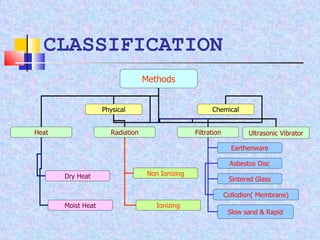
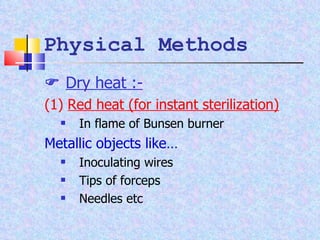
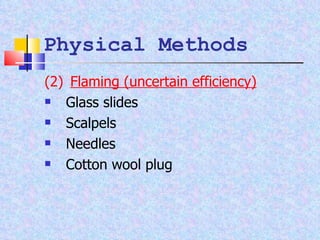
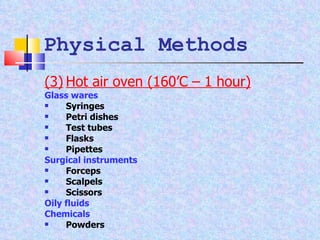
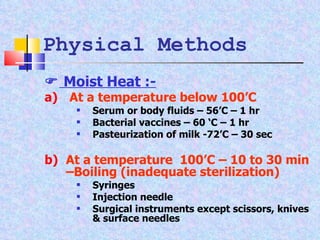
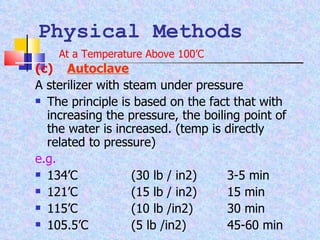
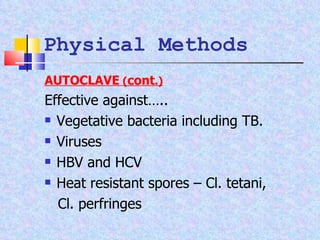
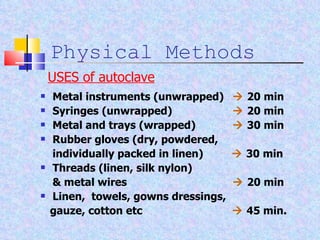
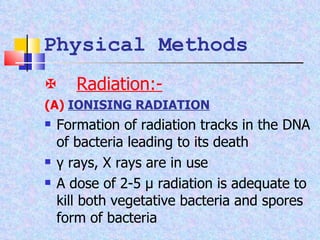
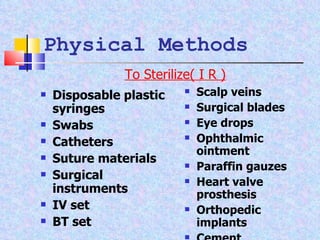
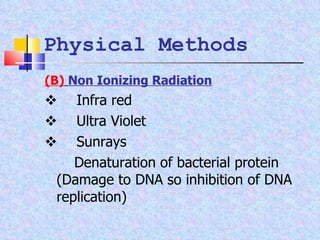
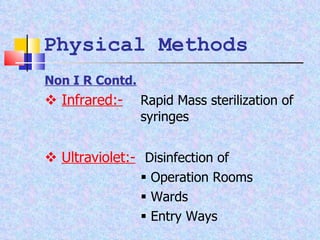
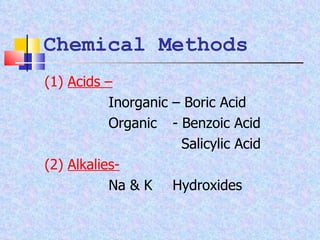
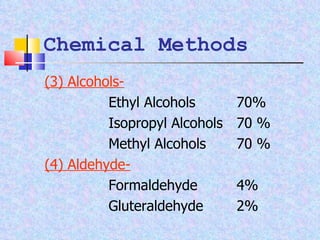
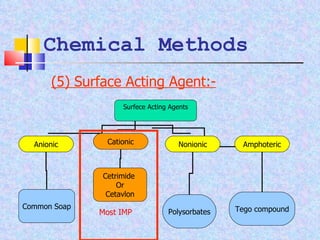
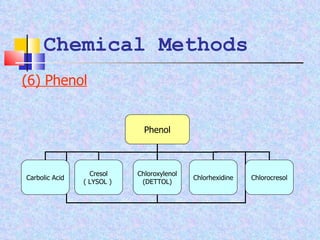
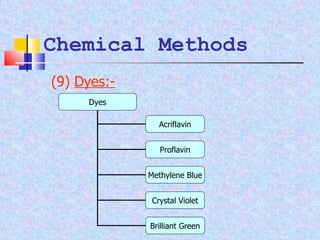
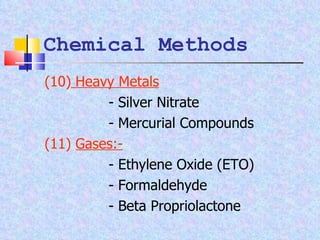
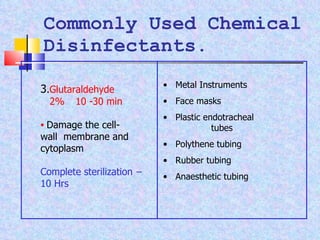
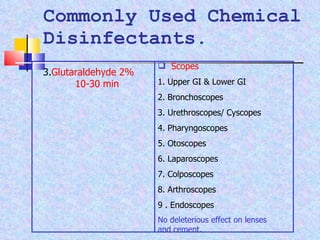
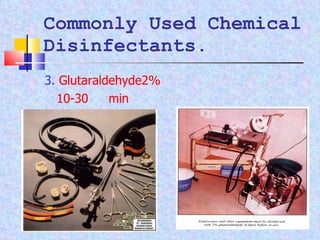
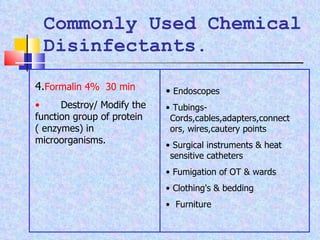
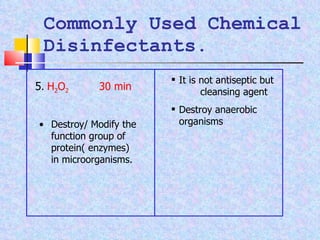
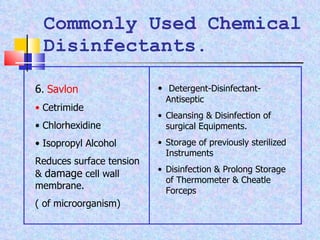
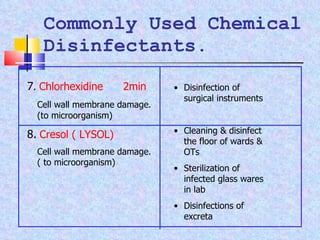
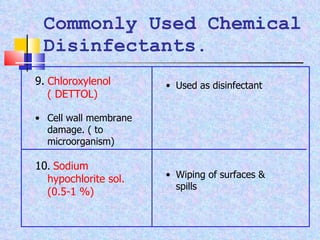
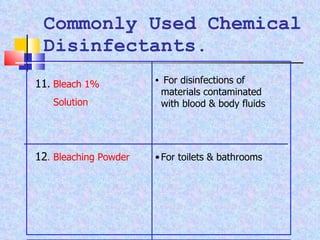
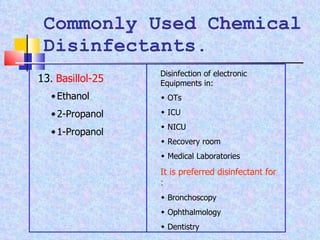
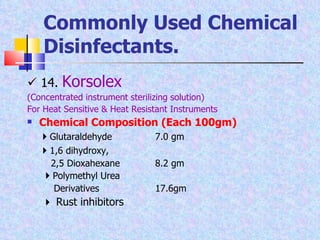
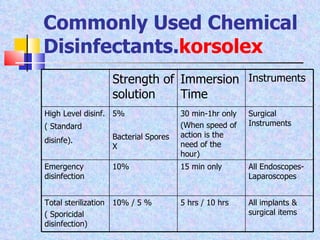
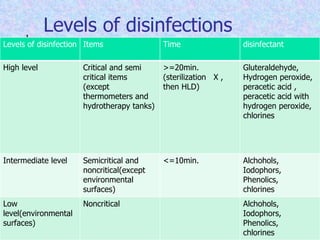
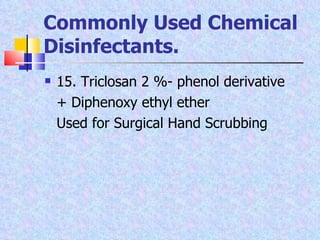
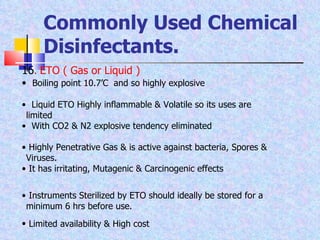
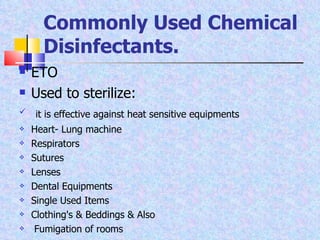
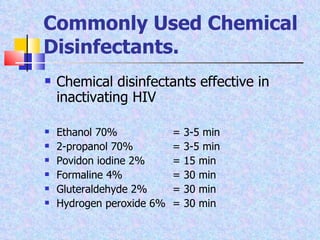
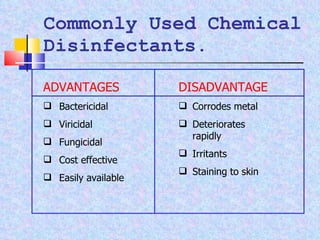
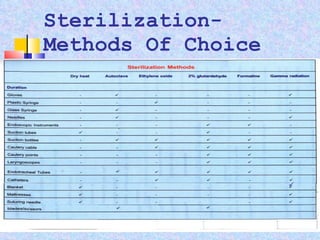
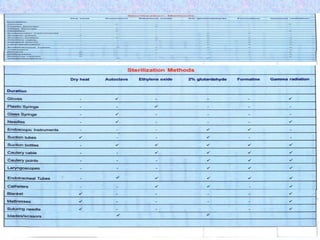
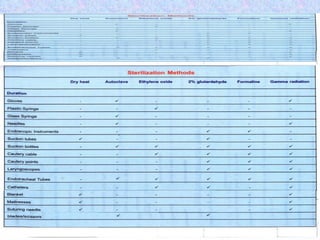
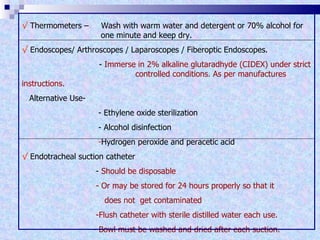
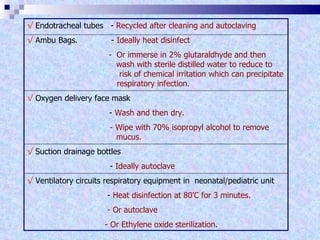
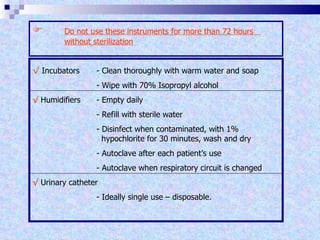
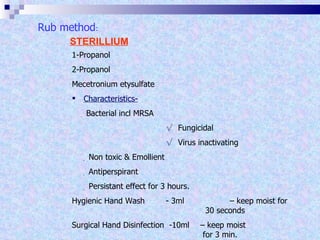
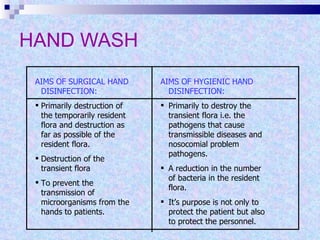
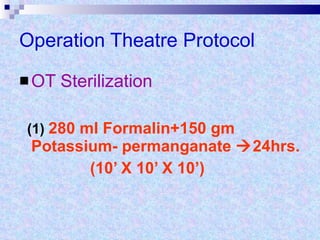
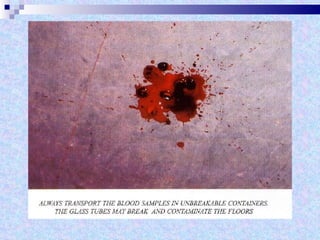
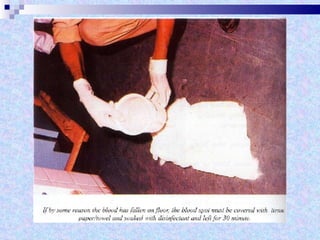
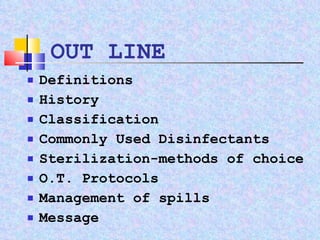
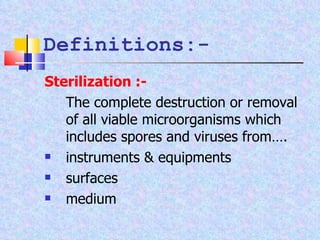
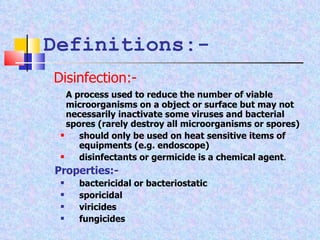
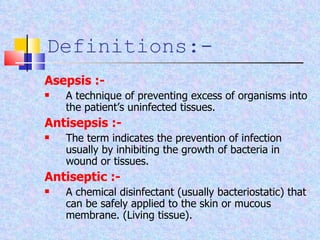
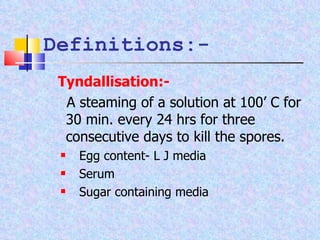
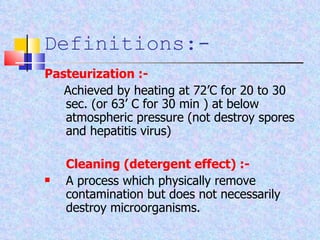
The document discusses sterilization and disinfection methods and commonly used disinfectants. It defines sterilization as destroying all microorganisms including spores and viruses, while disinfection reduces microorganisms but may not eliminate spores or viruses. Common sterilization methods include heat sterilization using dry heat, moist heat and autoclaving, as well as chemical methods using alcohols, aldehydes, halogens, and heavy metals. Commonly used disinfectants mentioned include ethanol, povidone iodine, glutaraldehyde, formalin, hydrogen peroxide, chlorhexidine, and chloroxylenol. The document also outlines different levels of disinfection.

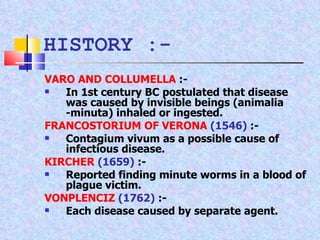
![ANTONY VAN LEEUWENHOCK (1683) [MICROSCOPE] :- Made accurate description at various types of bacteria and communated them to royal society of London. he called and acknowledged them as world of little animalcules. NEEDHAM (IRISH PRIEST) (1745-49) :- In 1745 published experiments purporting spontaneous generation (abiogenesis) of microorganisms in putrescible fluid. HISTORY :-](https://image.slidesharecdn.com/sterilizationfinal2003-100424085222-phpapp01/85/Sterilization-10-320.jpg)