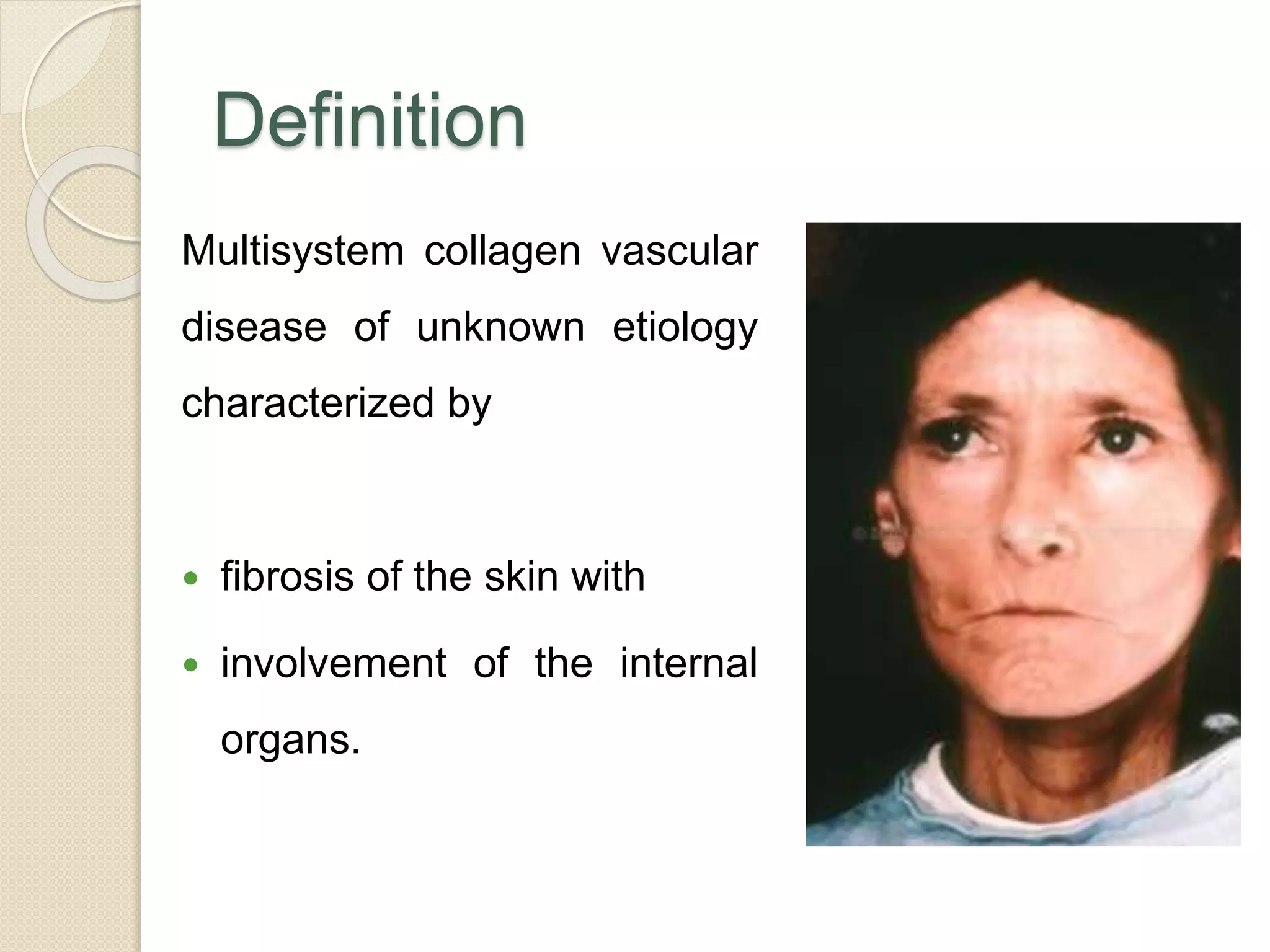
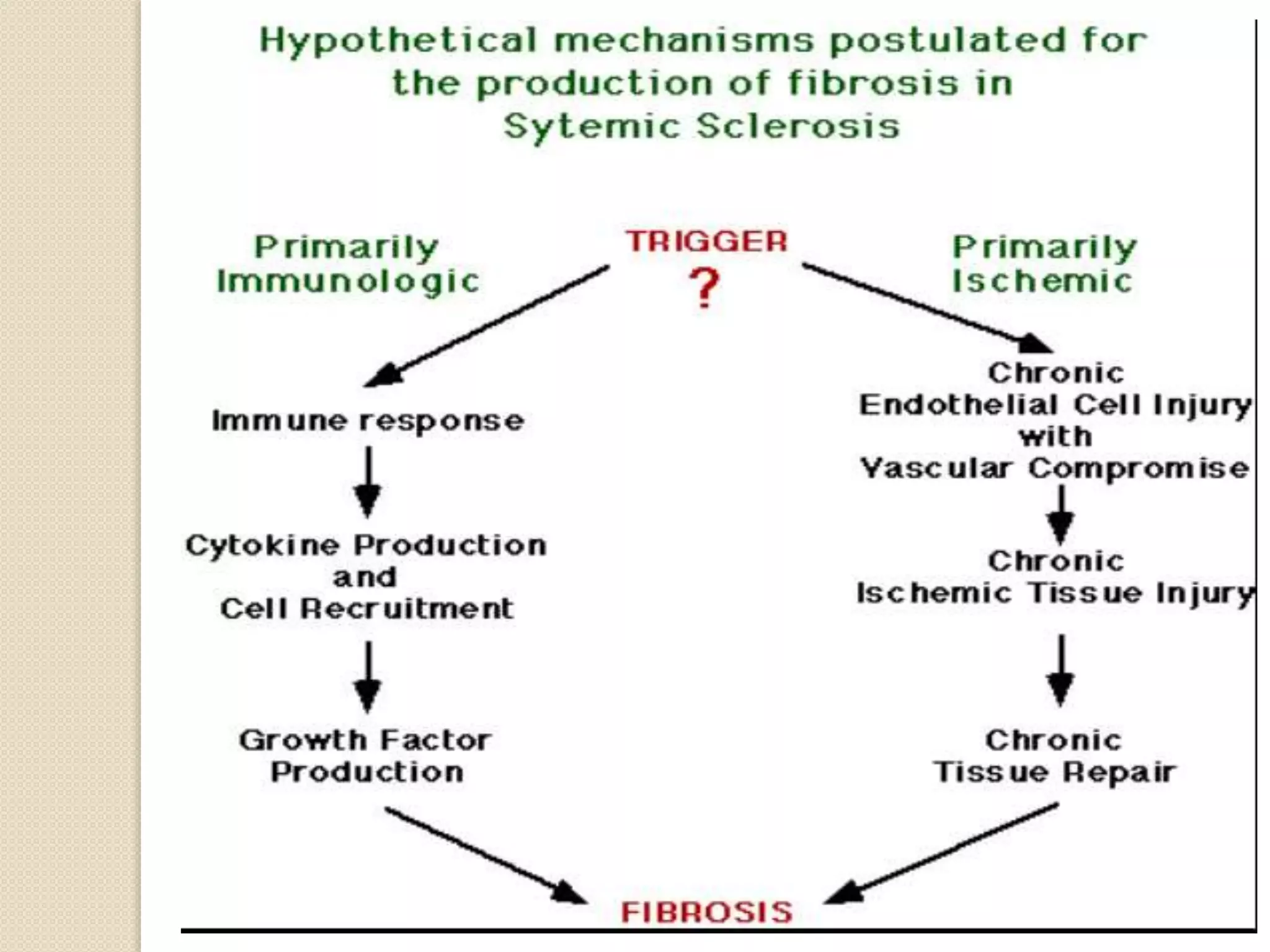
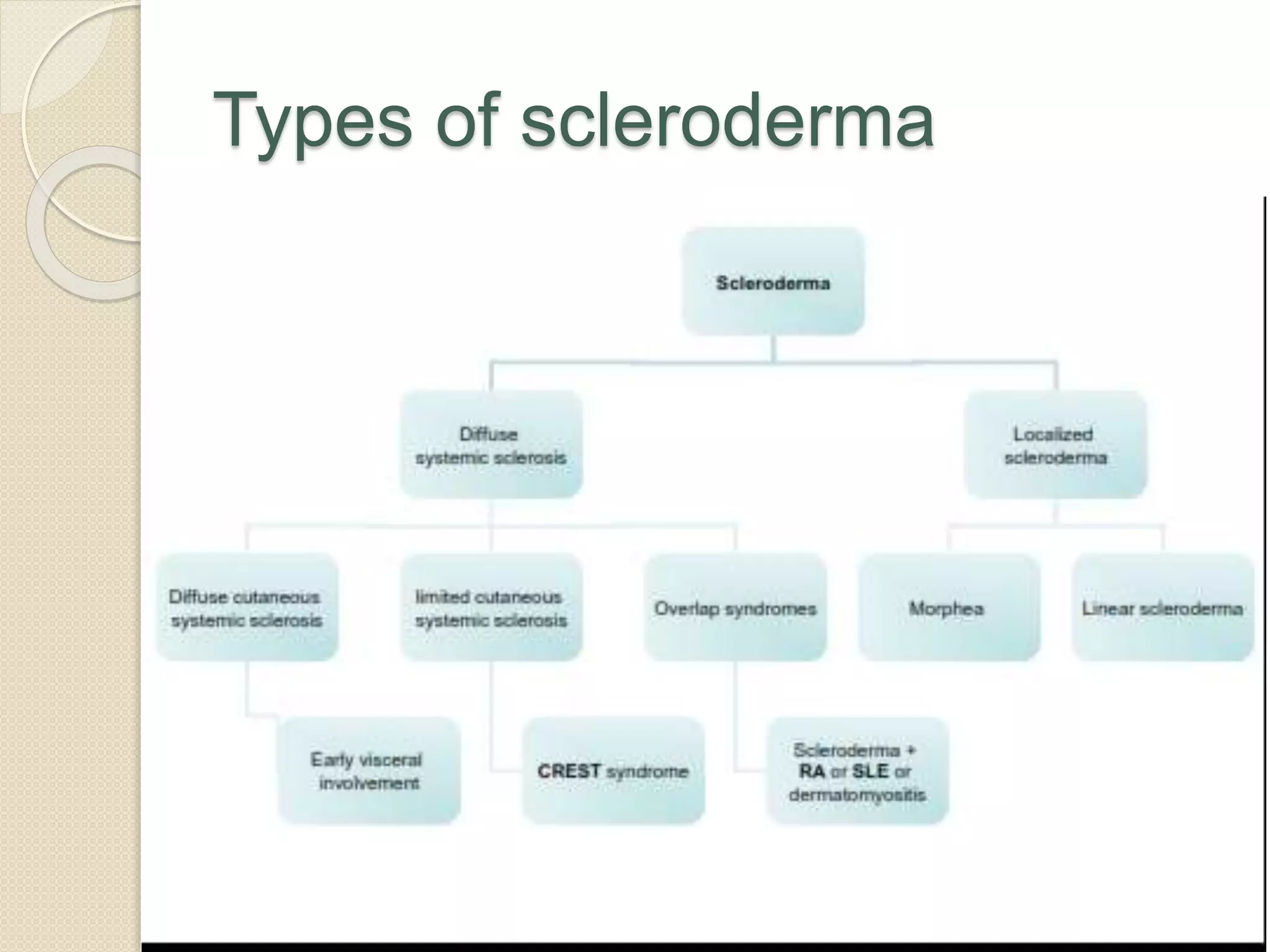
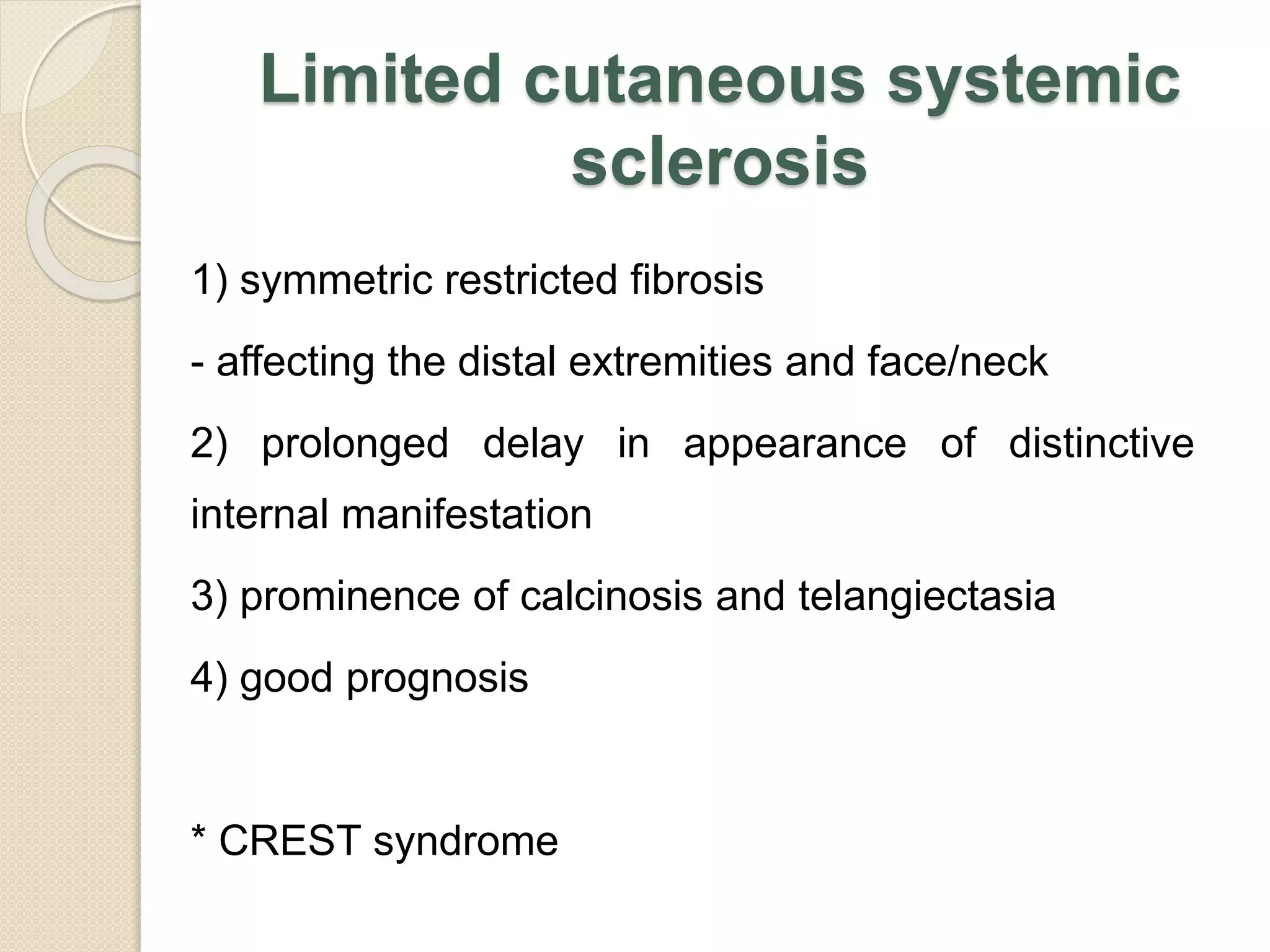
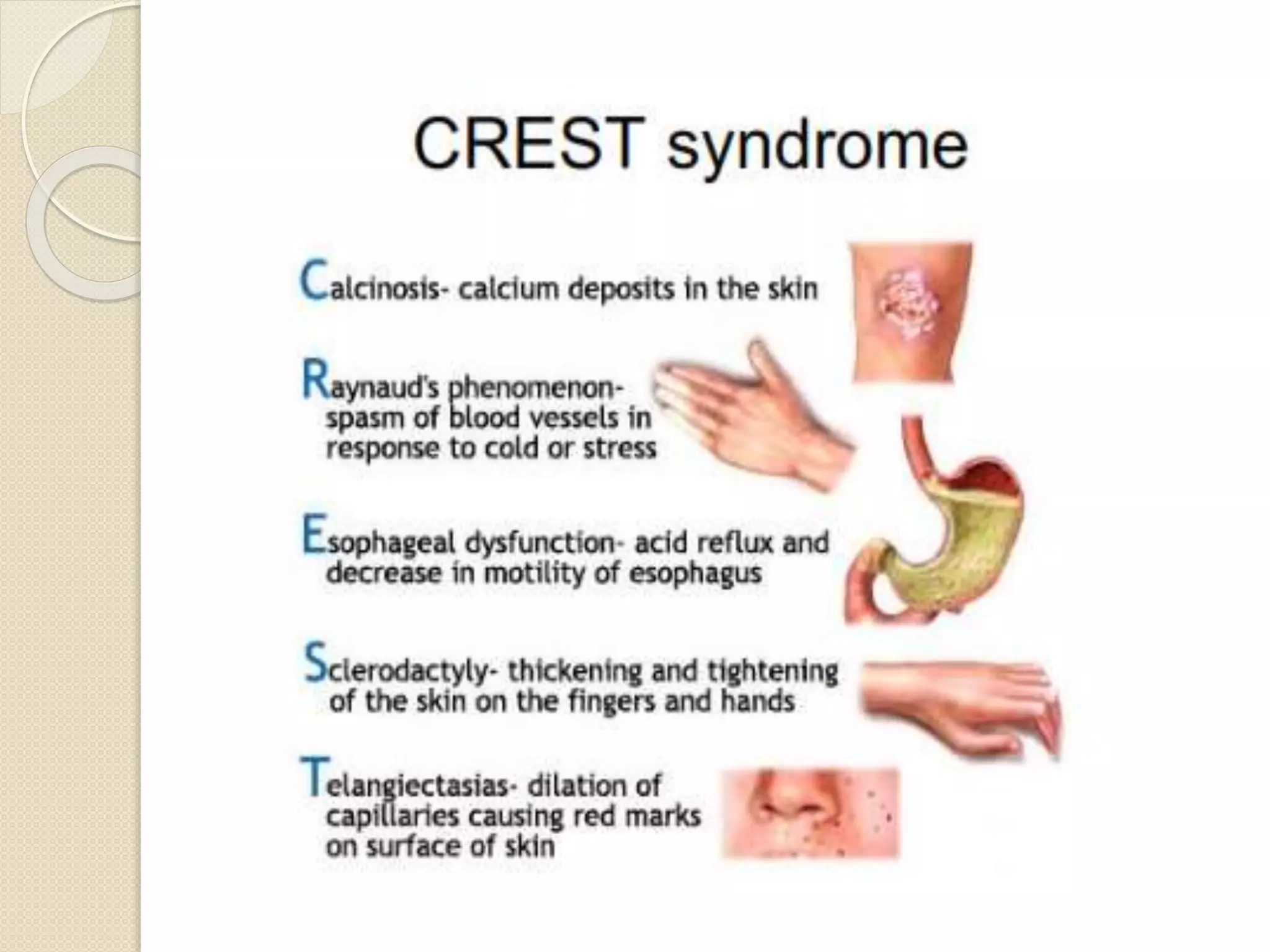
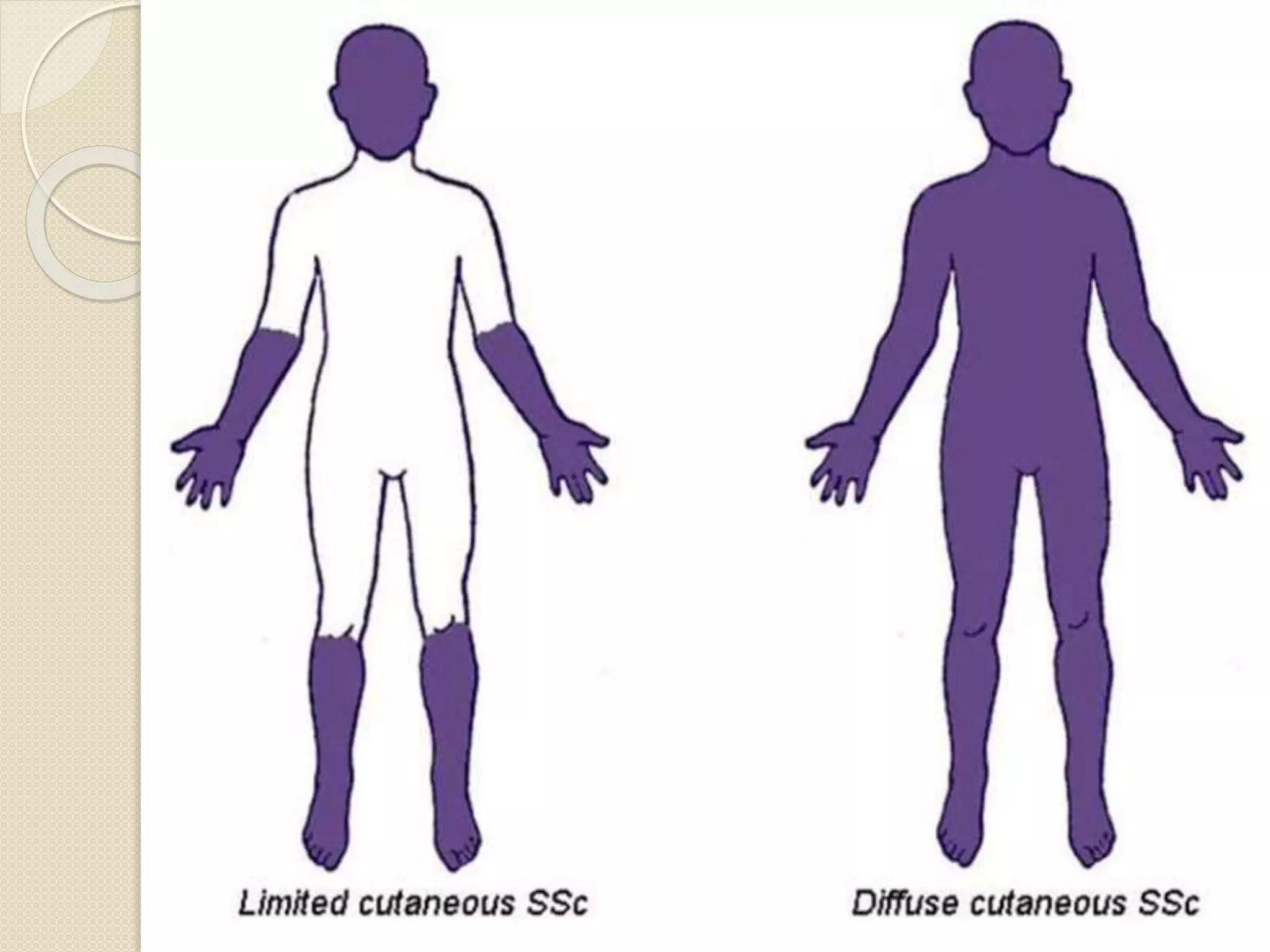
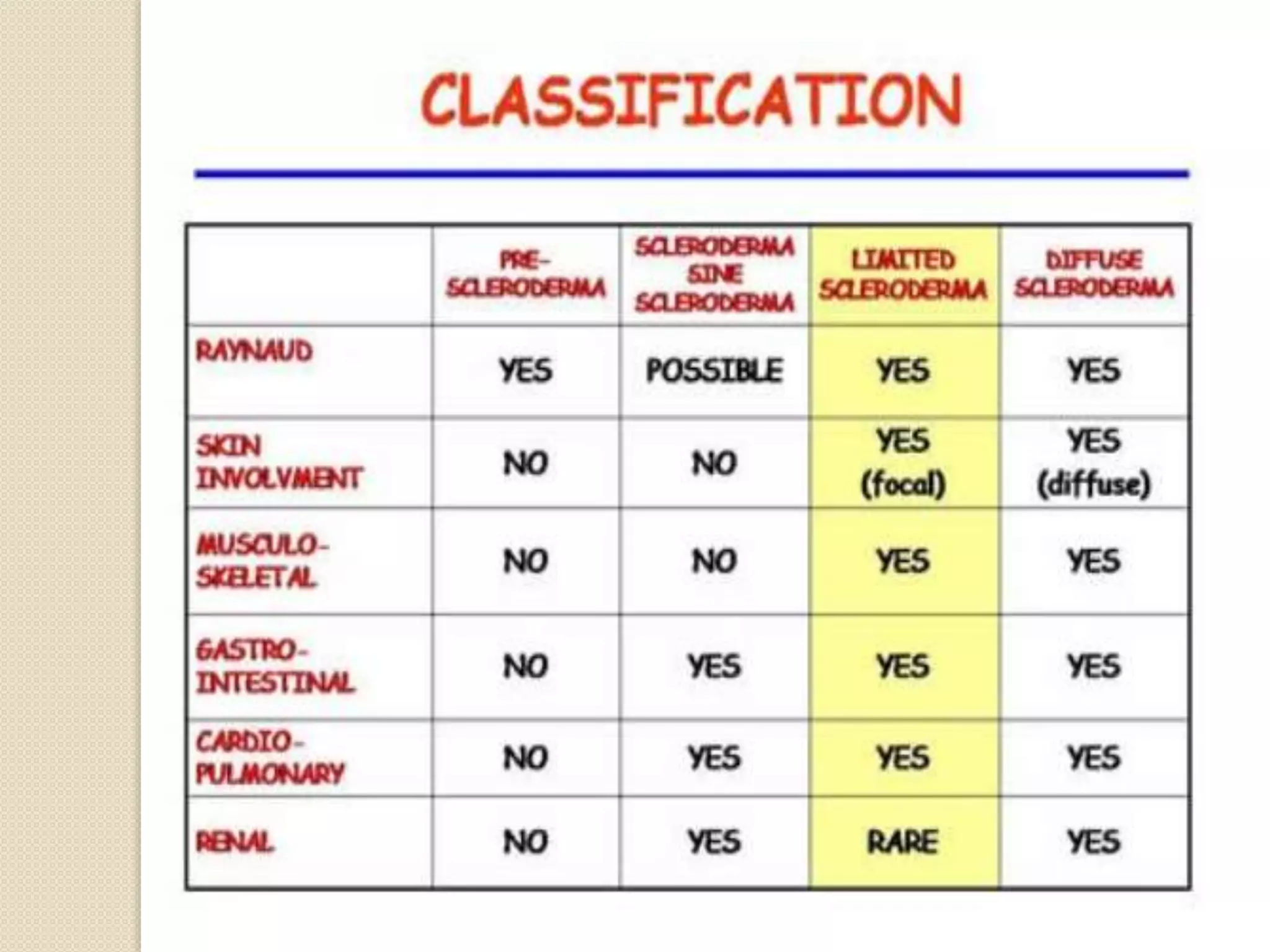
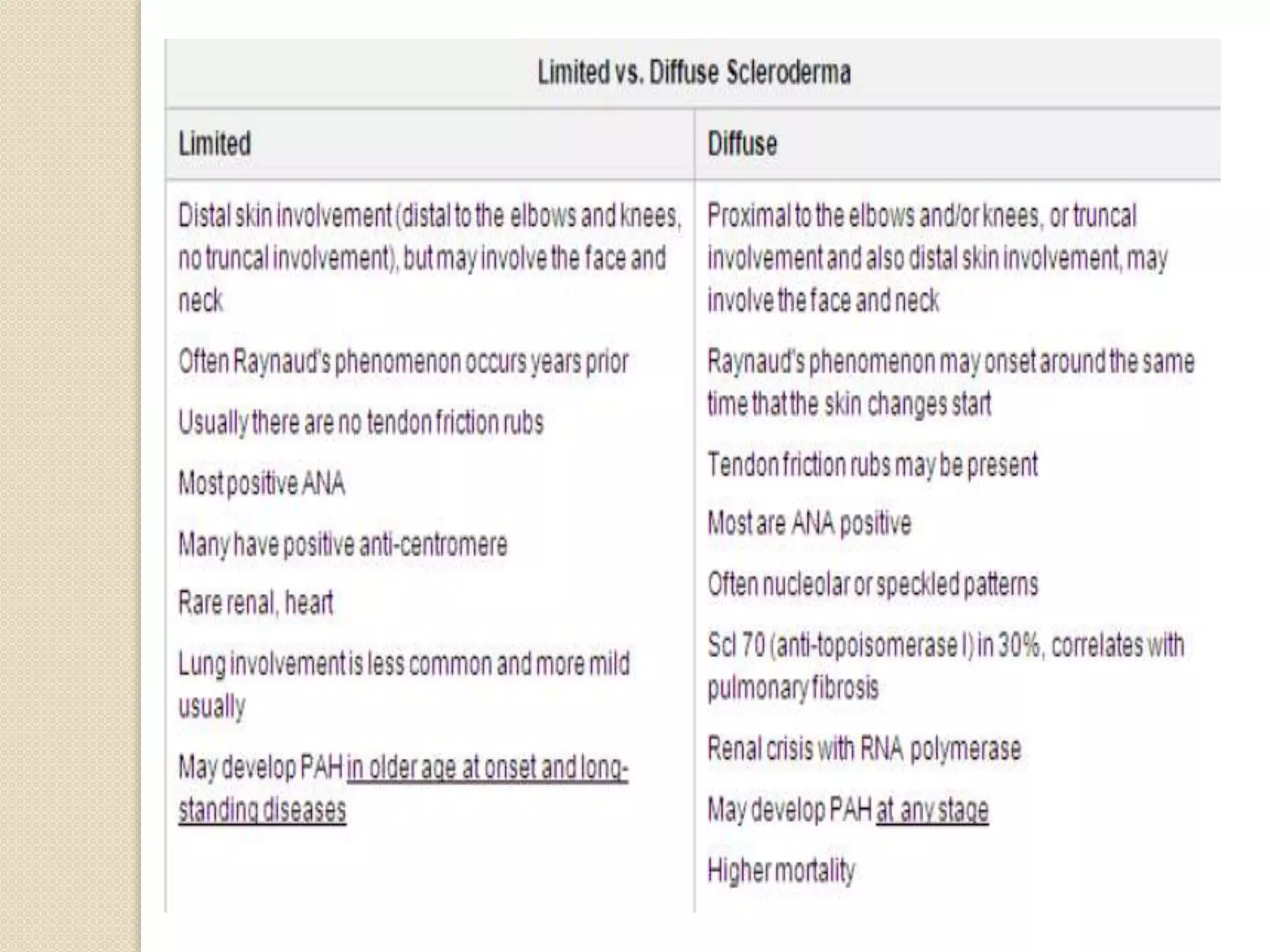
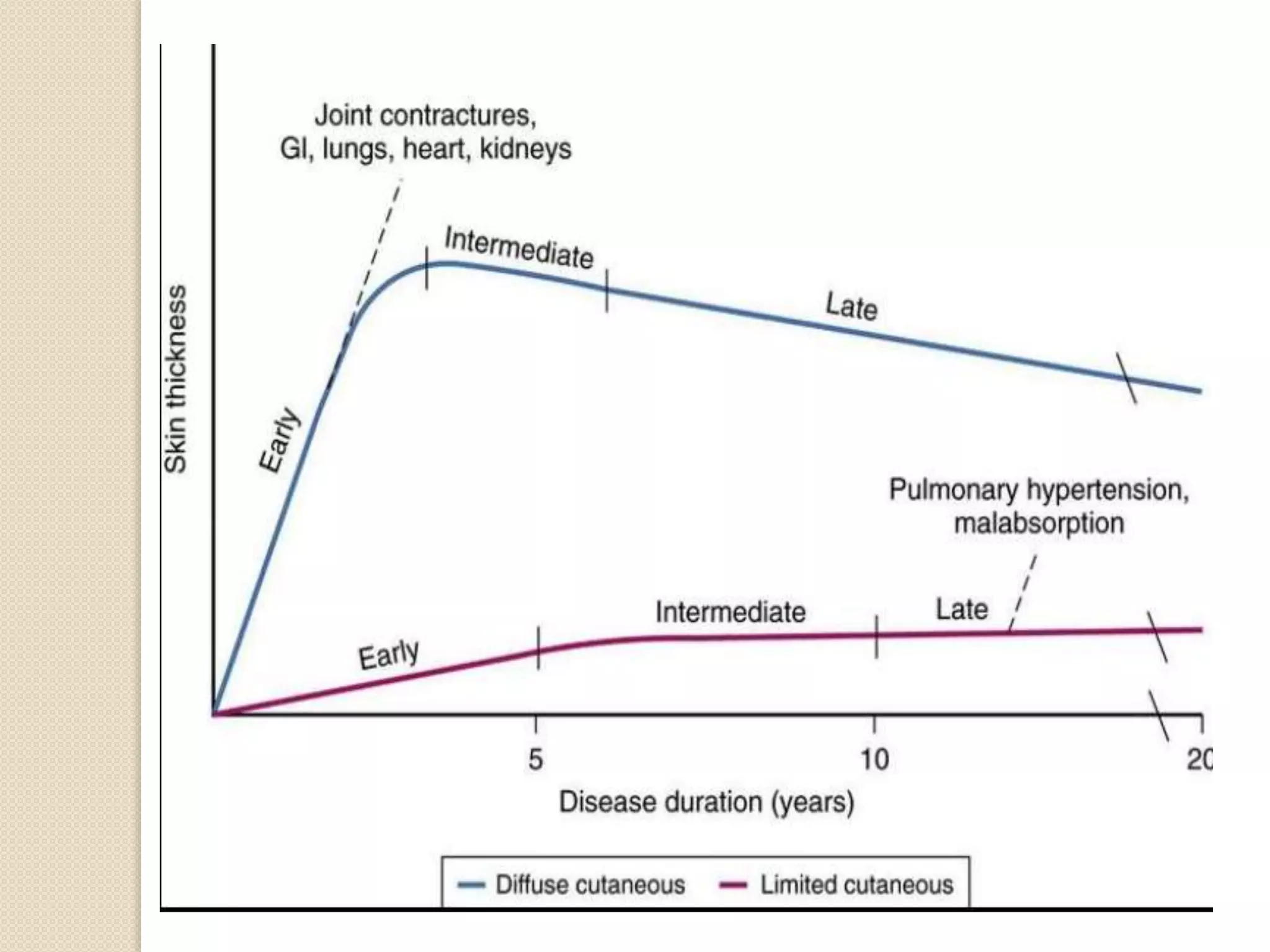
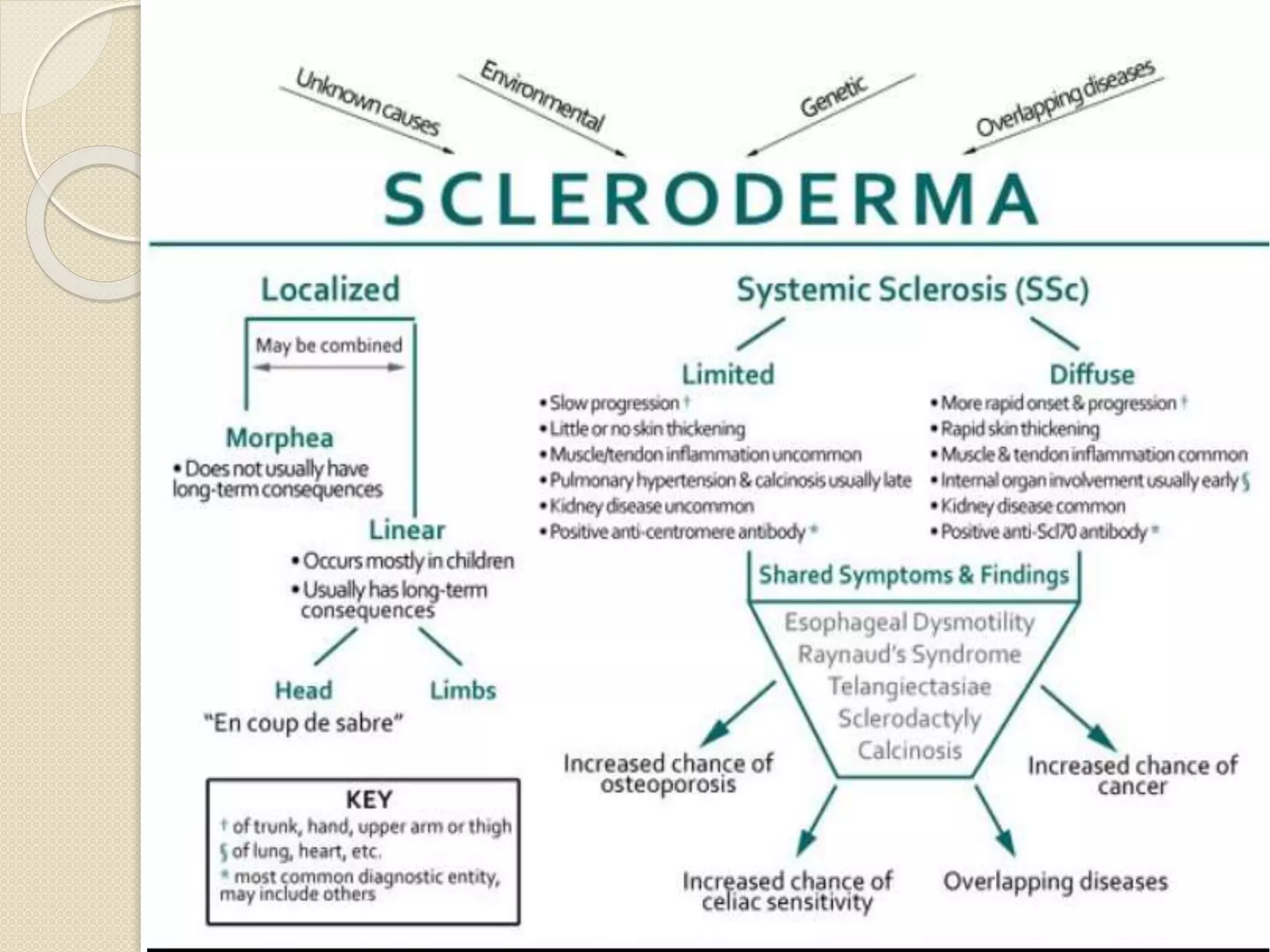
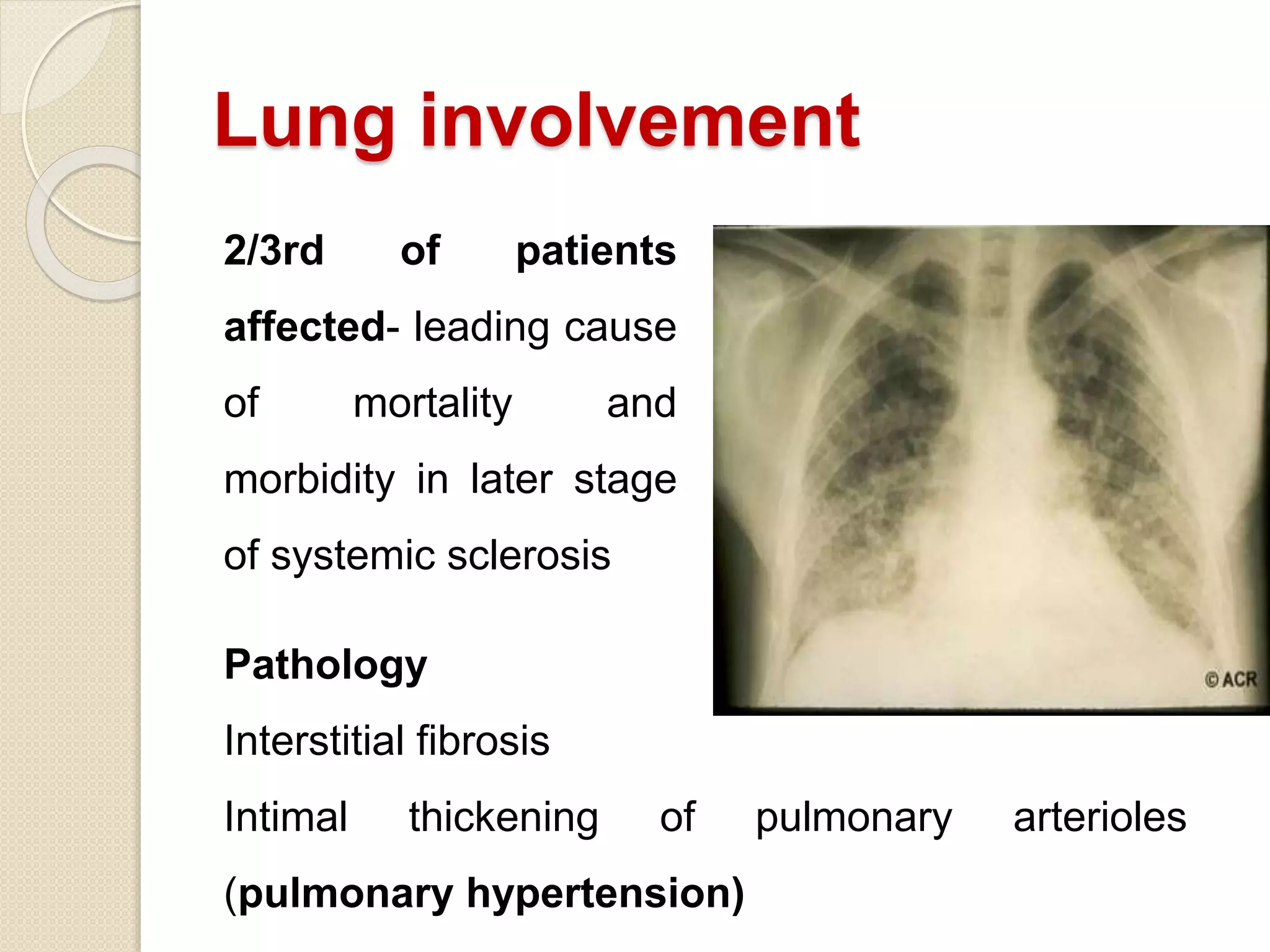
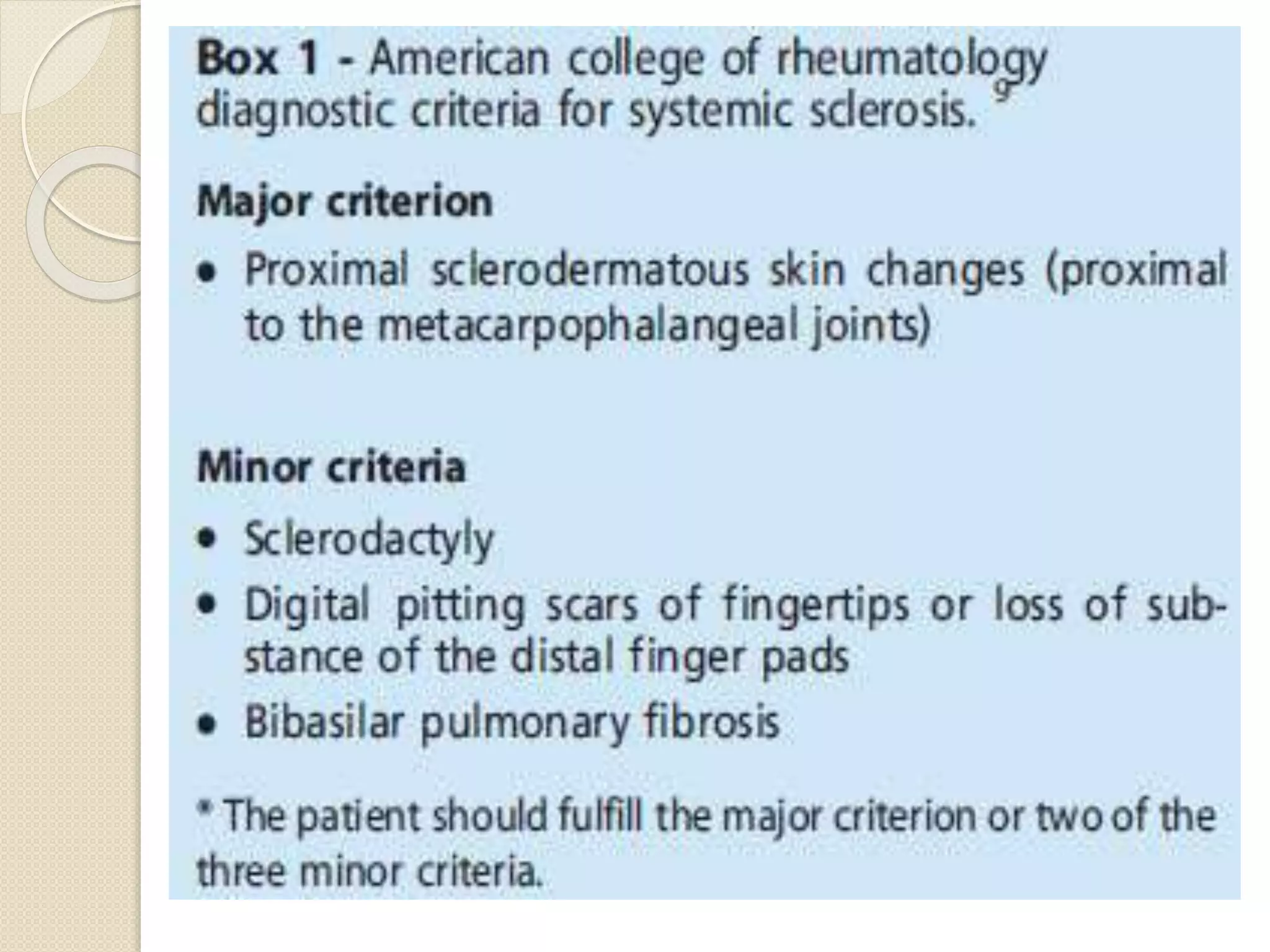
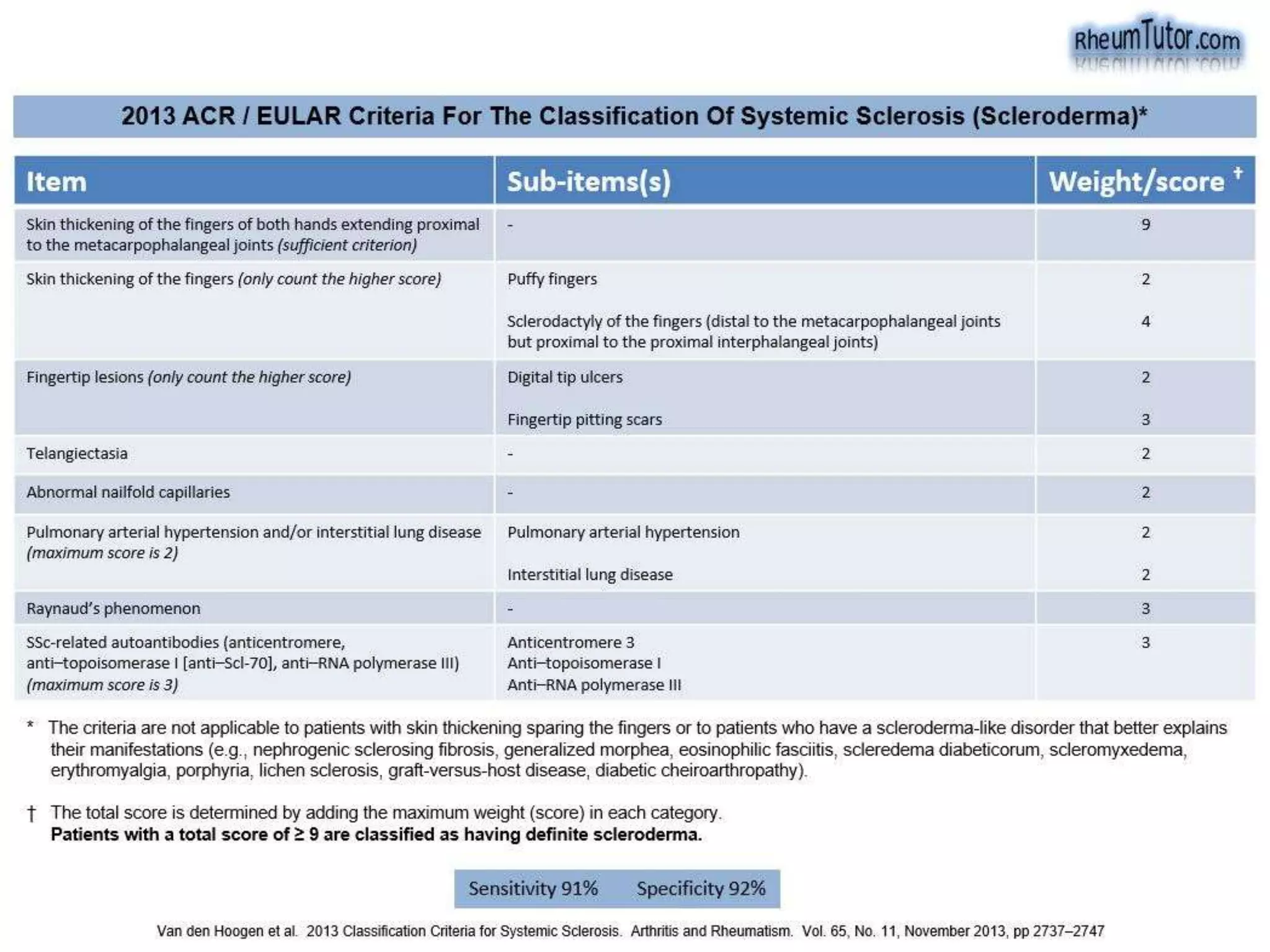
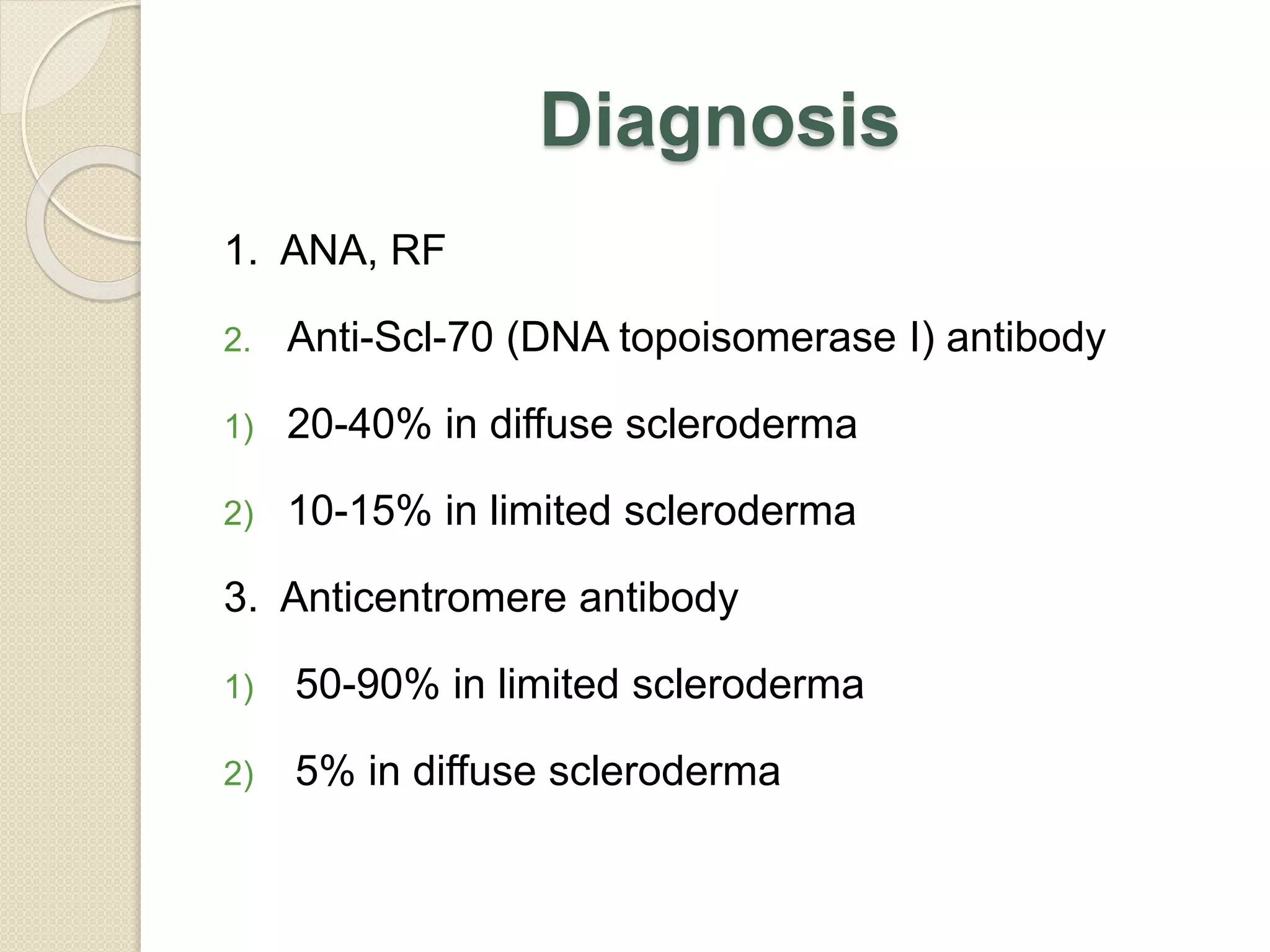
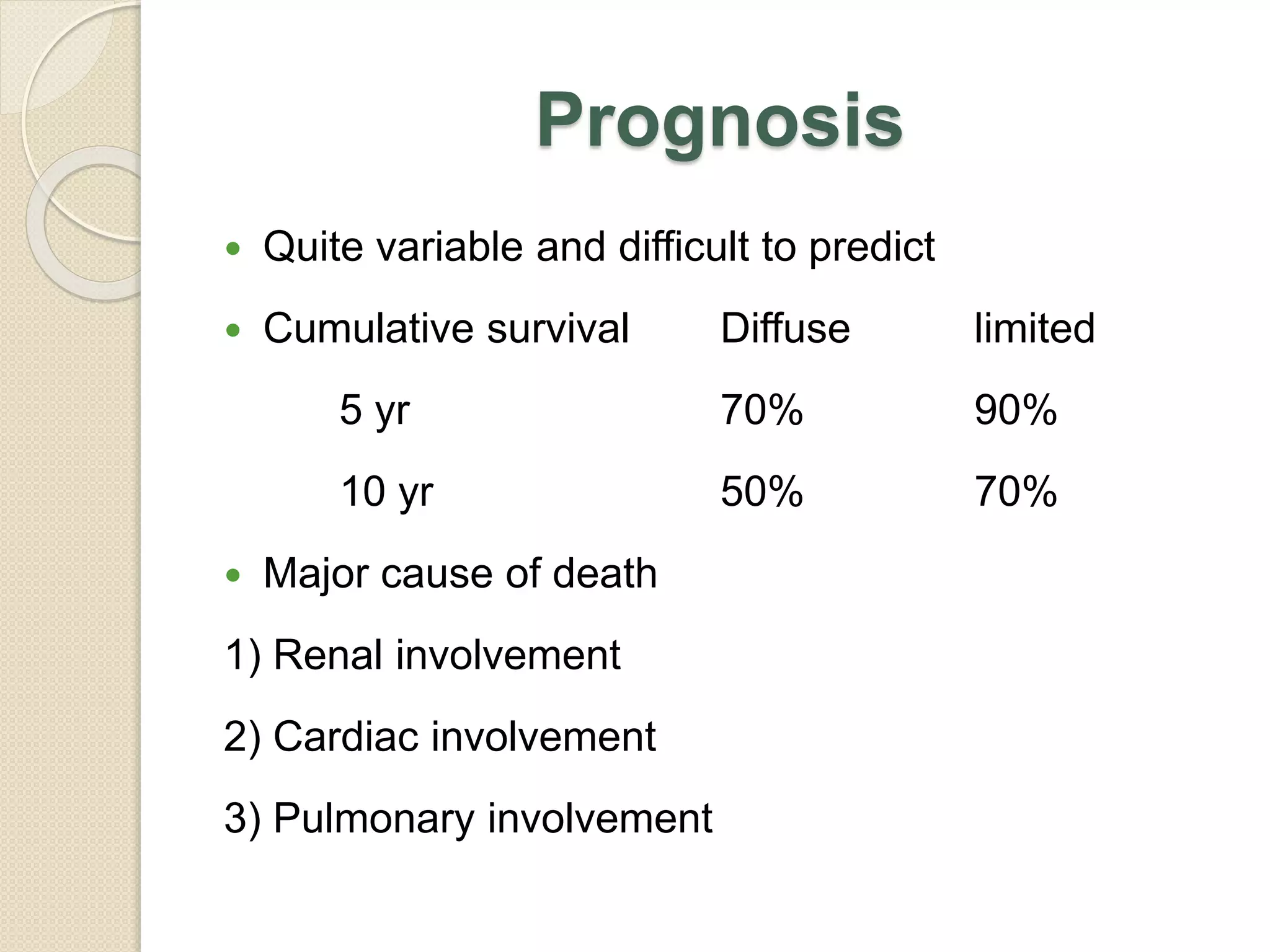
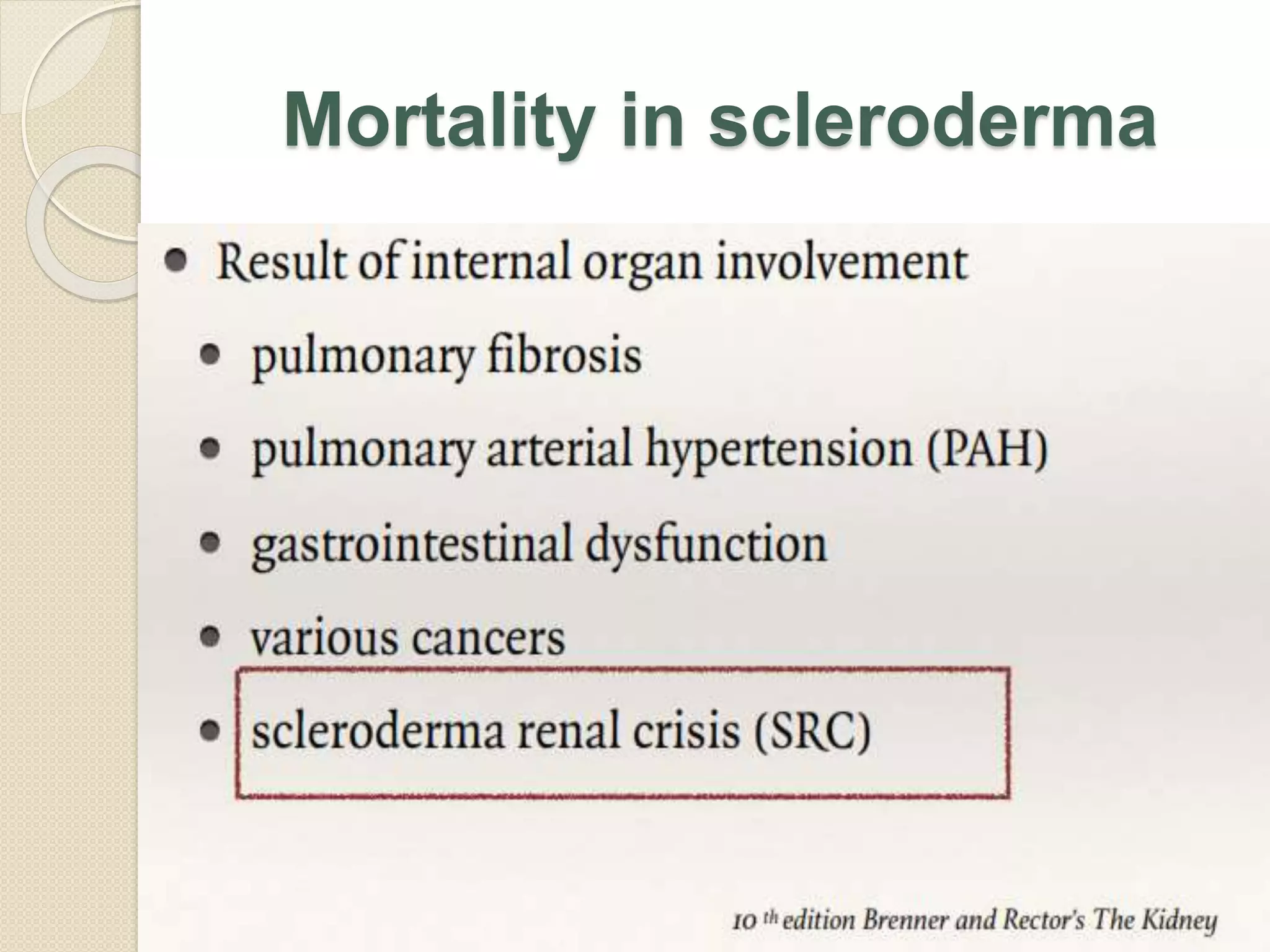
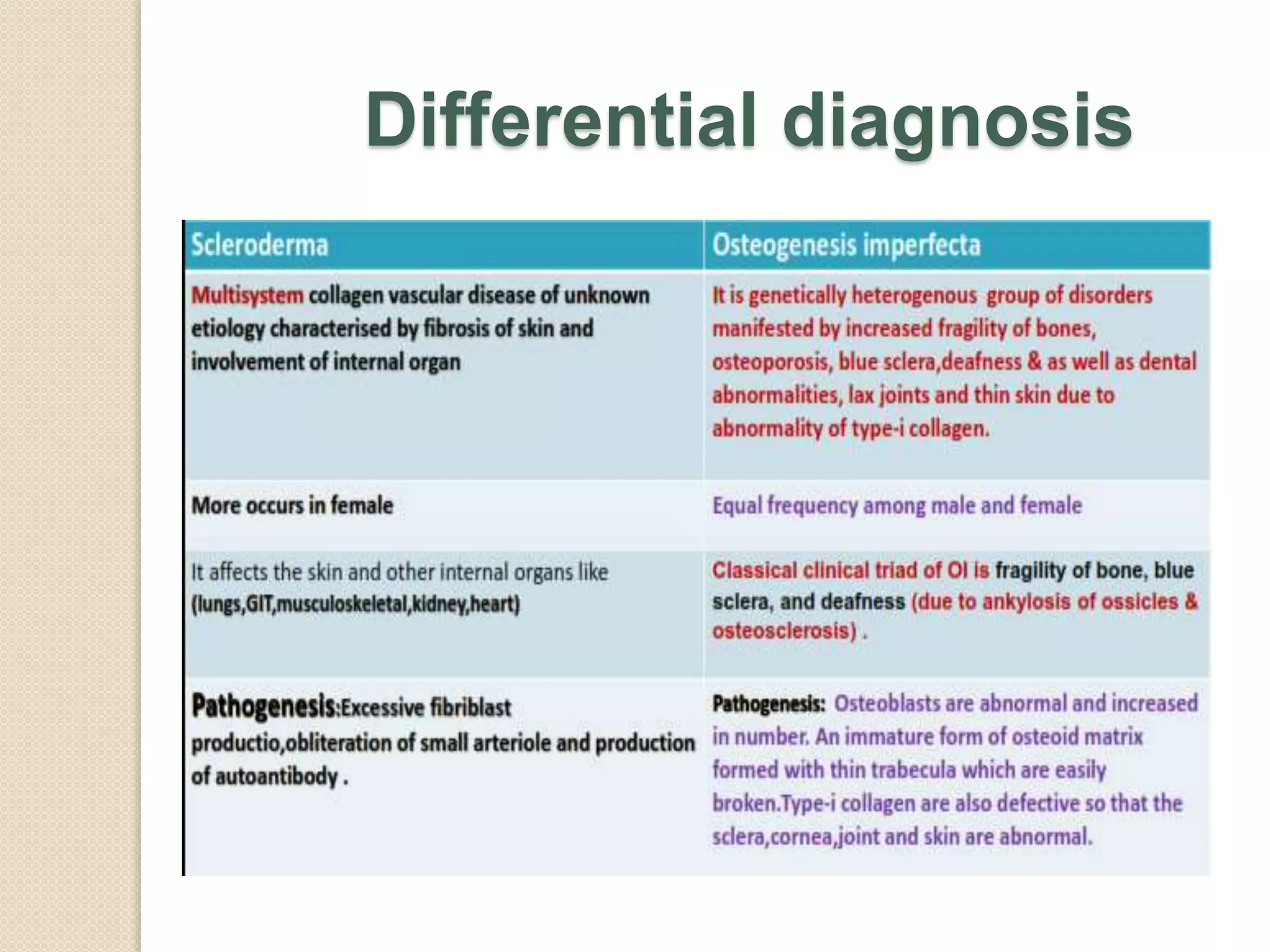
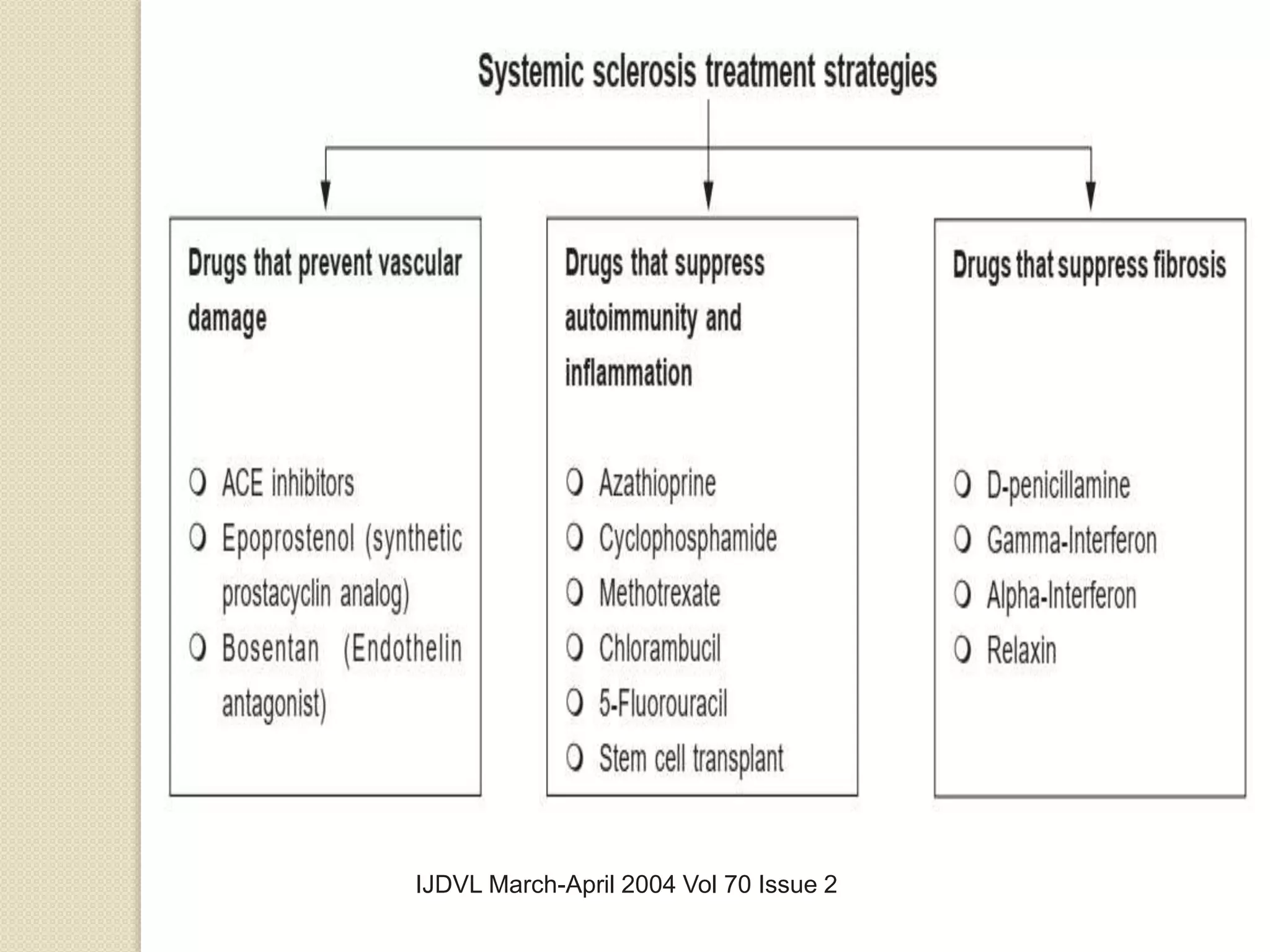
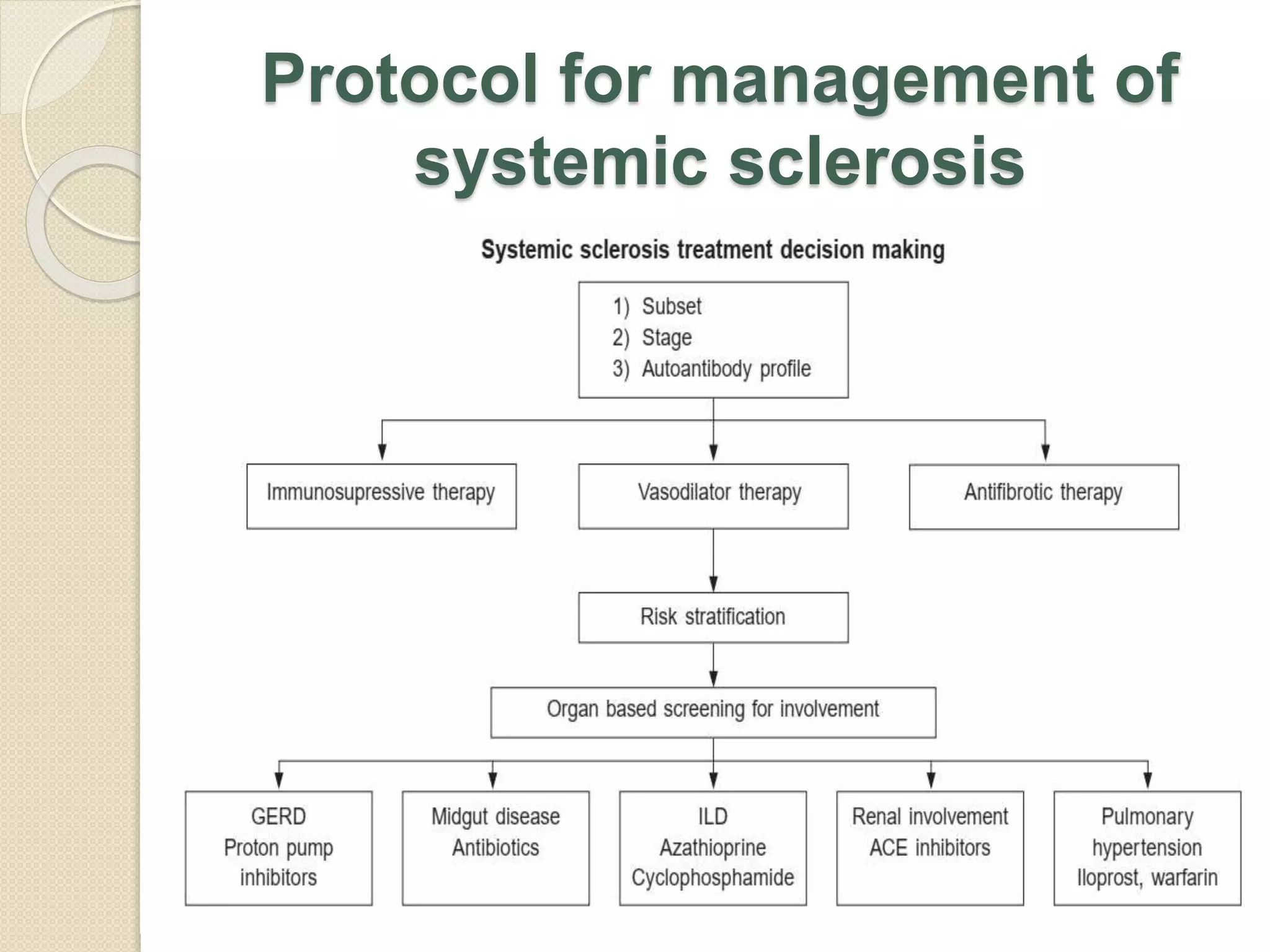
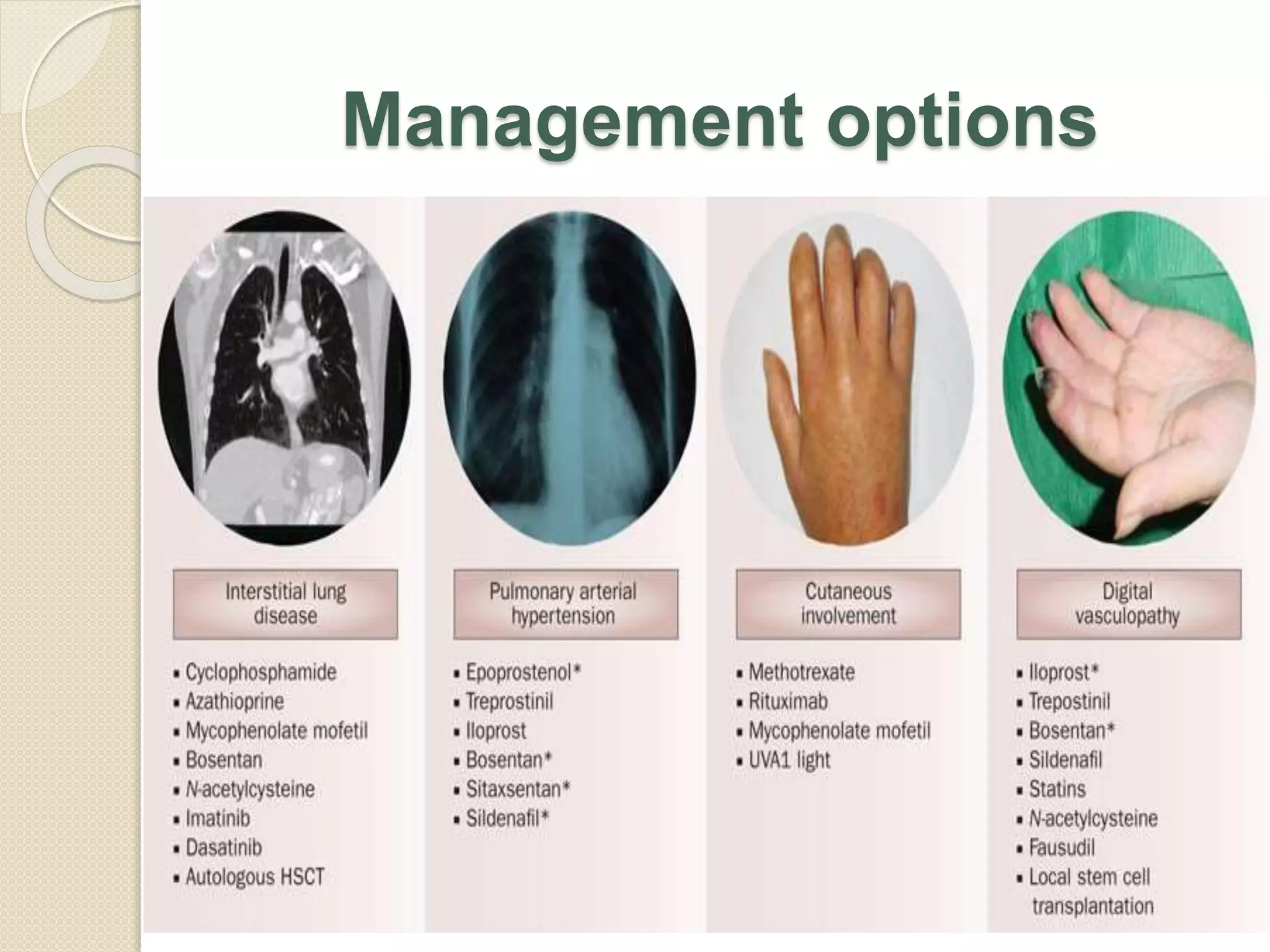
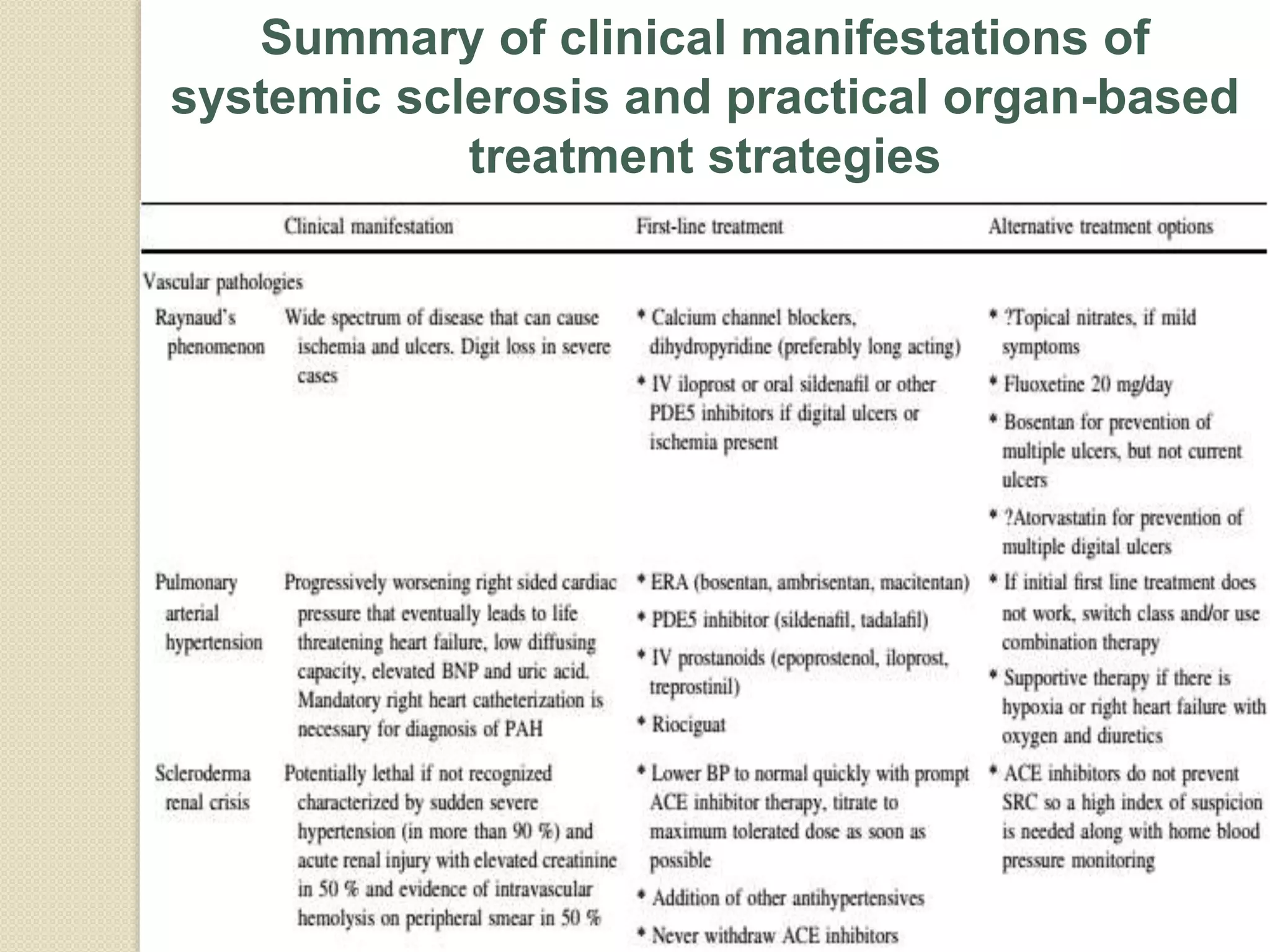
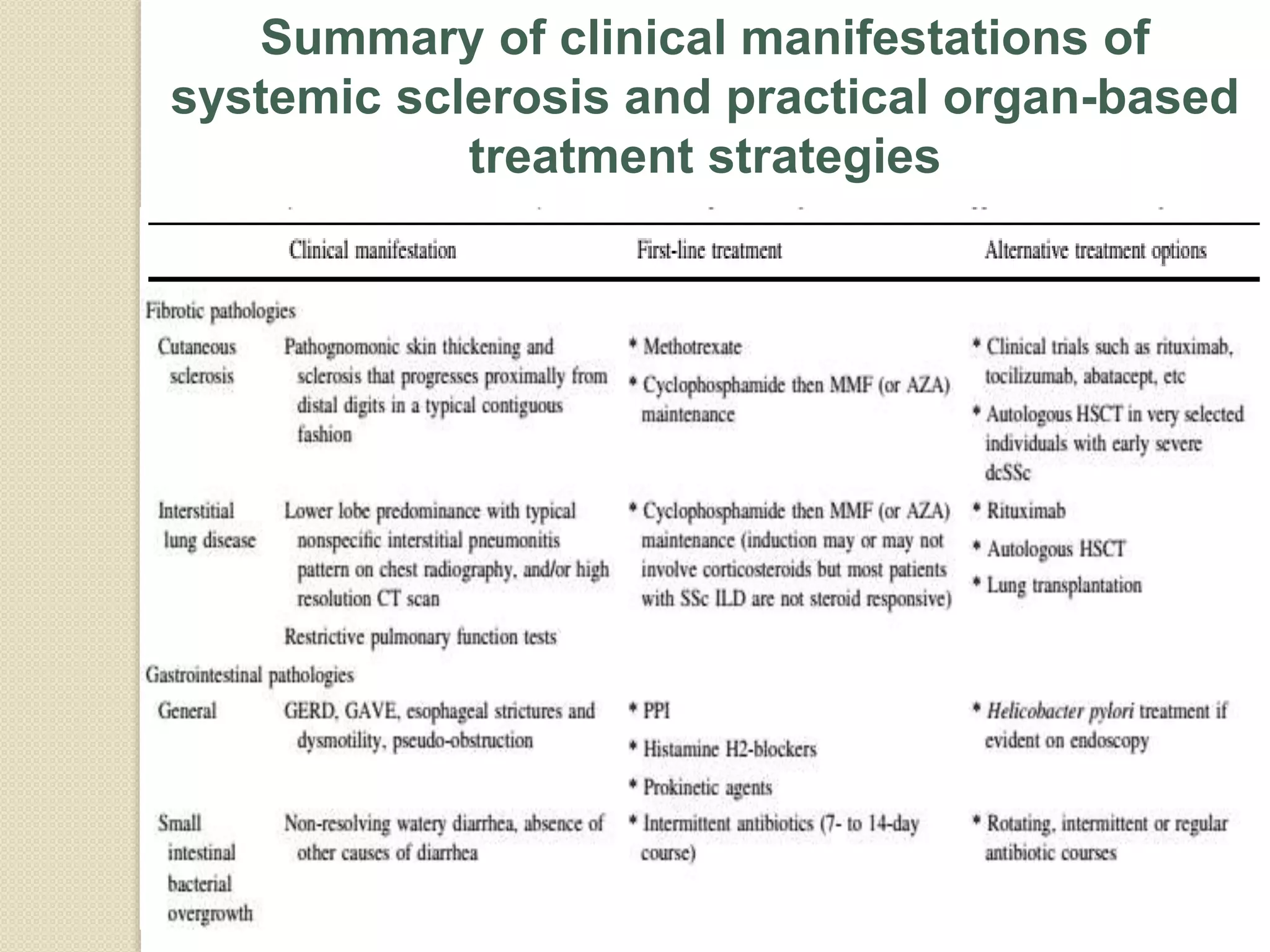
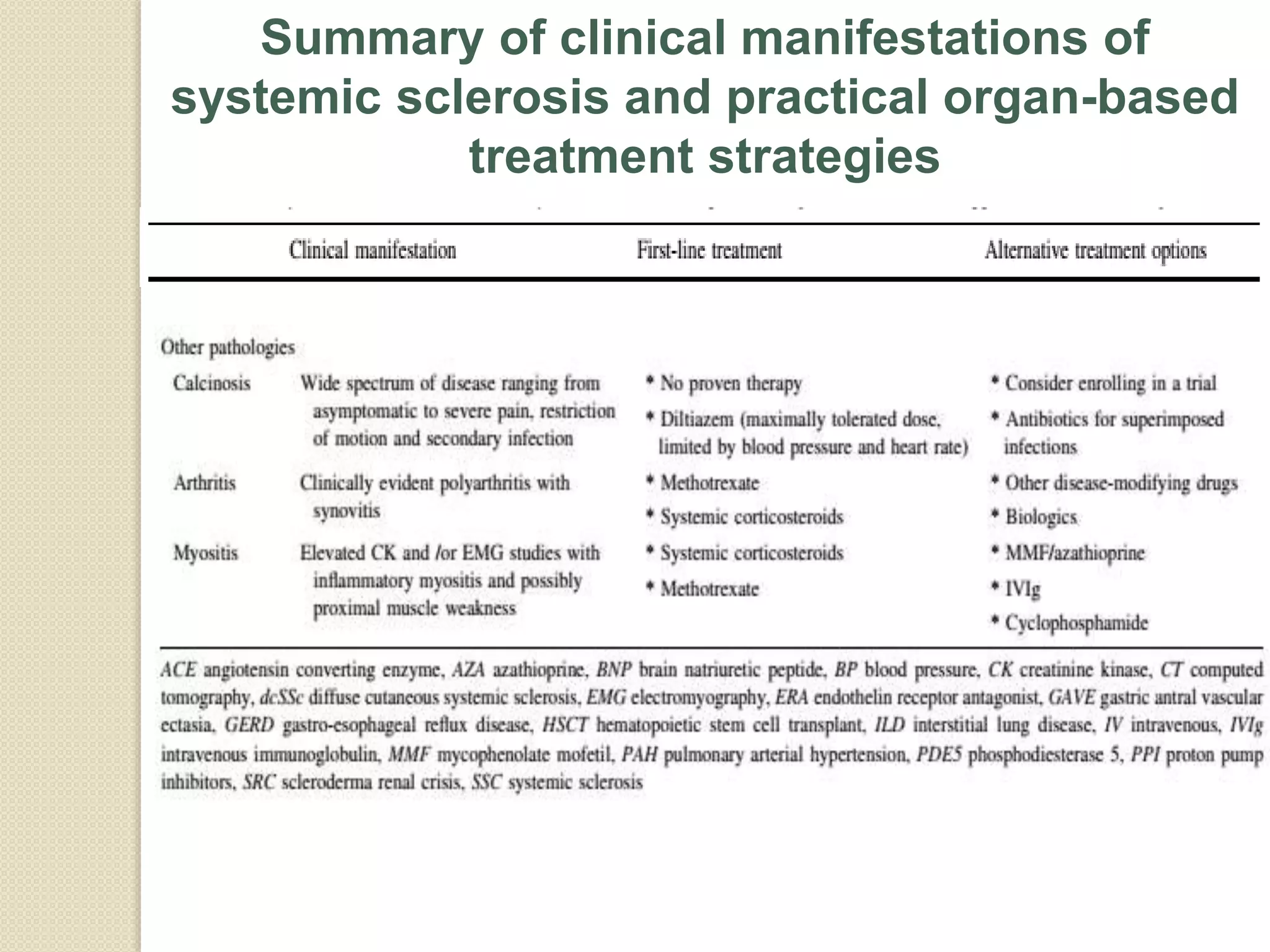
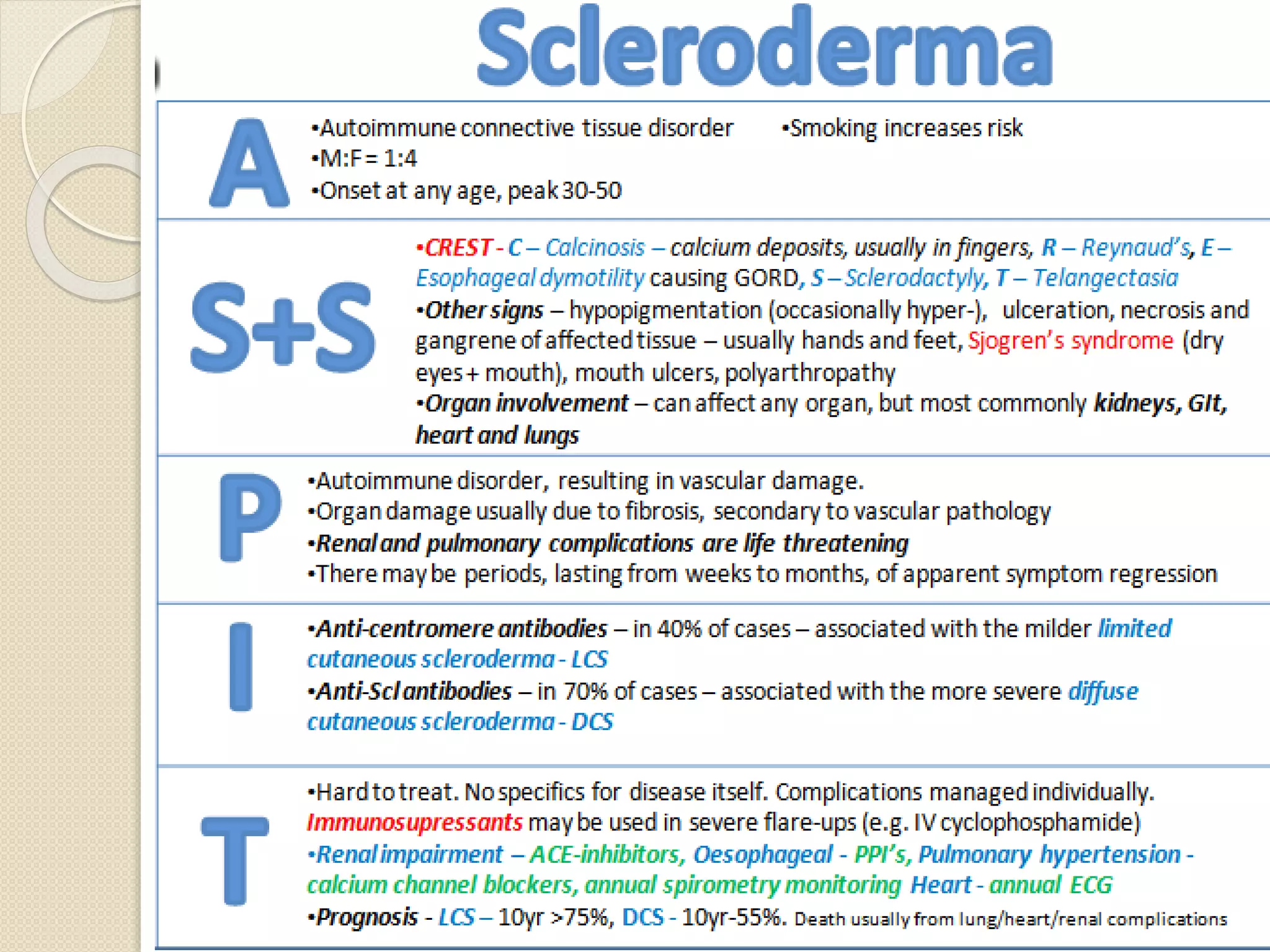
Scleroderma is a multisystem collagen vascular disease characterized by fibrosis of the skin and internal organs. It results from endothelial cell injury, fibroblast activation, and immune system involvement. The two main types are limited cutaneous systemic sclerosis, which affects the skin of the hands and face, and diffuse cutaneous systemic sclerosis, which has more extensive skin involvement. Major organ manifestations include pulmonary fibrosis, gastrointestinal tract abnormalities, heart and kidney involvement. Treatment focuses on preventing further organ damage through immunosuppression and addressing specific organ system complications.