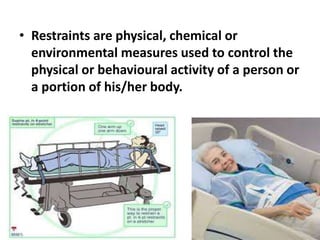
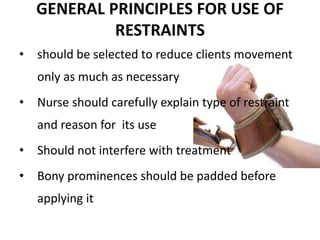
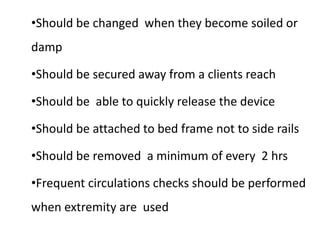
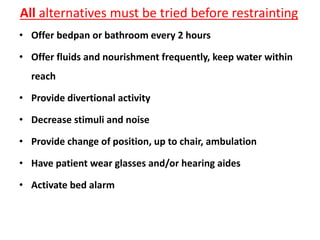
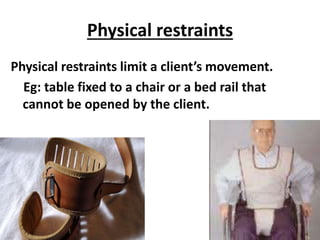
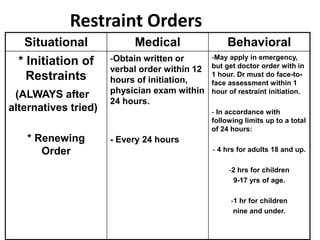
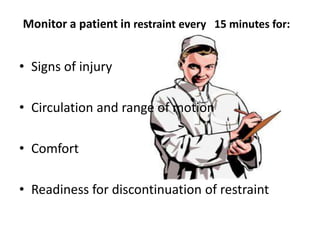
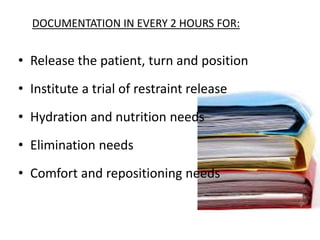
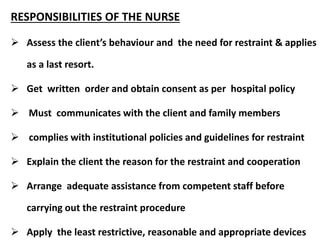
This document provides information on the nurse's role and responsibilities regarding the use of restraints. It defines restraints and outlines general principles, indications, types, risks, and guidelines for their use. The nurse's role includes obtaining a doctor's order, monitoring the restrained patient every 15 minutes, documenting checks every 2 hours, and considering the earliest removal of restraints. Alternatives to restraints should always be tried first to reduce risk of harm.