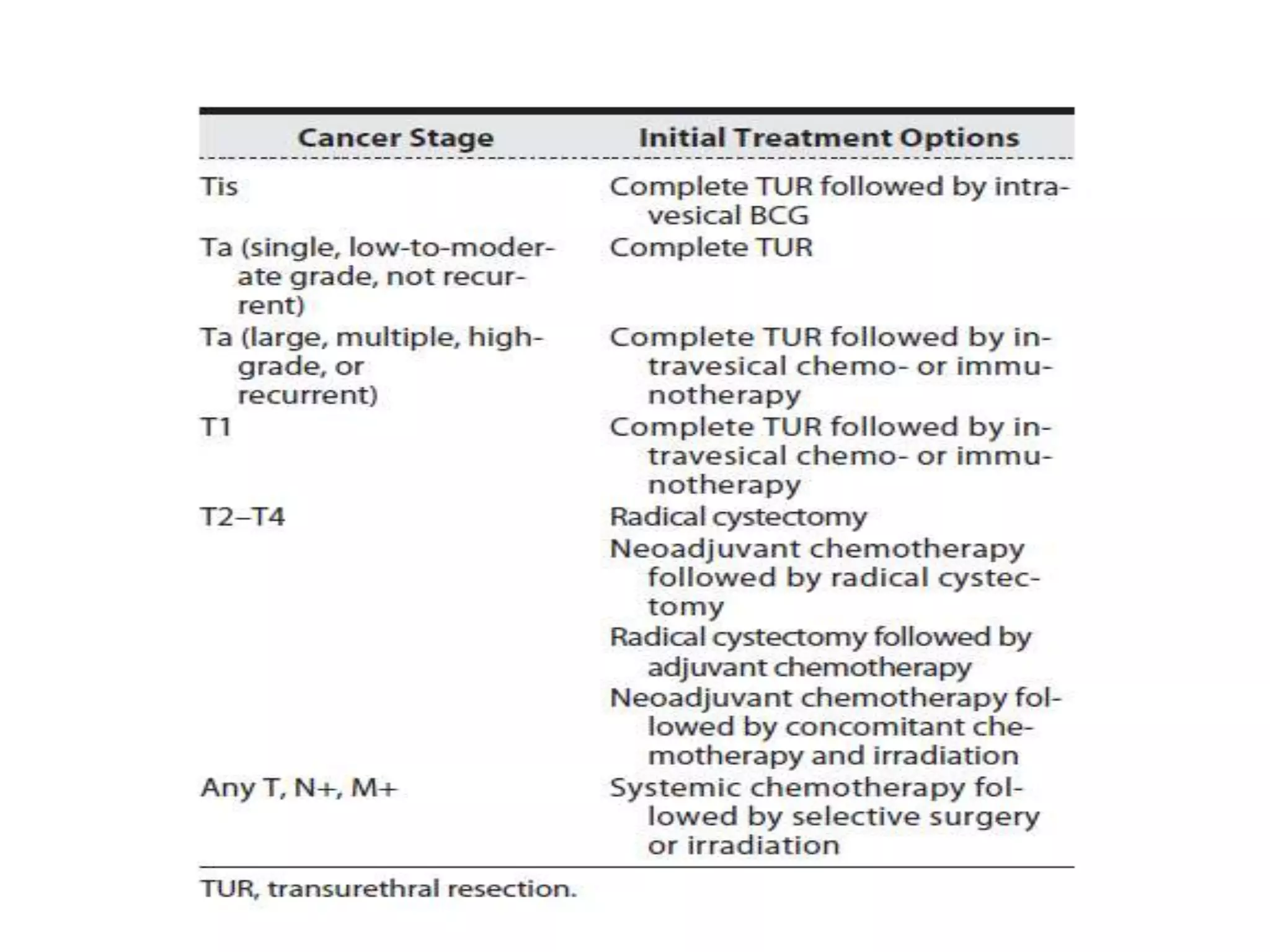
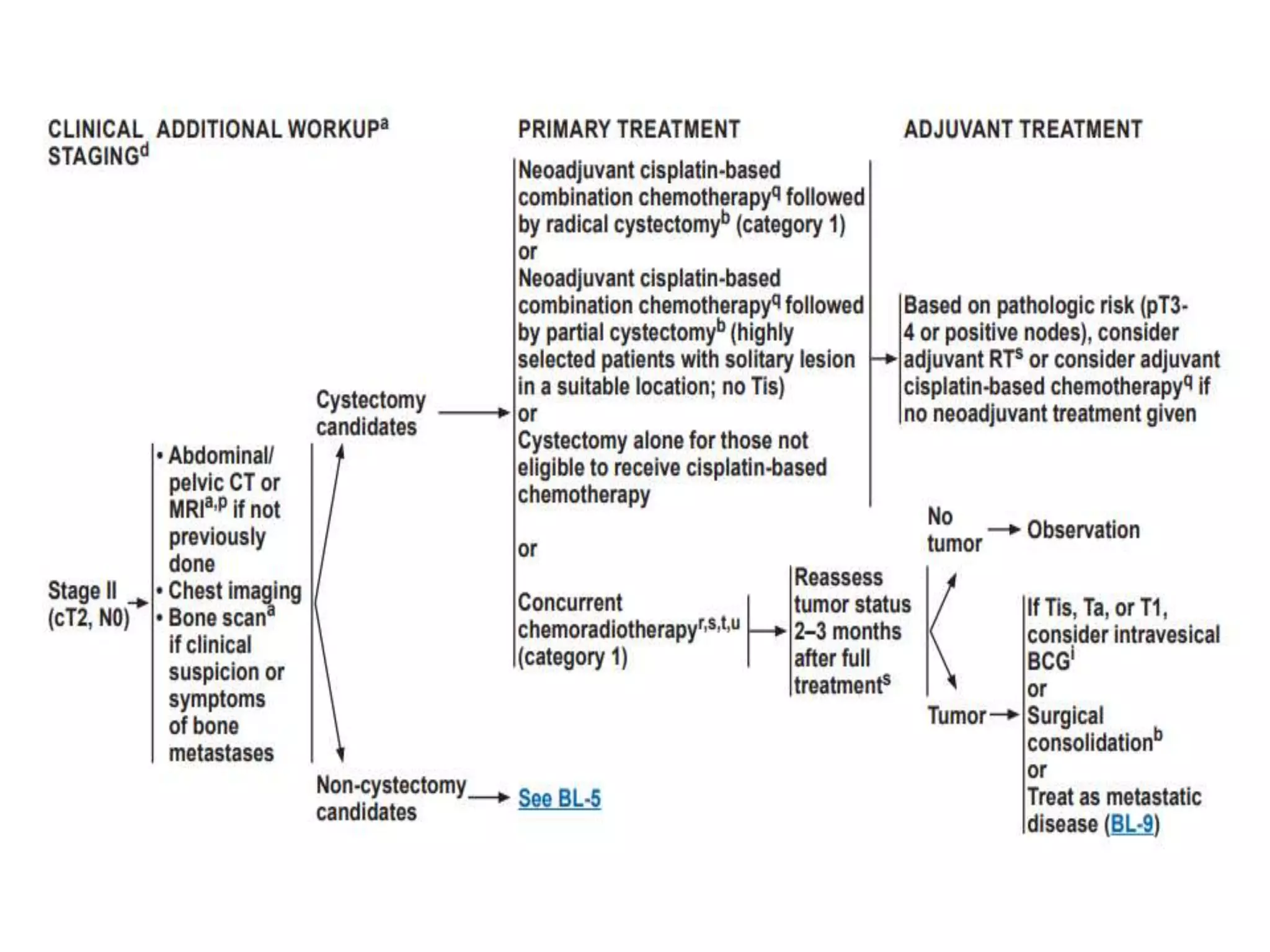
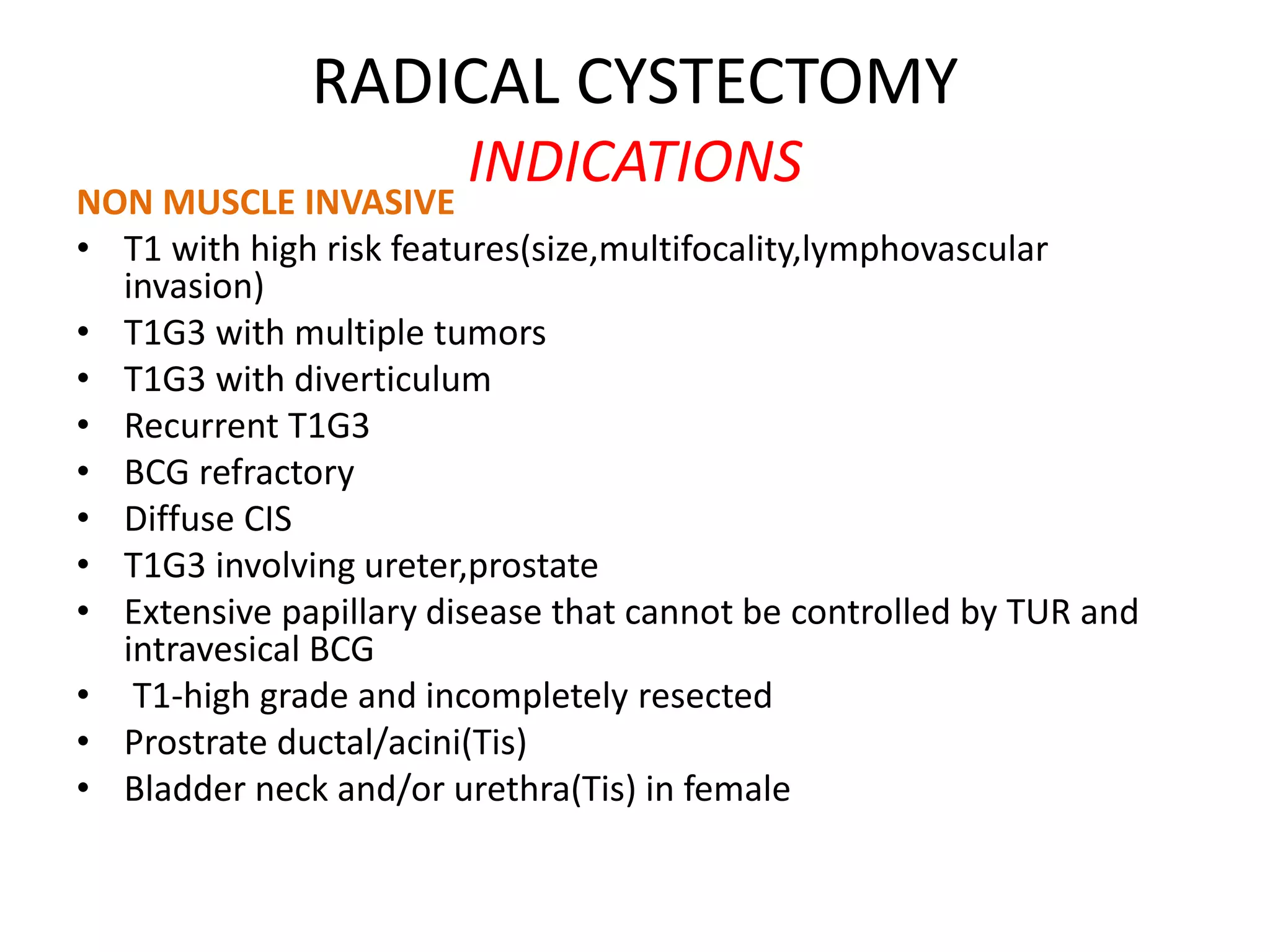
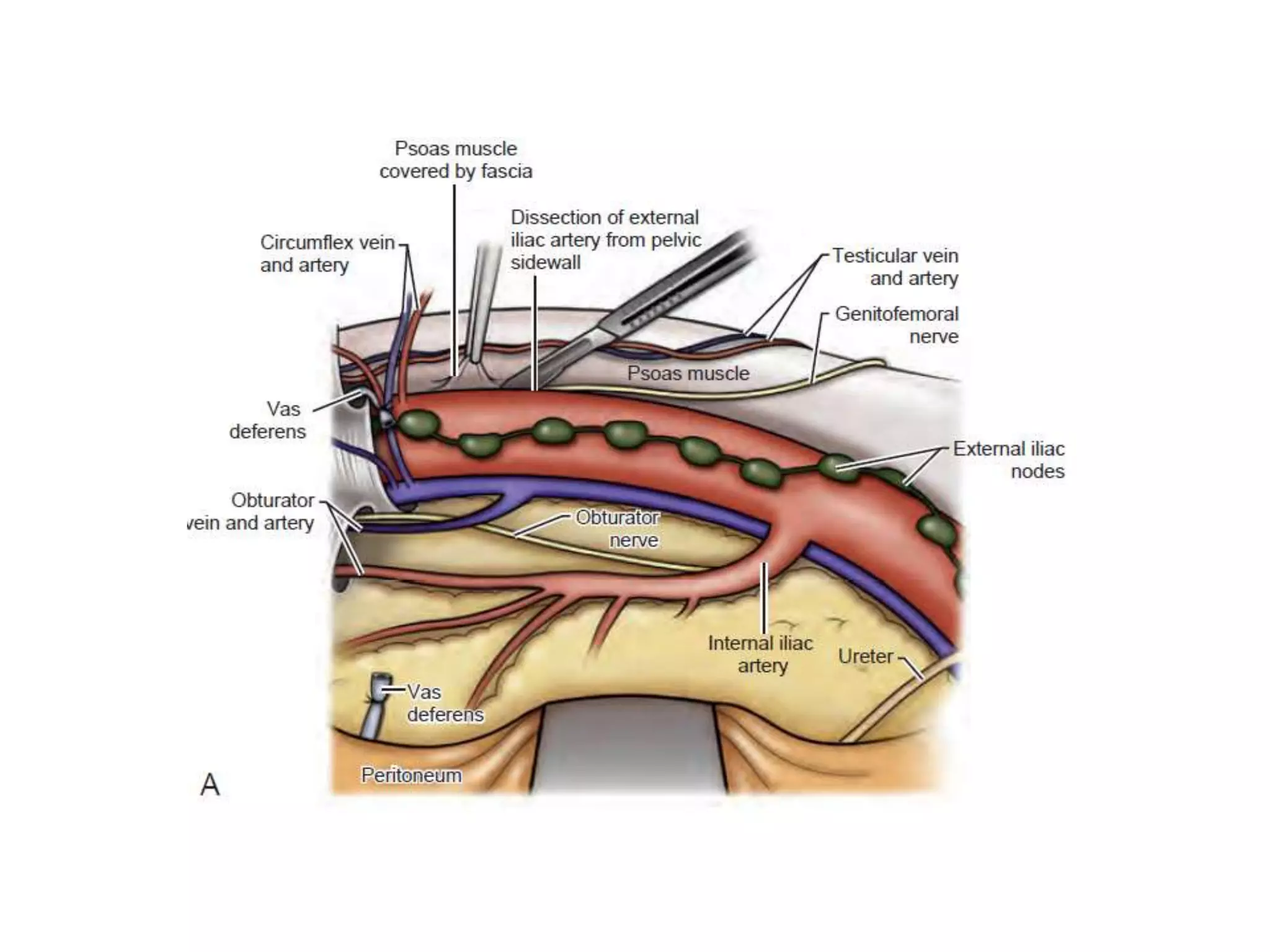
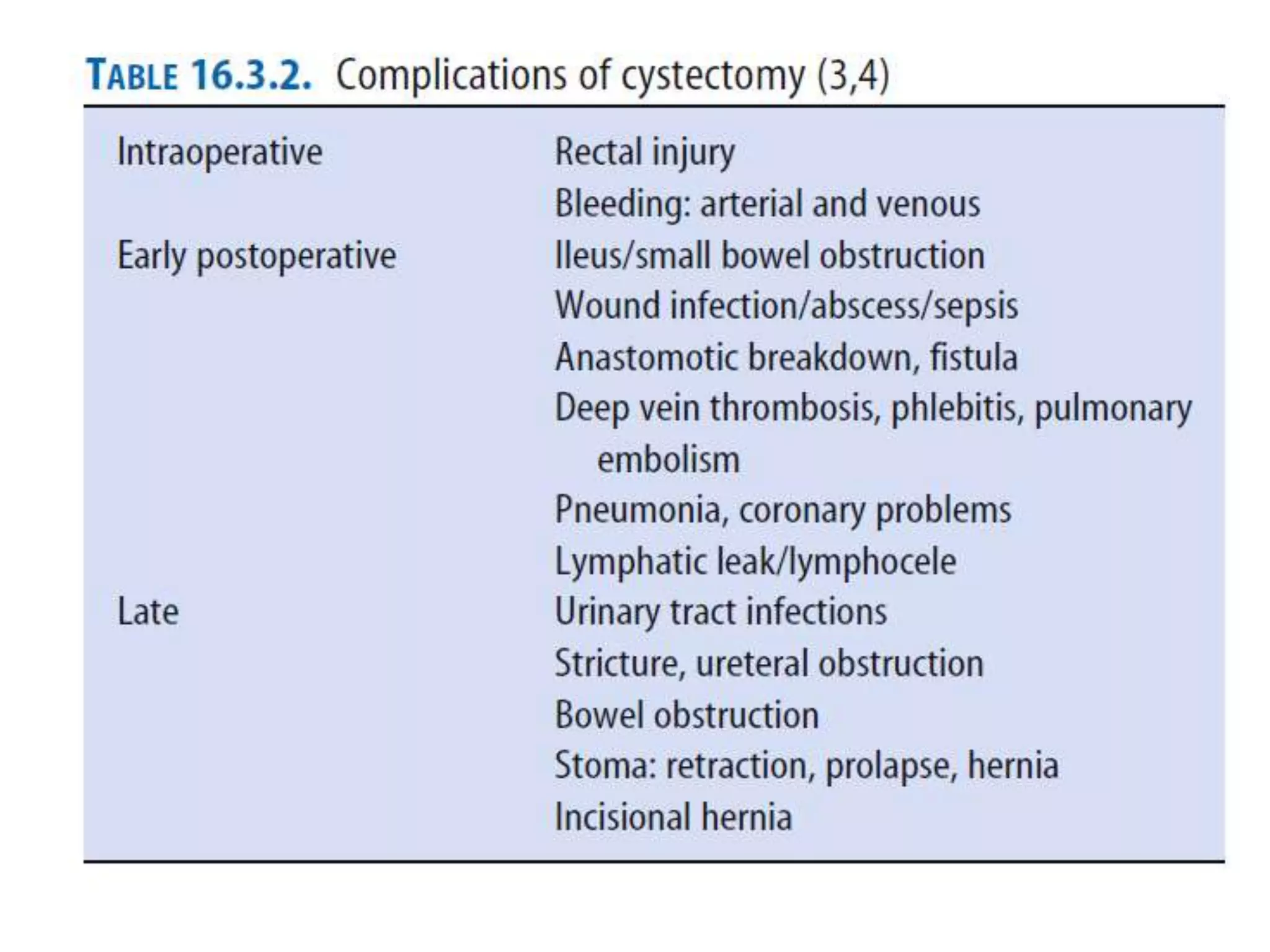
1) Radical cystectomy involves removal of the bladder and adjacent organs for muscle-invasive or high-risk non-muscle invasive bladder cancer.
2) Neoadjuvant chemotherapy prior to surgery offers benefits like improved survival and early control of micrometastases for muscle-invasive tumors.
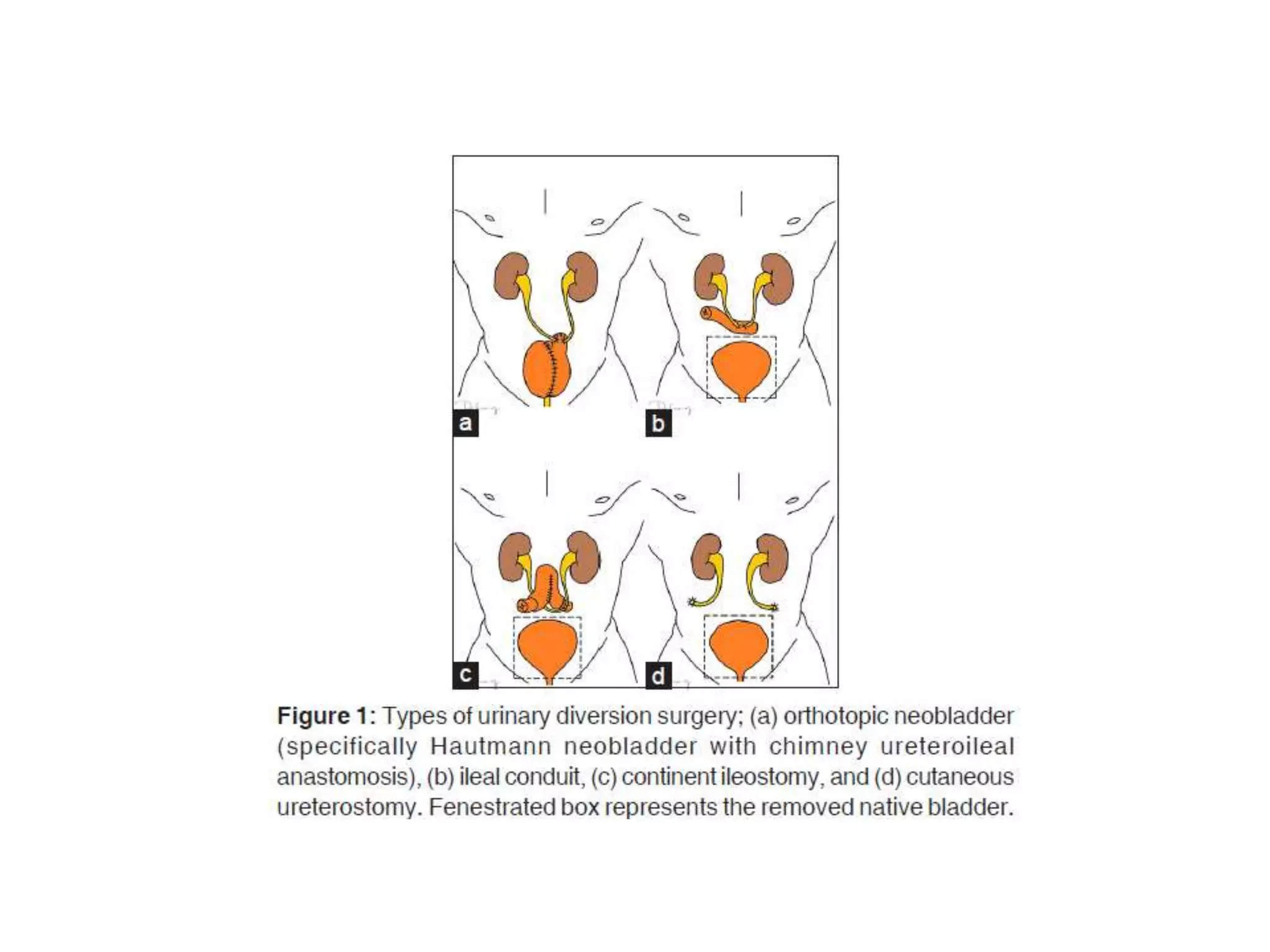
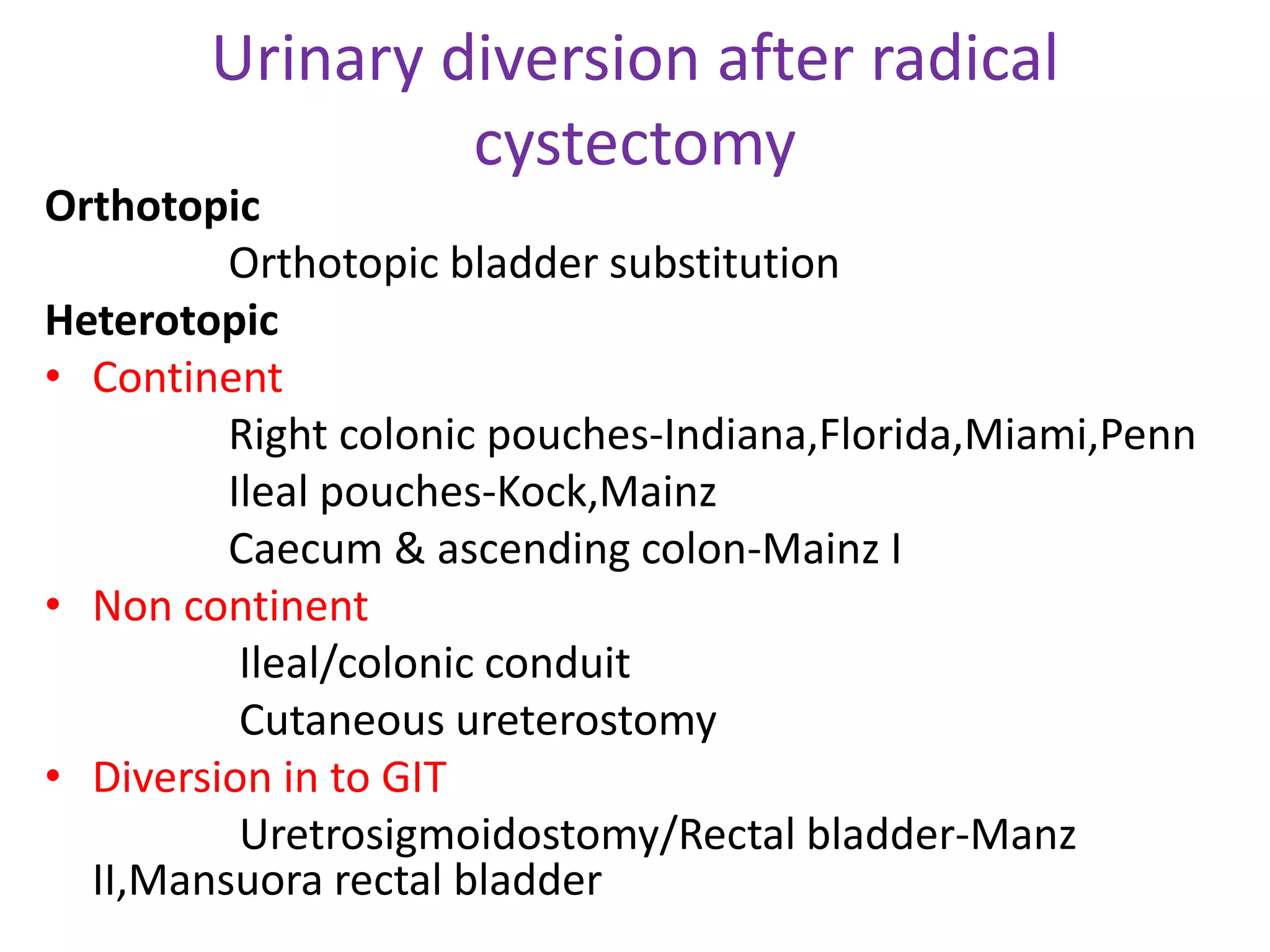
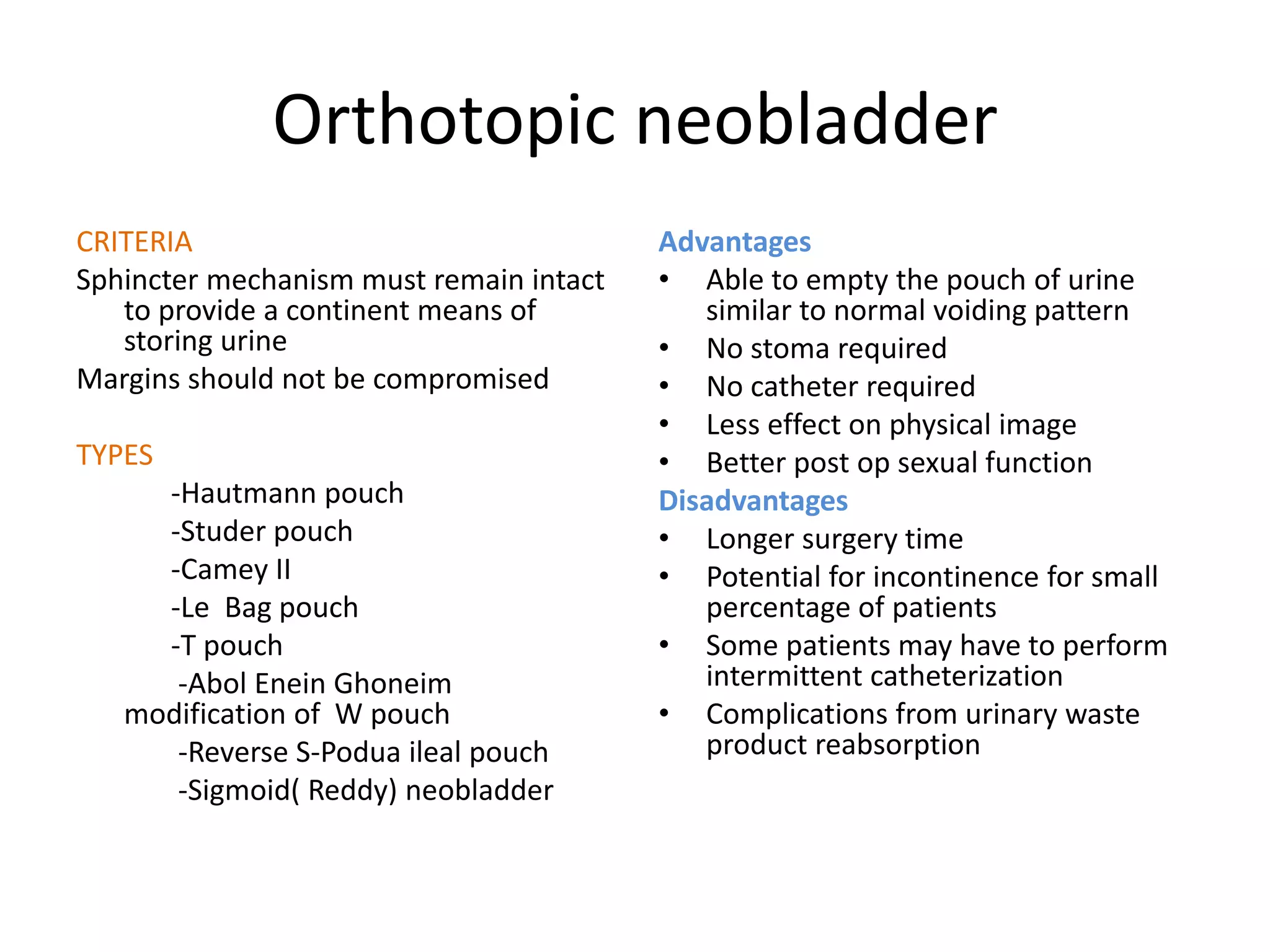
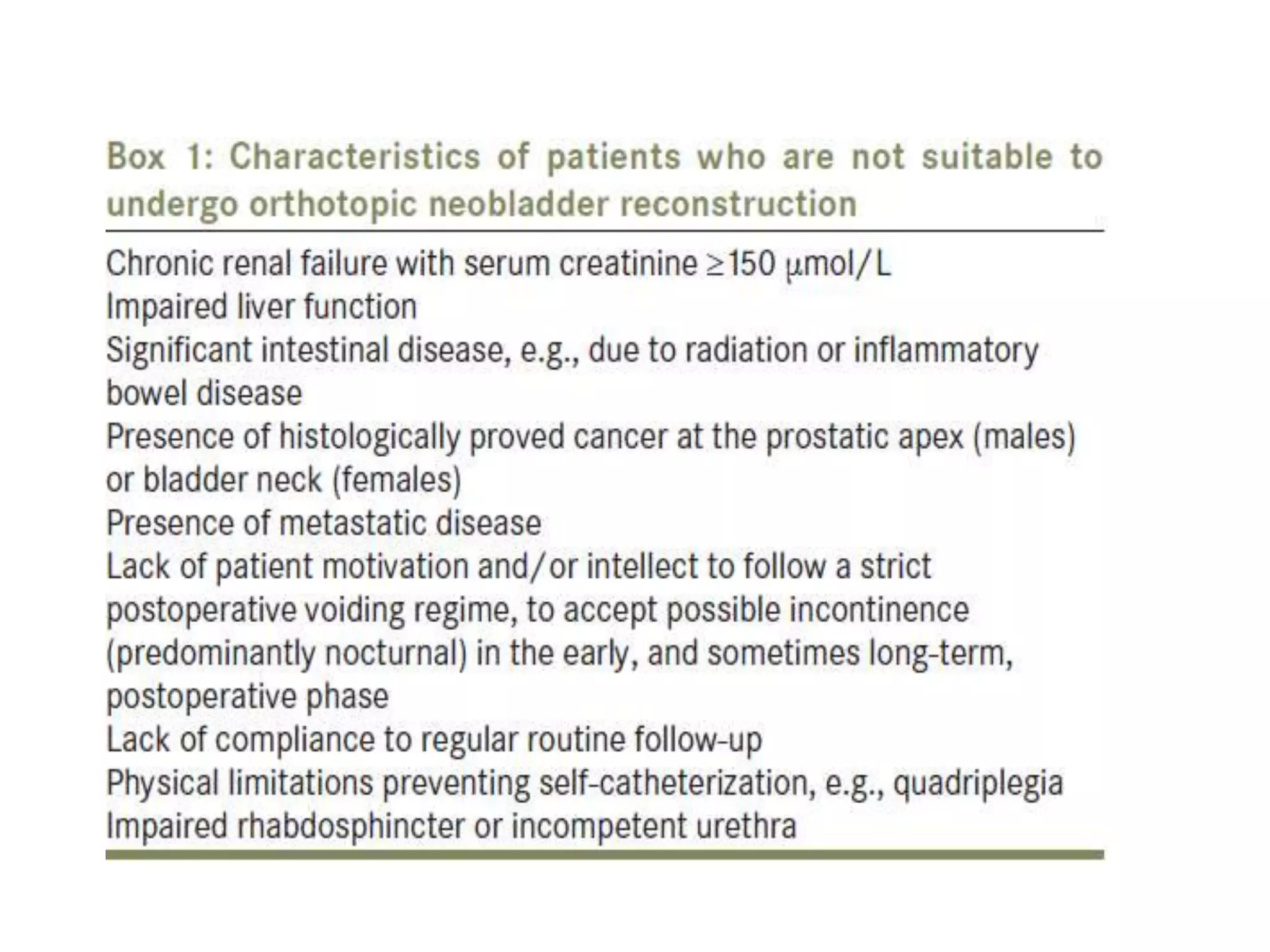
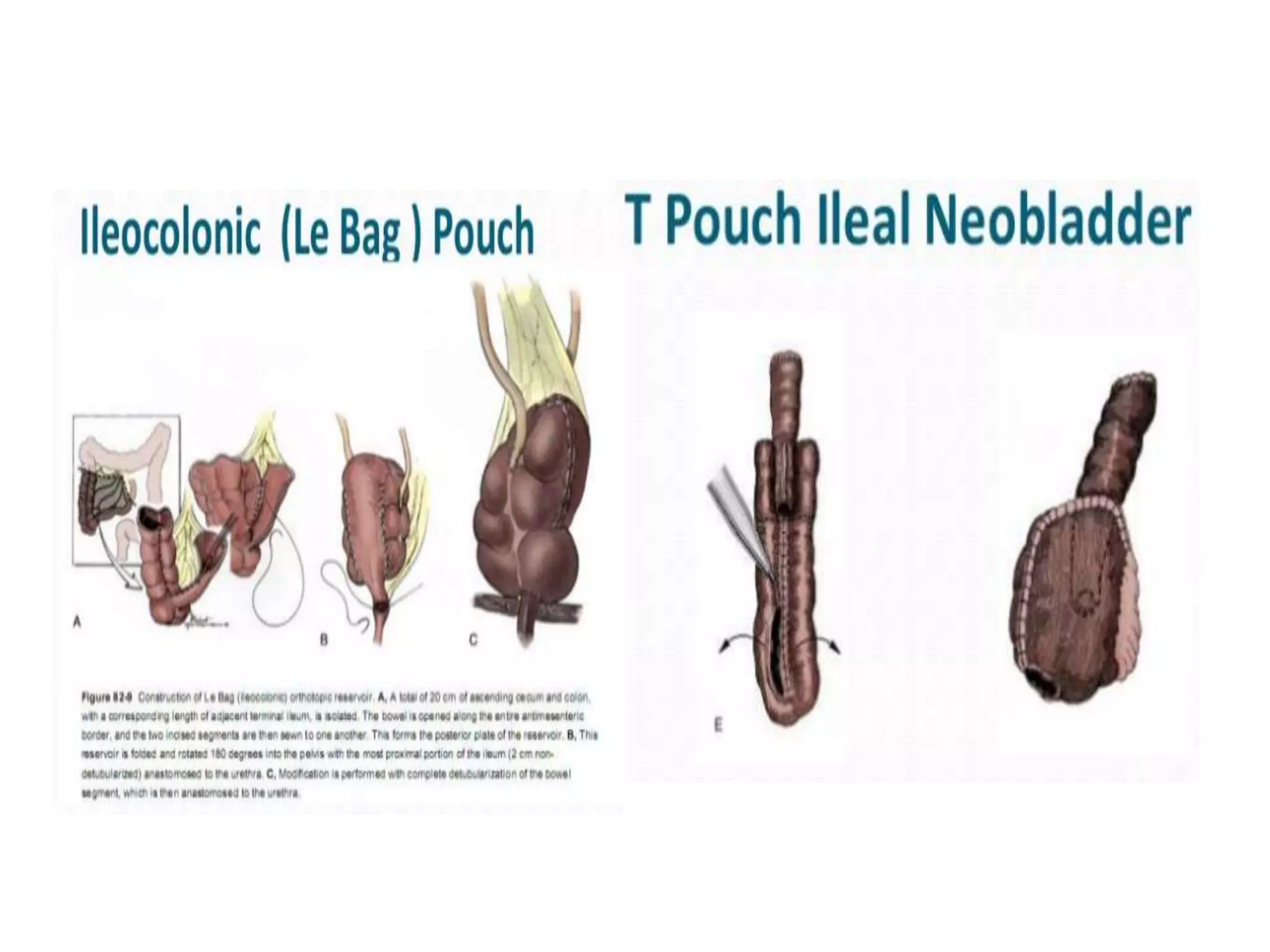
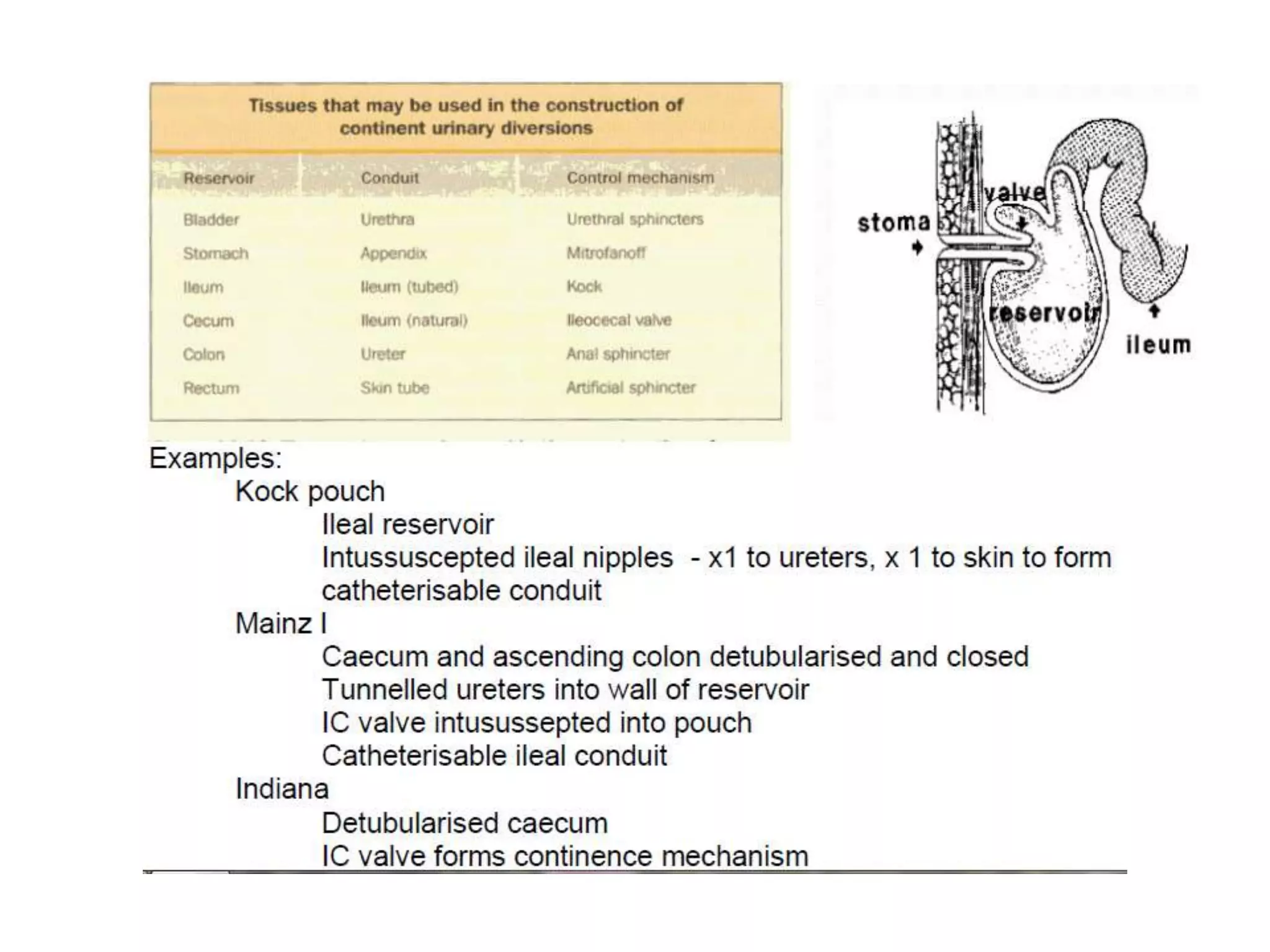
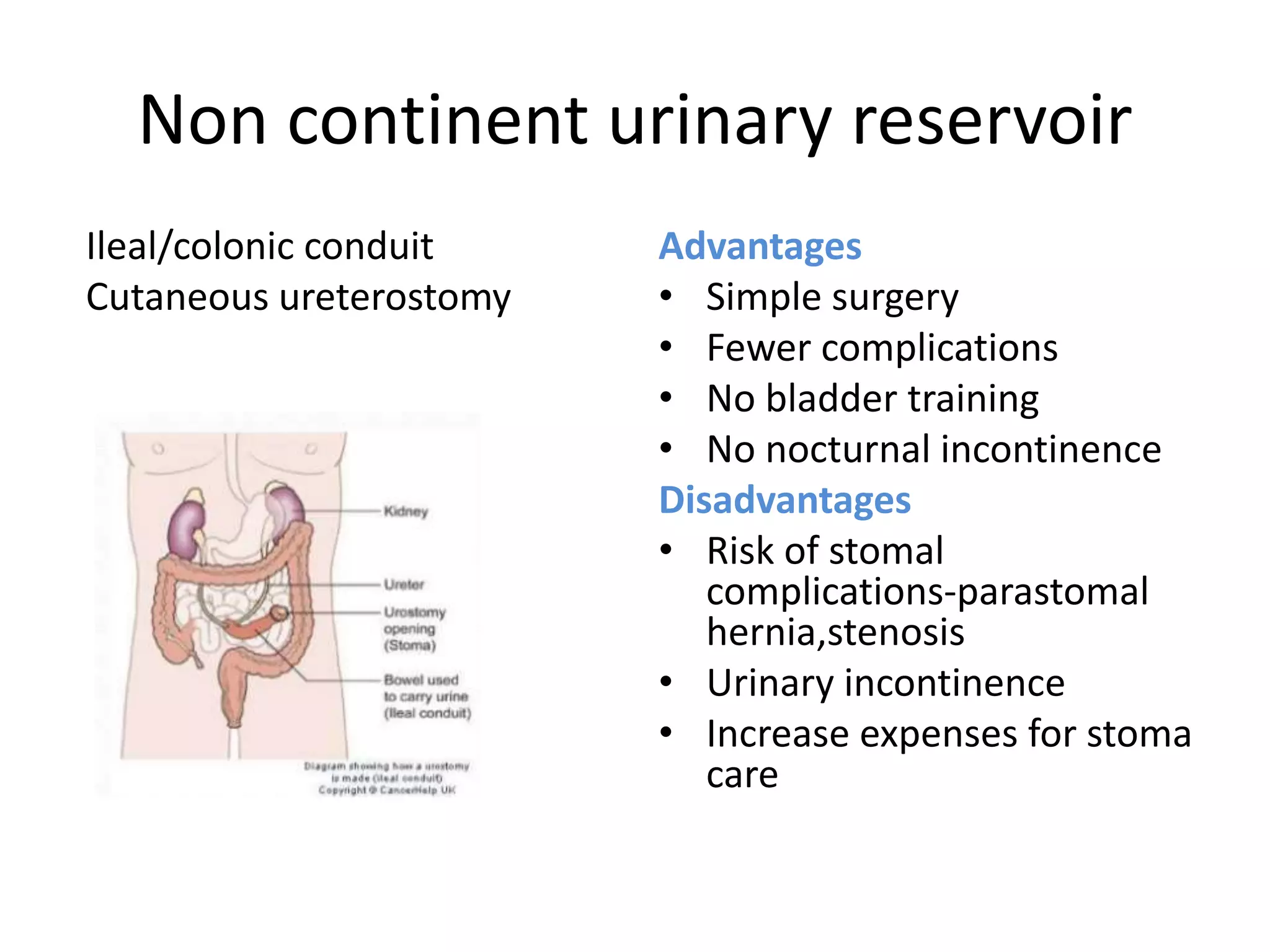
3) Urinary diversion options after cystectomy include orthotopic neobladder reconstruction to allow near-normal voiding or continent reservoirs requiring clean intermittent catheterization, or non-continent options like ileal conduit that require a stoma.