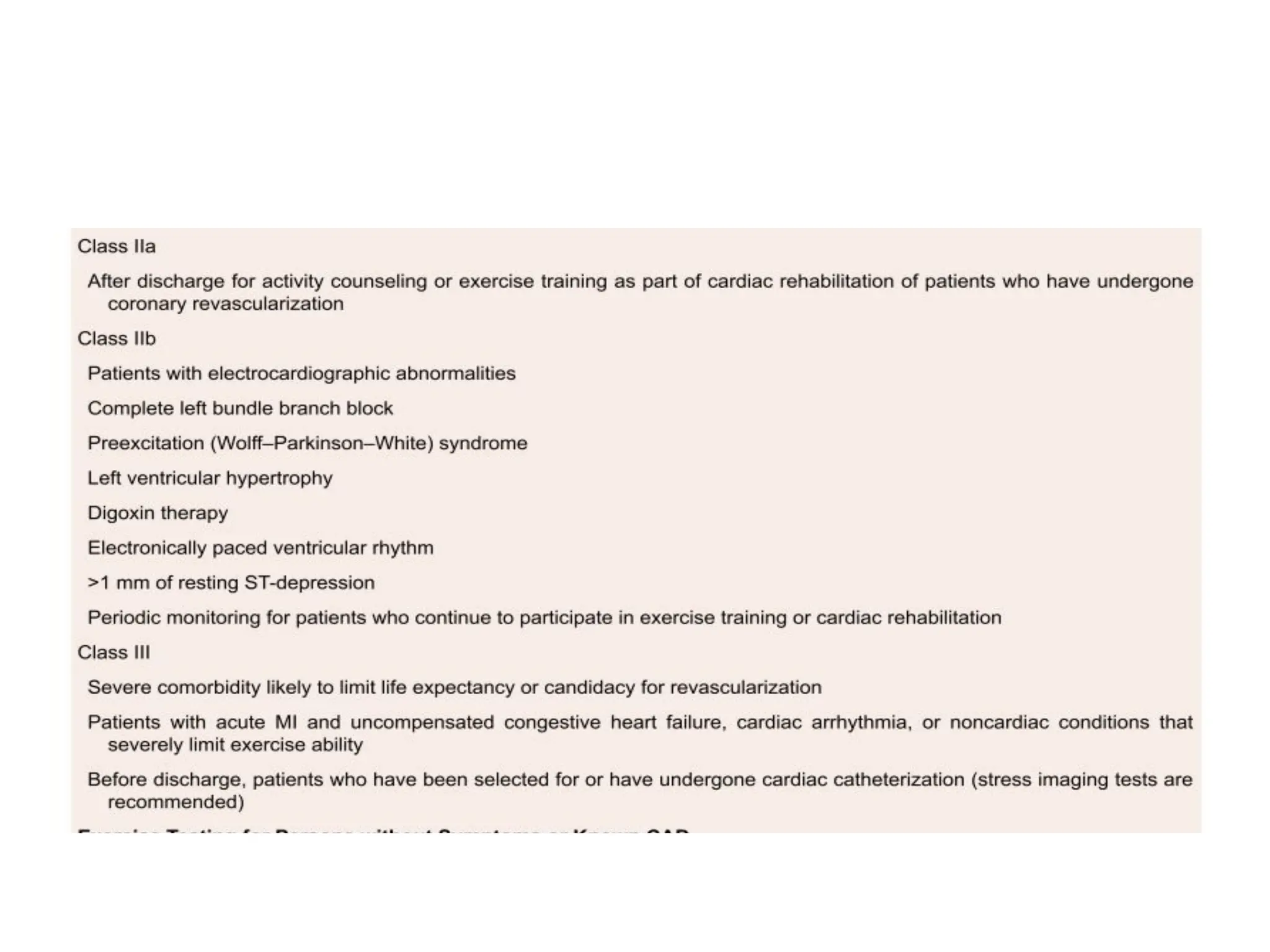






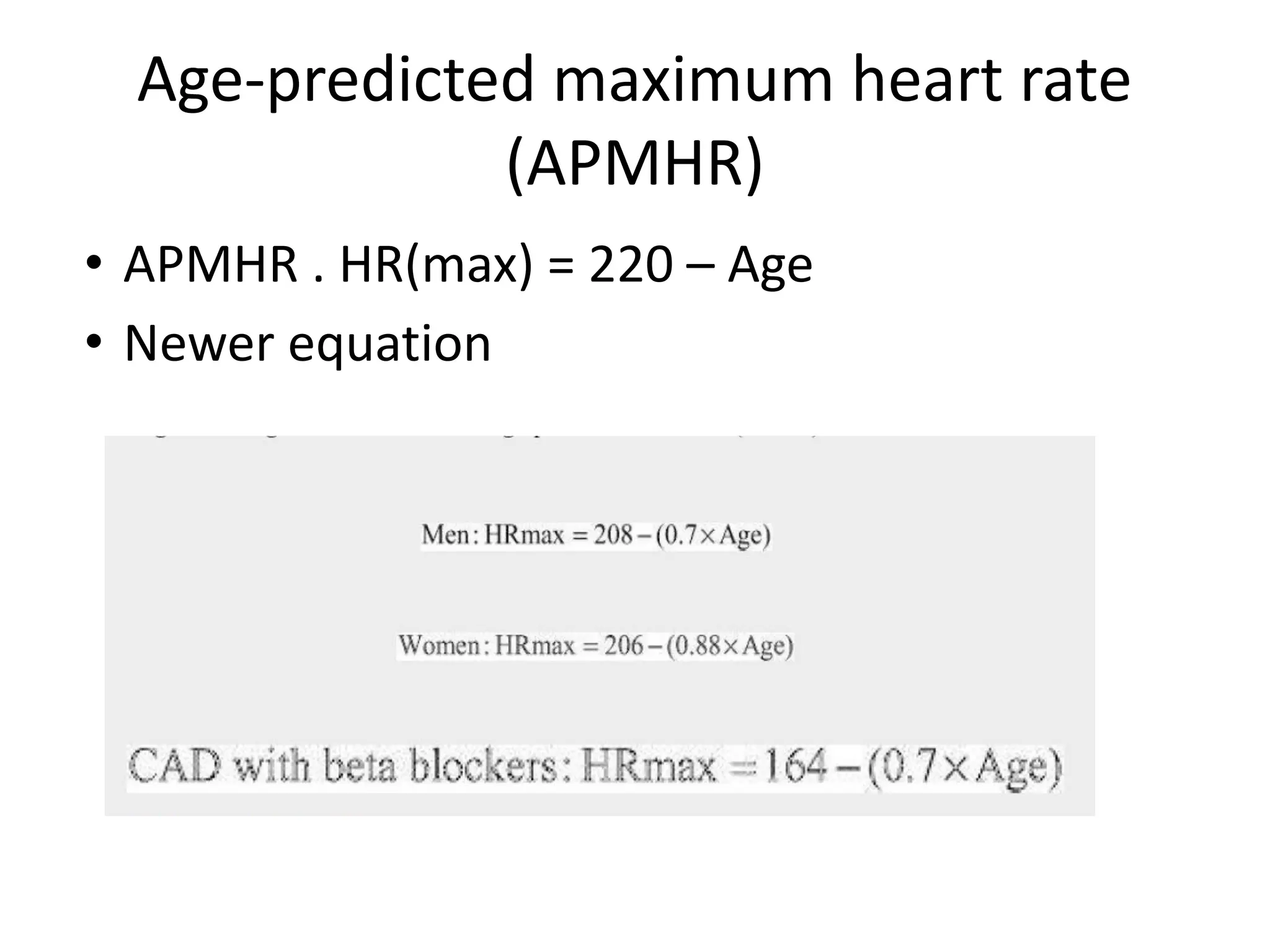
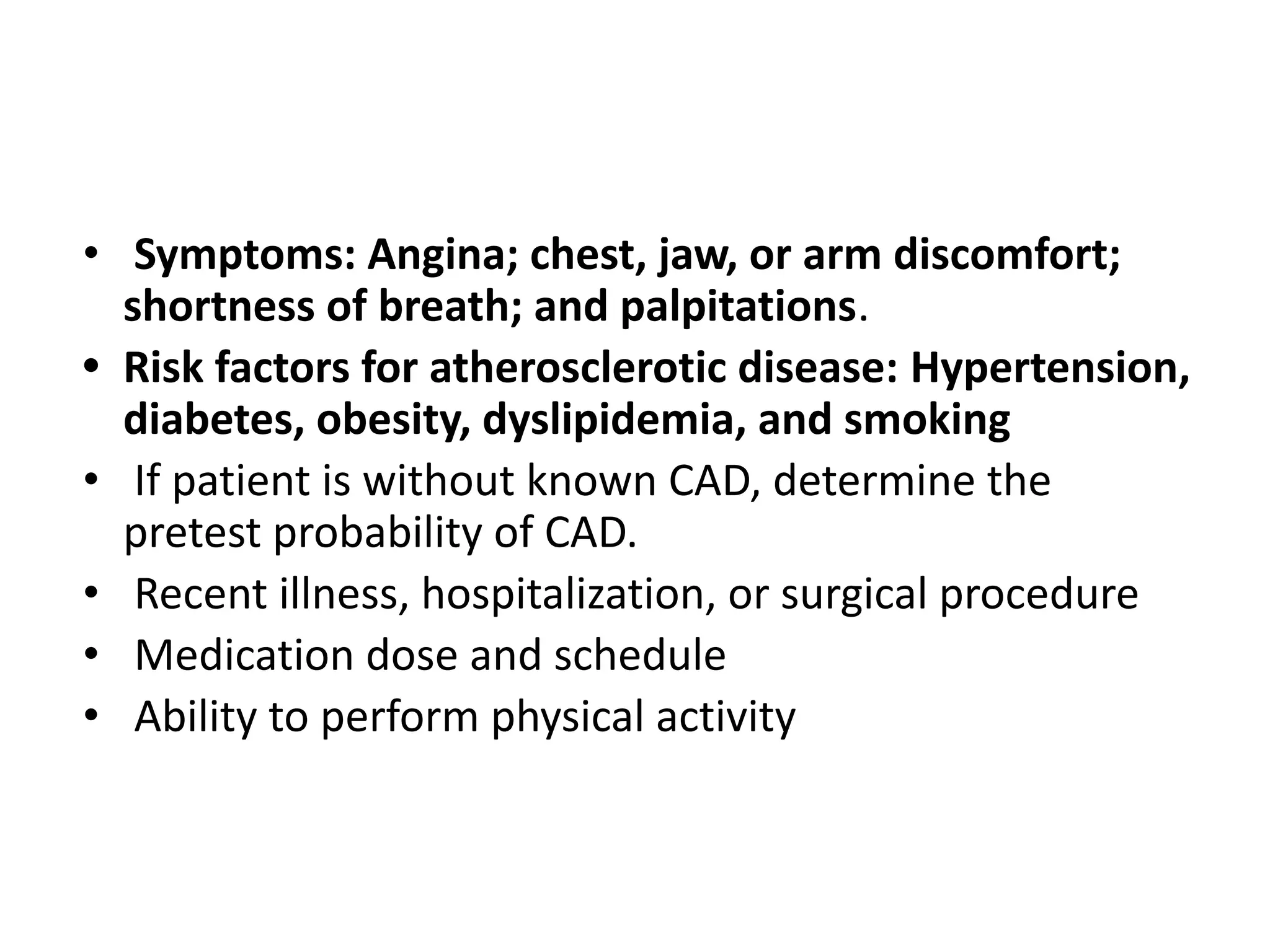
![HISTORY
• Medical history: including cardiovascular disease (known
existing coronary artery disease [CAD], previous myocardial
infarction, or coronary revascularization);
• Arrhythmias
• Syncope or presyncope;
• Pulmonary disease, including asthma, emphysema, and
bronchitis or recent pulmonary embolism;
• Cerebrovascular disease, including stroke;
• Peripheral artery disease;
• Current pregnancy;
• Musculoskeletal, neuromuscular, or joint disease.](https://image.slidesharecdn.com/tmtppt-241209050040-aff0e854/75/TMT-for-evaluation-in-chronic-stable-angina-20-2048.jpg)


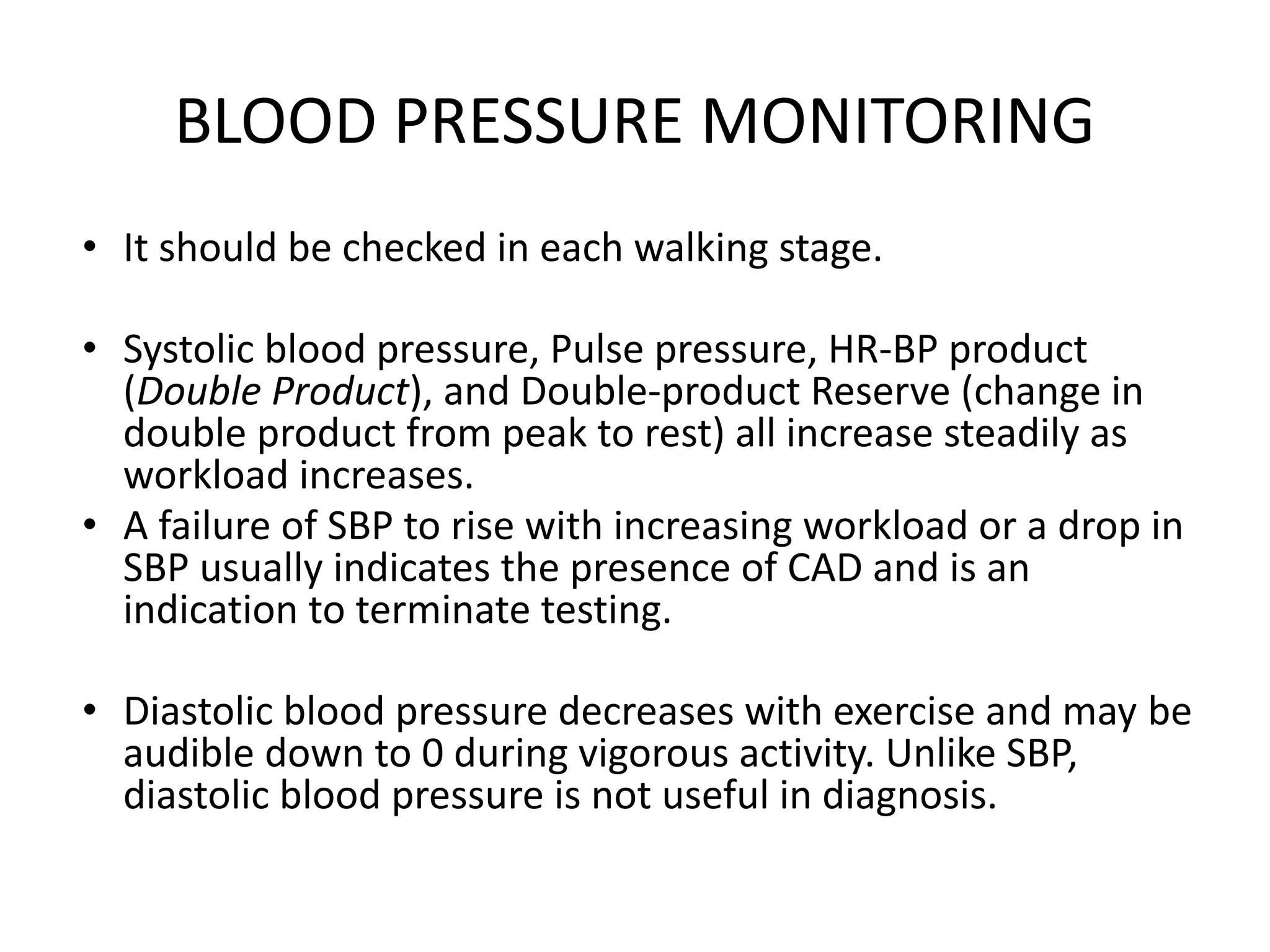
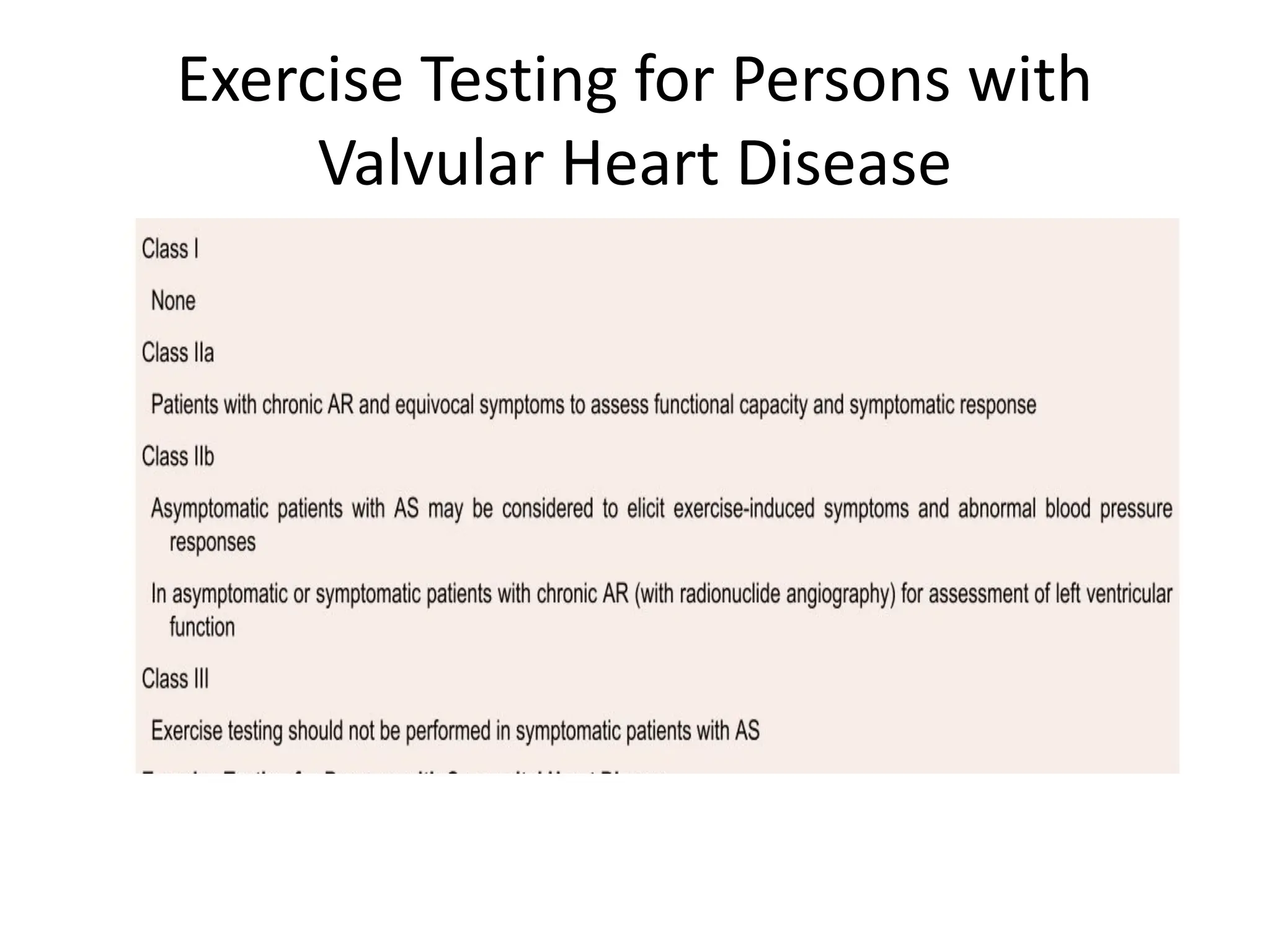
![Relative Indications
• Marked ST displacement (horizontal or
downsloping of >2 mm, measured 60 to 80 ms
after the J point [the end of the QRS complex])
in a patient with suspected ischemia
• Drop in systolic blood pressure >10 mmHg
(persistently below baseline) despite an
increase in workload, in the absence of other
evidence of ischemia
• Increasing chest pain](https://image.slidesharecdn.com/tmtppt-241209050040-aff0e854/75/TMT-for-evaluation-in-chronic-stable-angina-30-2048.jpg)