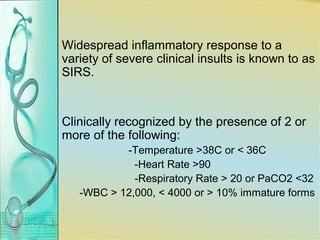
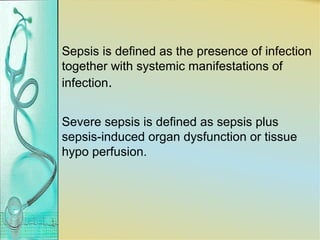
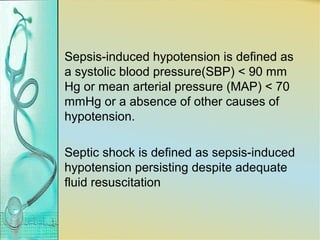
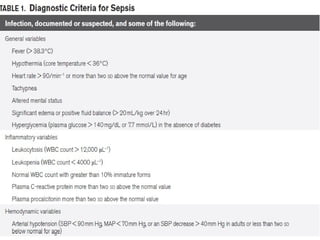
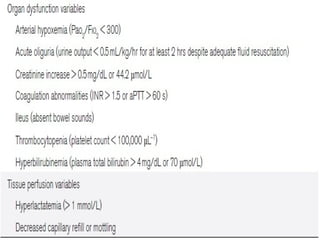
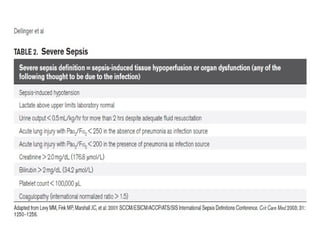
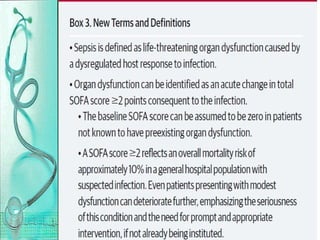
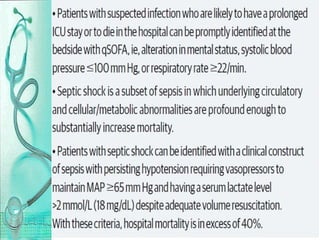
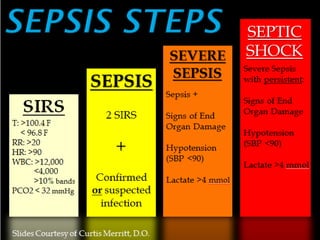
1. Sepsis is a major cause of morbidity and mortality worldwide, with mortality rates ranging from 15-60% depending on the severity. The guidelines provide recommendations for the management of sepsis, severe sepsis, and septic shock.
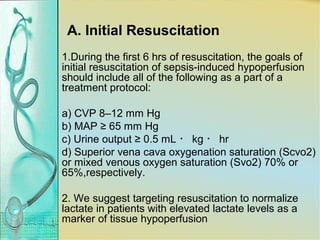
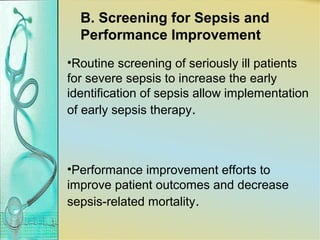
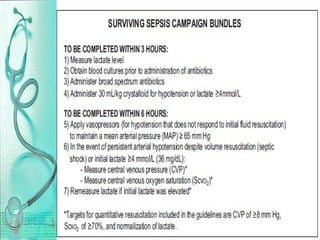
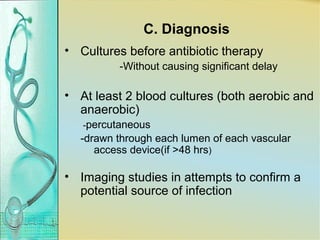
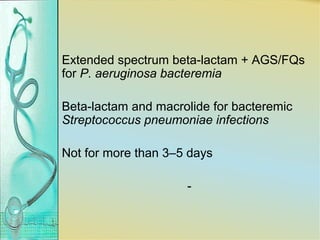
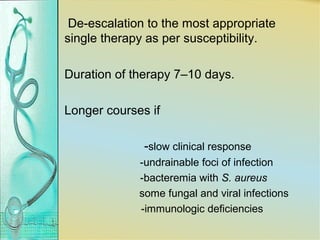
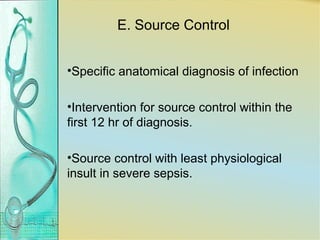
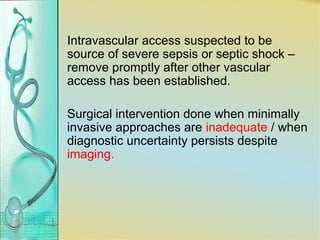
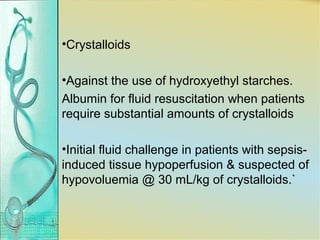
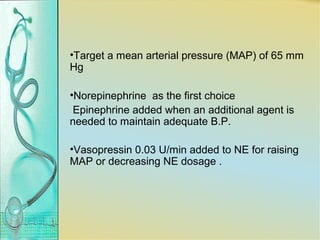
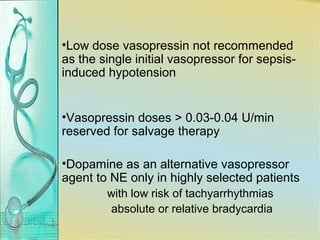
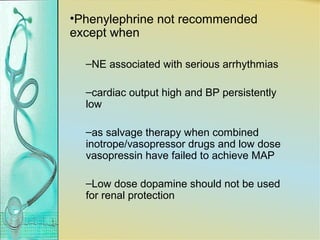
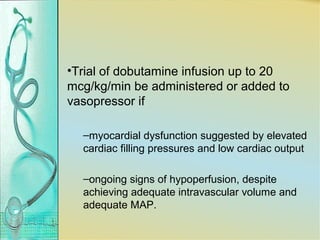
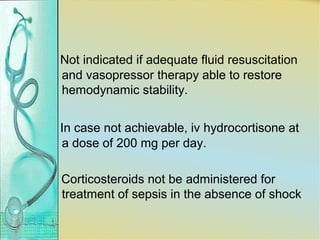
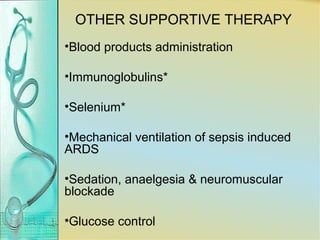
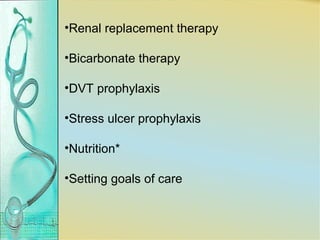
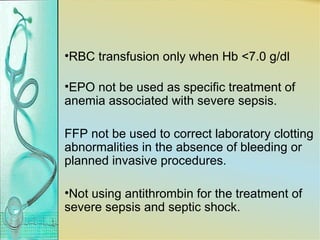
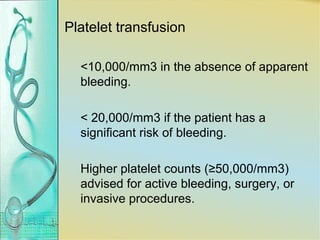
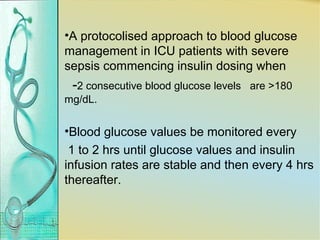
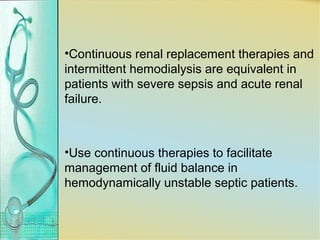
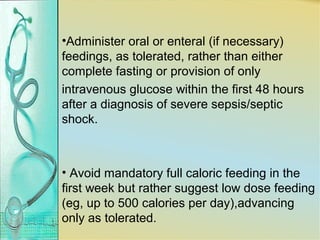
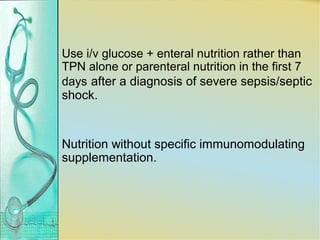
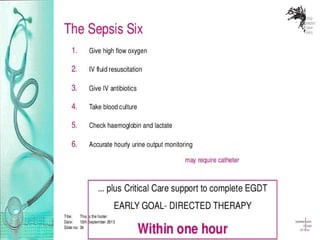
2. The initial focus is on early recognition and treatment within the first hour including antibiotics, fluid resuscitation, lactate monitoring, and source control. Vasopressors, inotropes, steroids and other supportive care measures are also addressed.
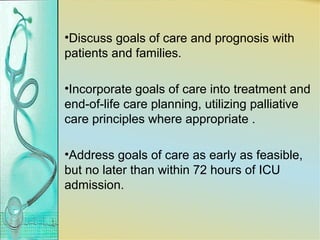
3. Goals are to diagnose and treat the infection while restoring tissue perfusion and organ function through a coordinated response and supportive therapies.