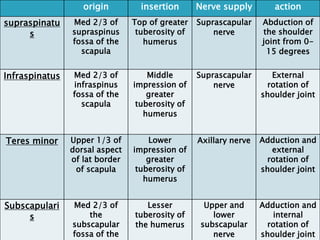
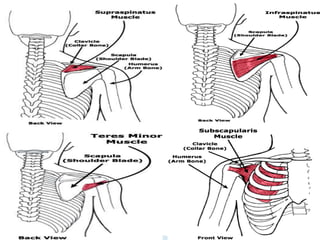
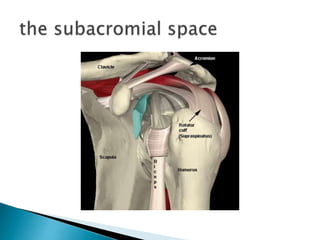
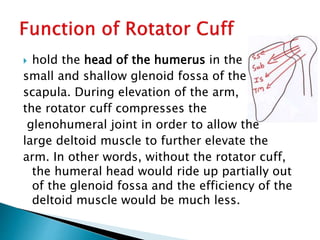
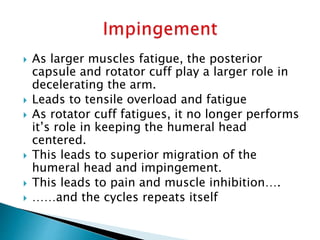
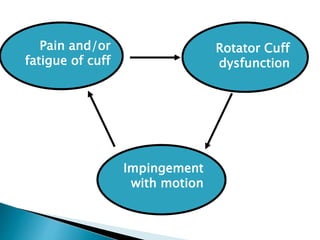
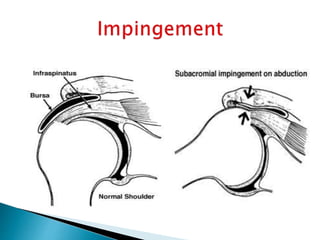
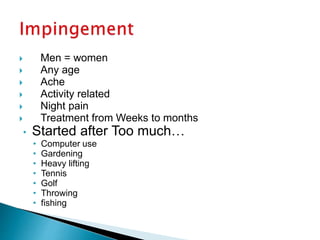
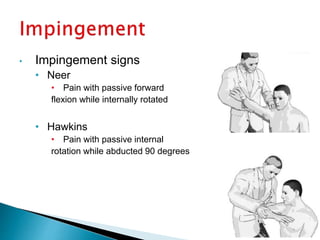
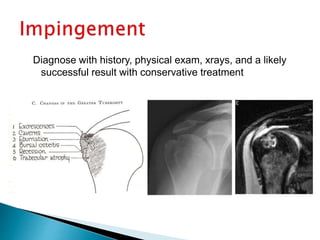
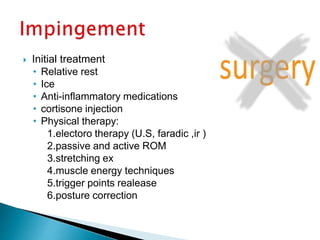
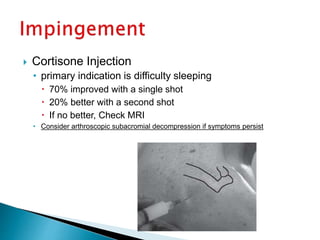
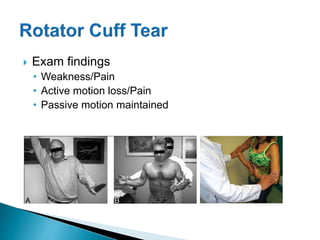
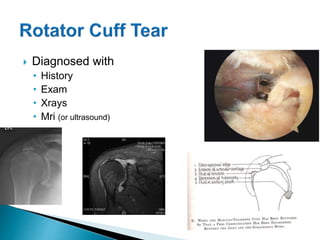
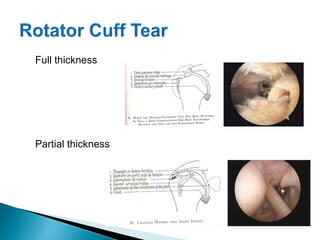
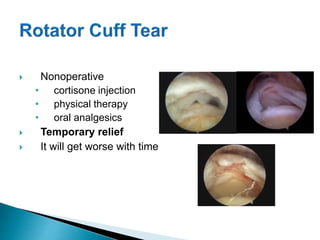
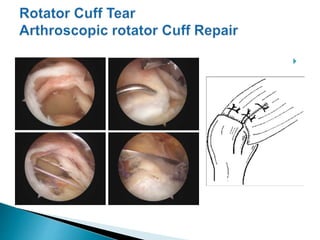
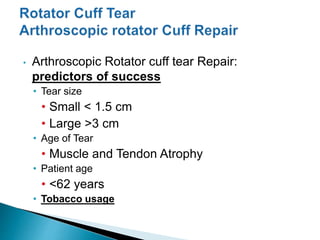
This document describes the anatomy and function of the rotator cuff muscles, as well as causes, diagnosis, and treatment of rotator cuff injuries. It notes that the rotator cuff is comprised of 4 muscles that stabilize the shoulder joint. Rotator cuff injuries can range from inflammation to complete tears and are usually caused by overuse, aging, or trauma. Treatment involves rest, anti-inflammatories, cortisone injections, and physical therapy, with surgery reserved for tears not improving otherwise.