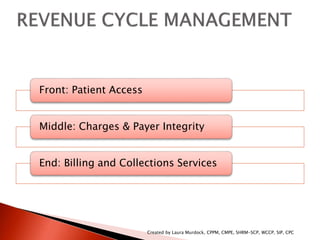
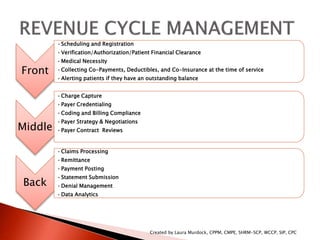
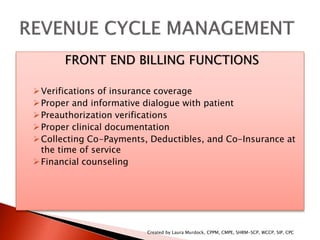
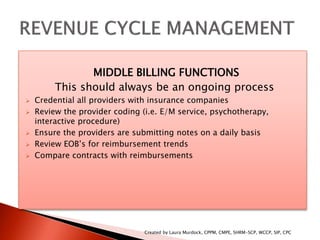
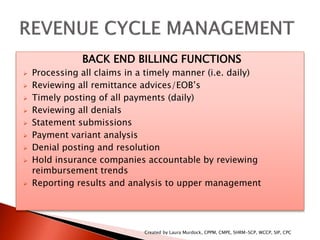
The document outlines the comprehensive revenue cycle management process, categorized into three phases: front-end (patient access), middle (charges and payer integrity), and back-end (billing and collections). Each phase includes detailed functions such as scheduling, insurance verification, charge capture, claims processing, and denial management, emphasizing the need for ongoing processes and timely actions. It also highlights the importance of compliance, technology leverage, and performance management in optimizing revenue cycle operations.