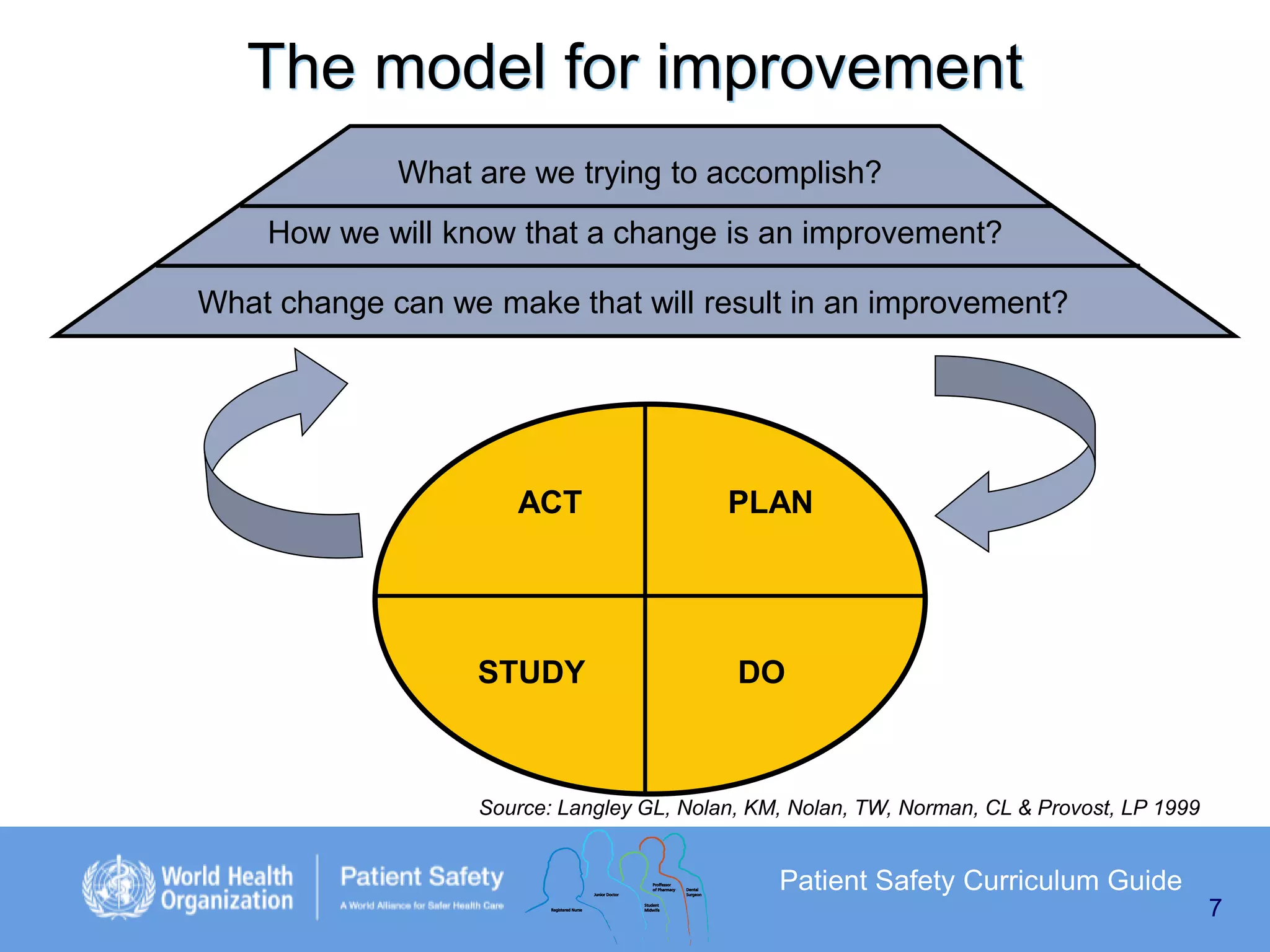
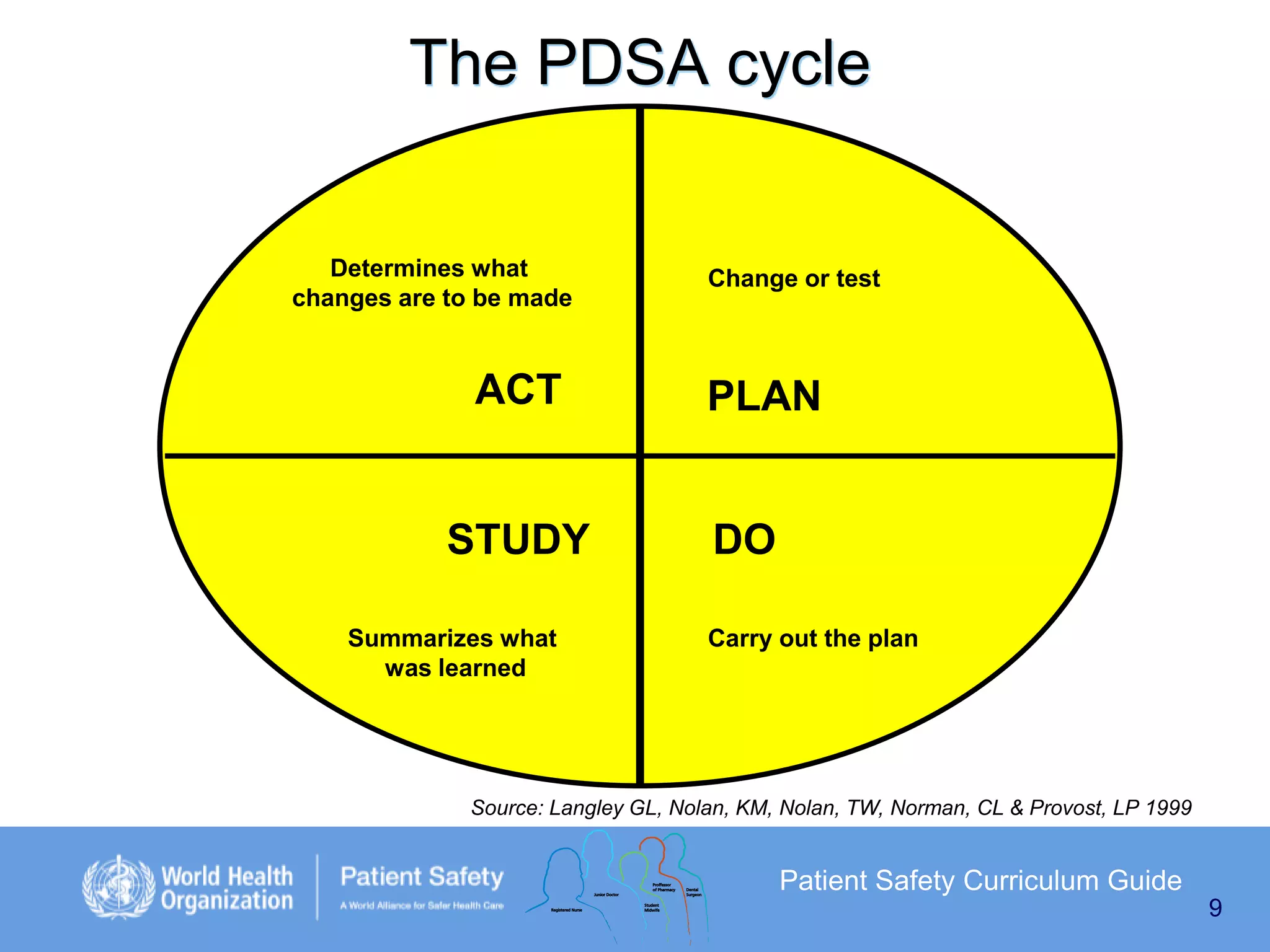
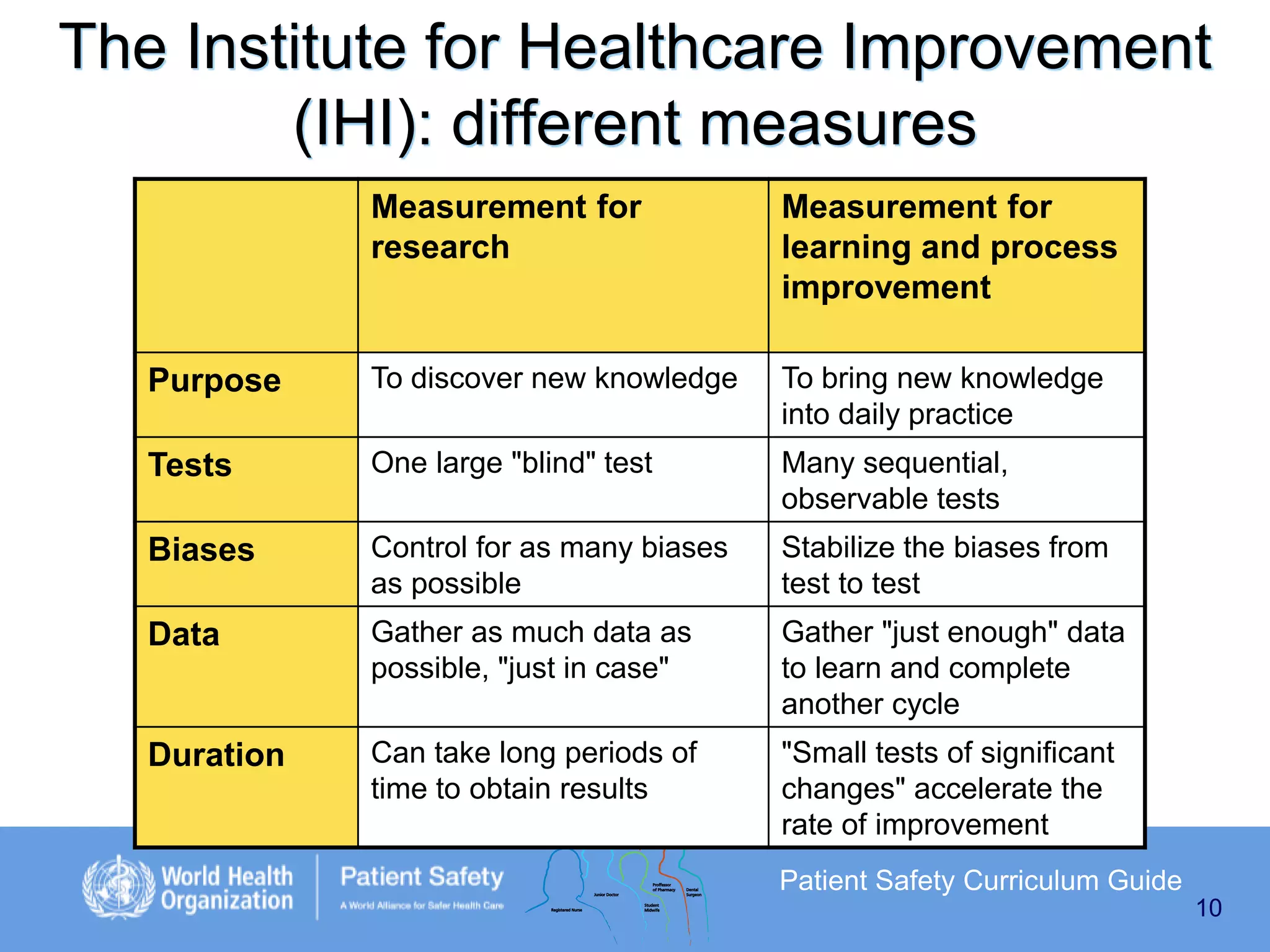
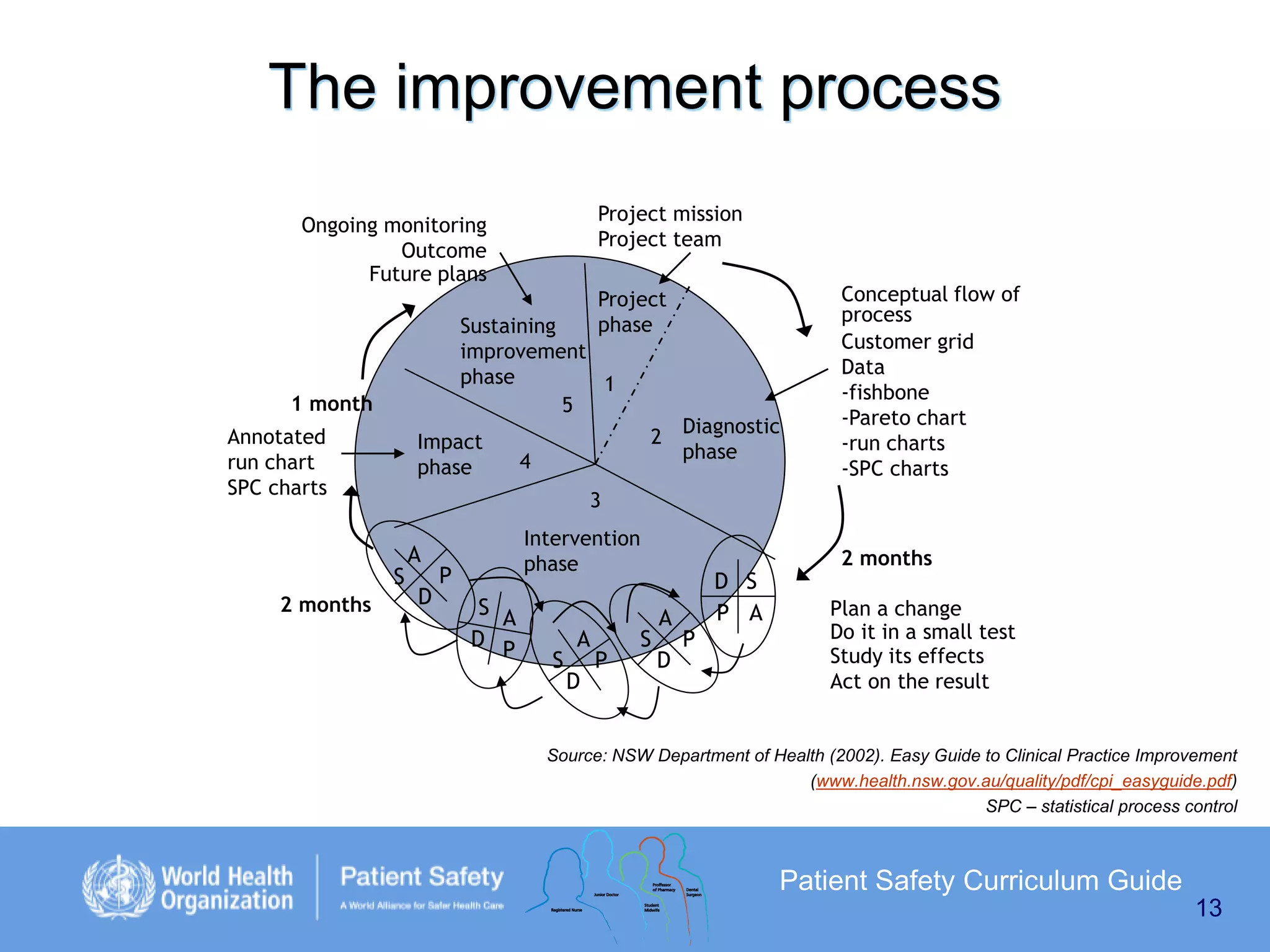
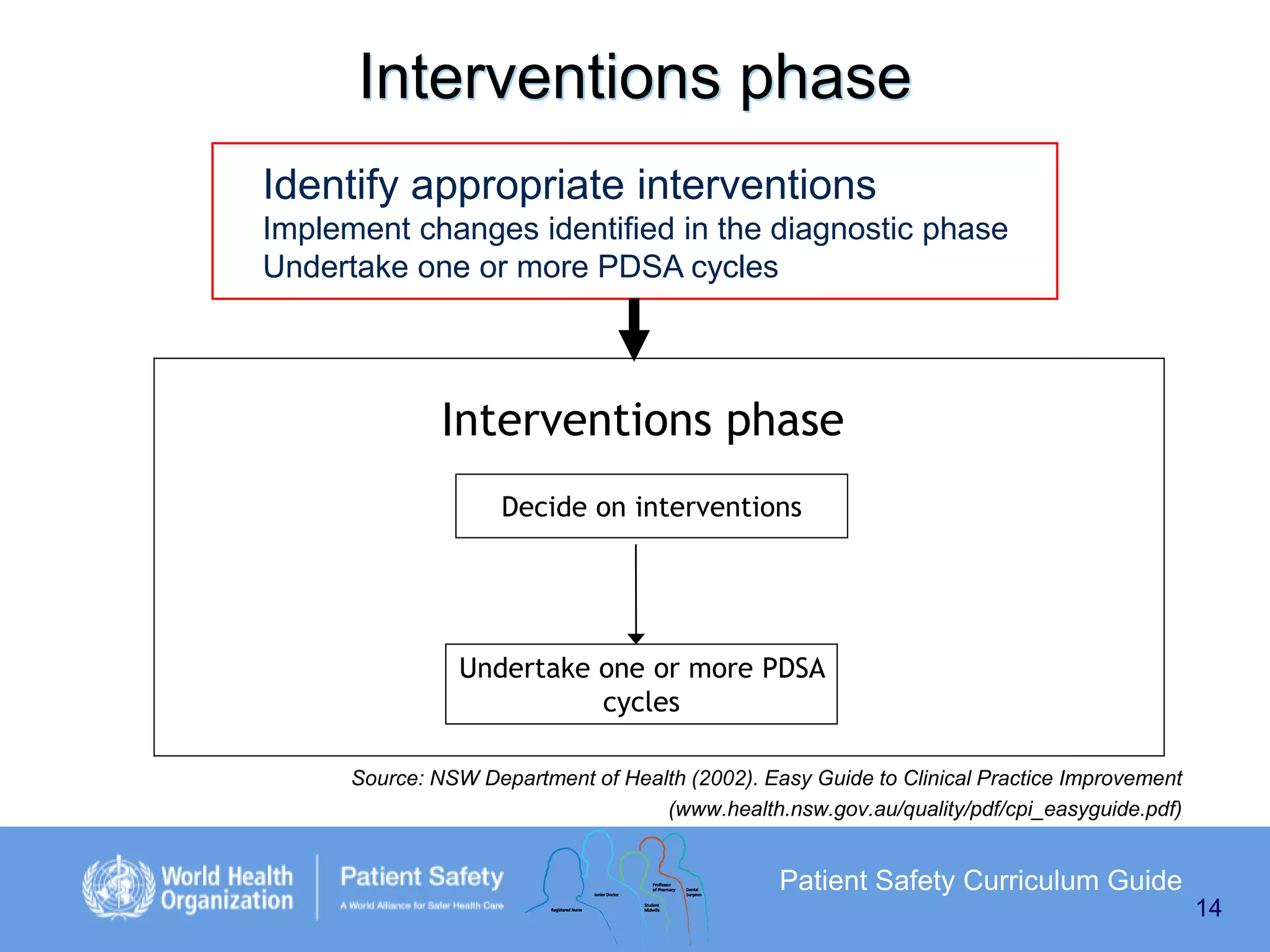
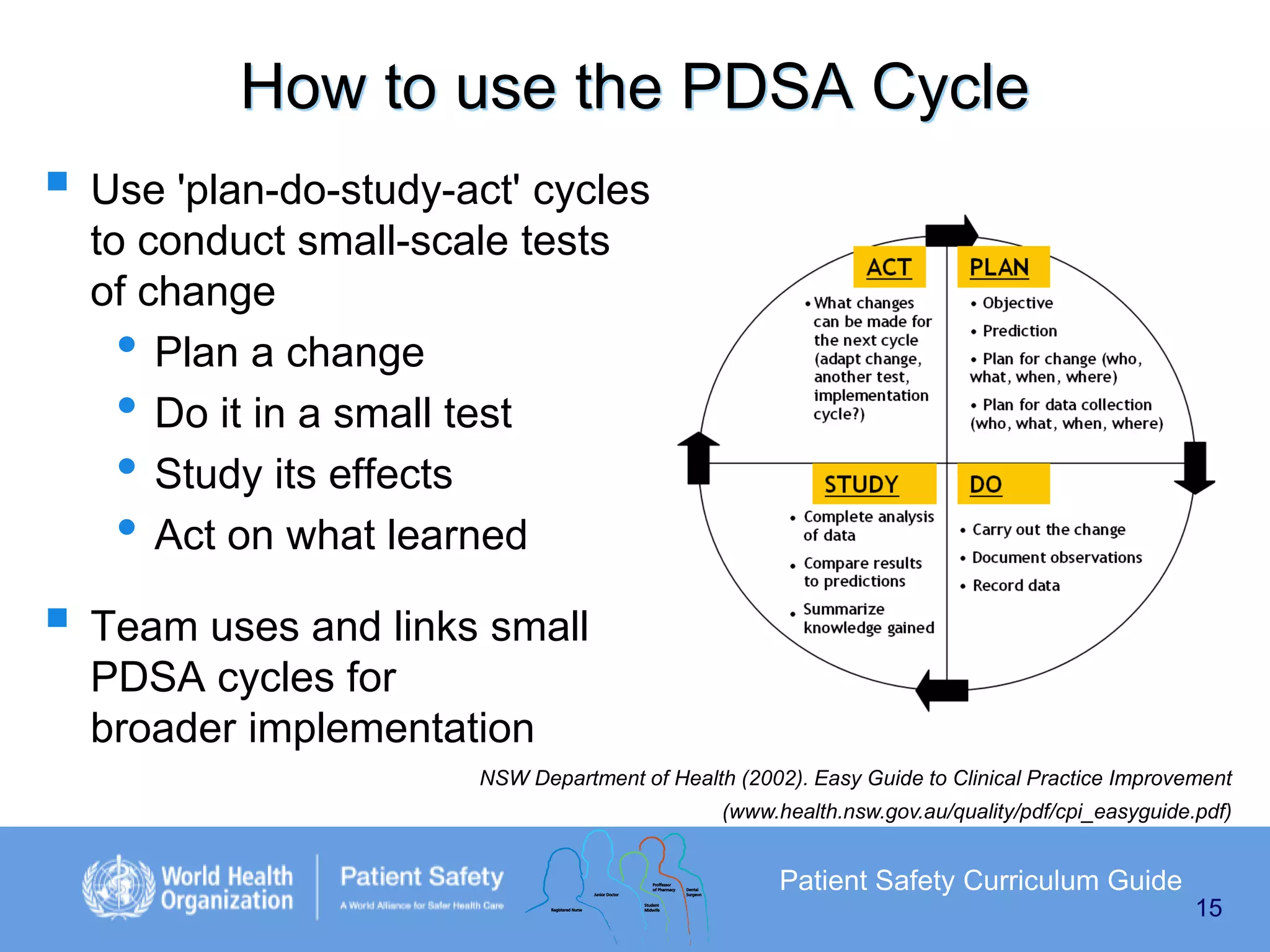
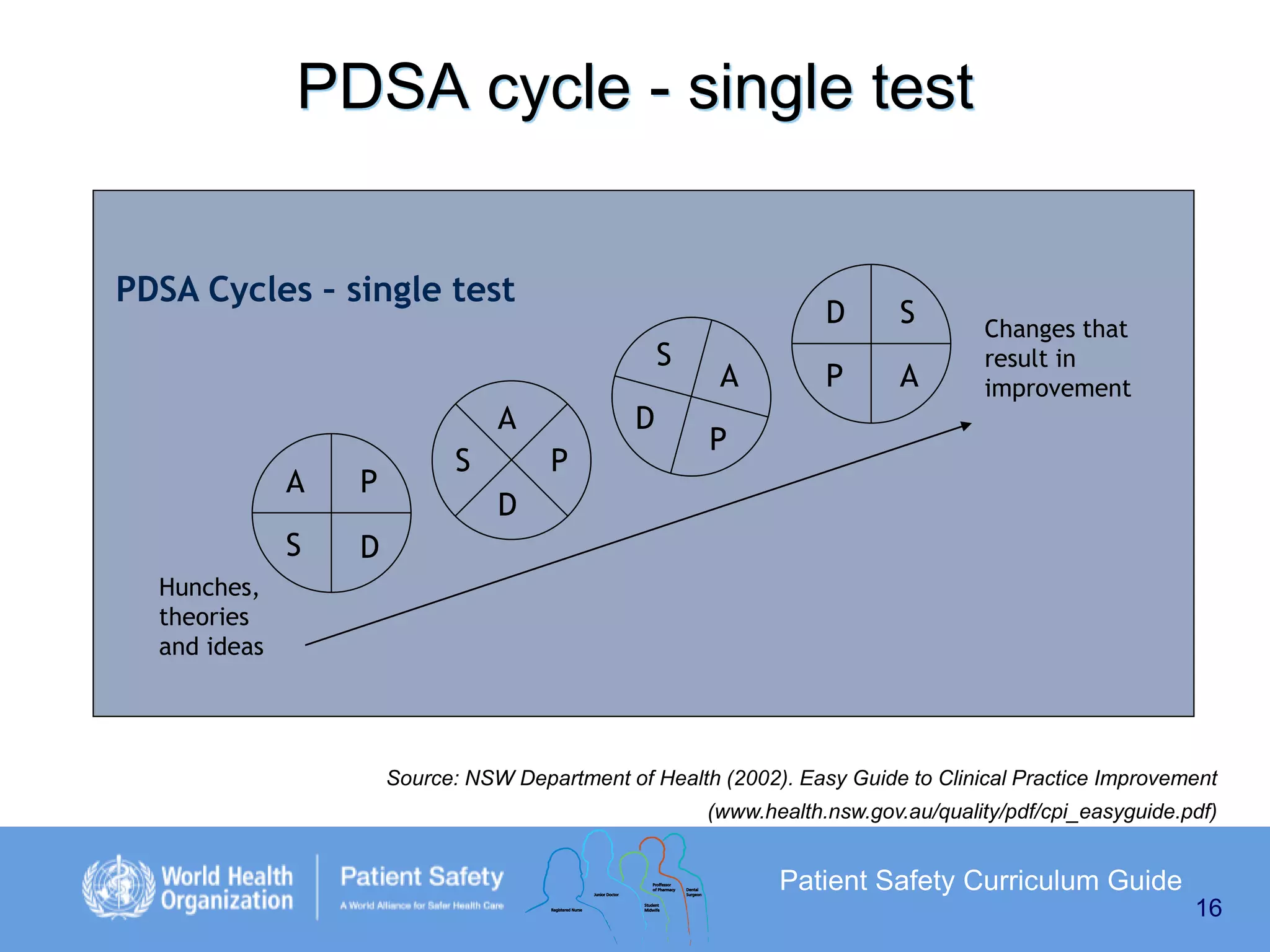
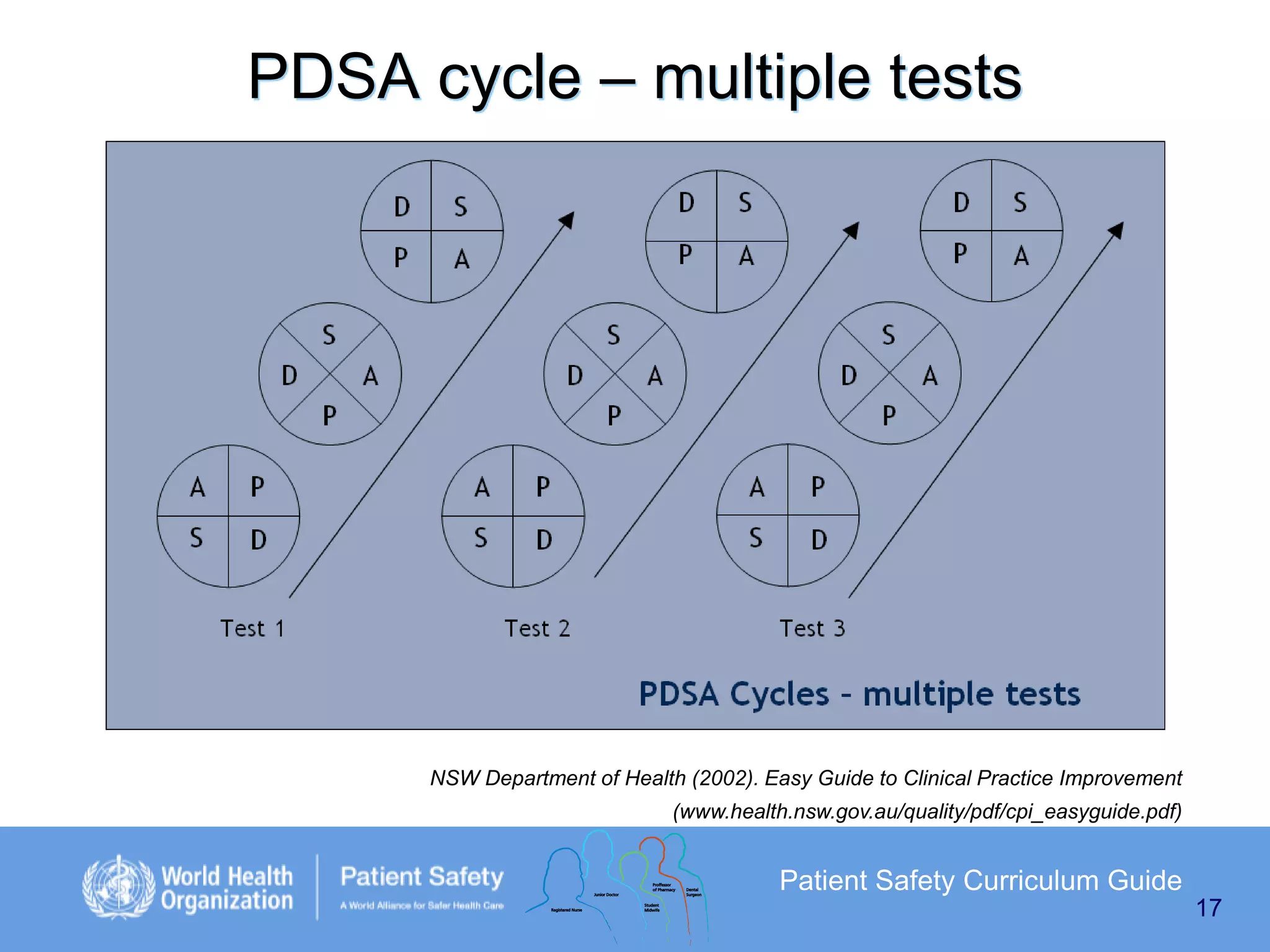
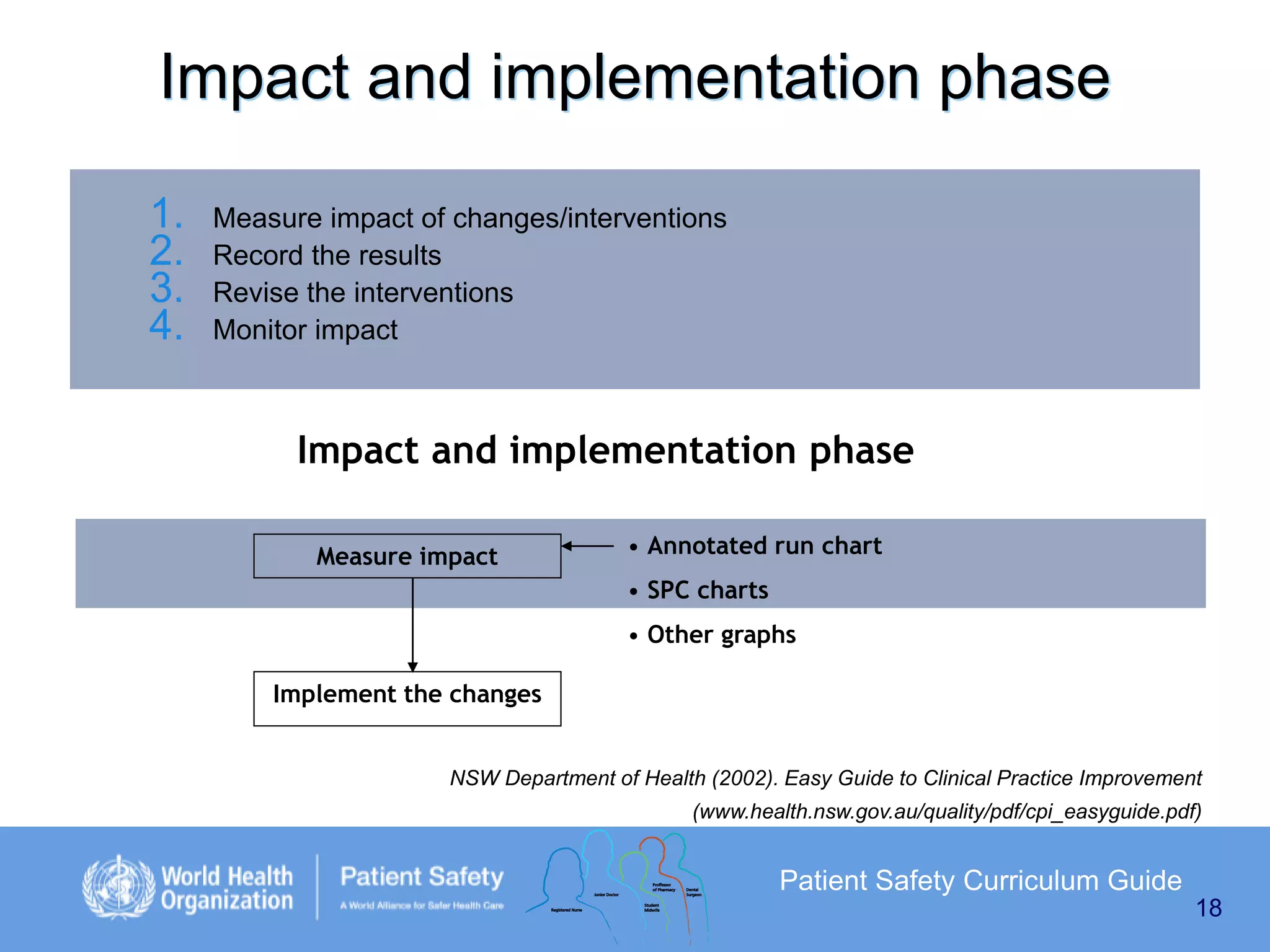
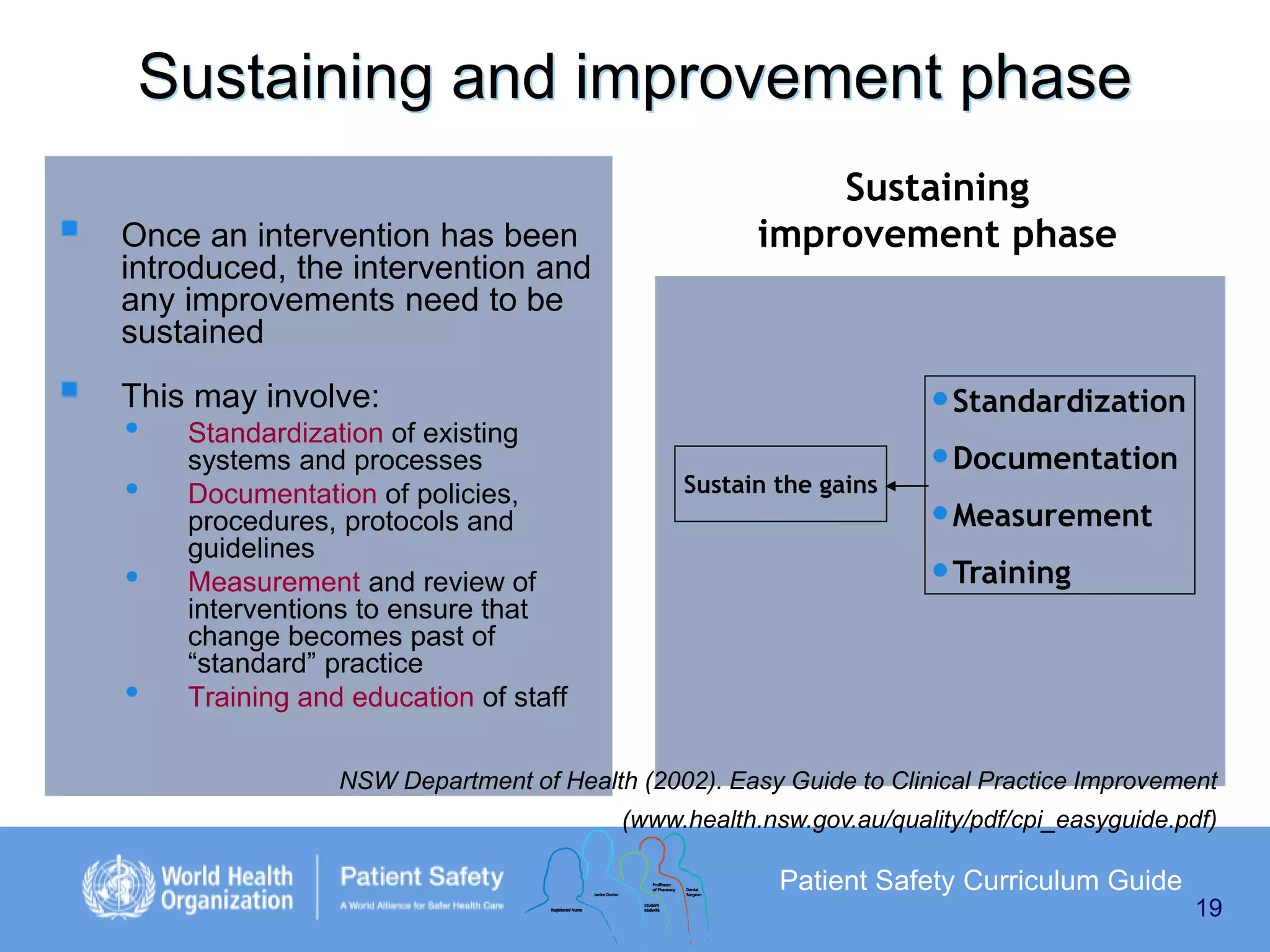
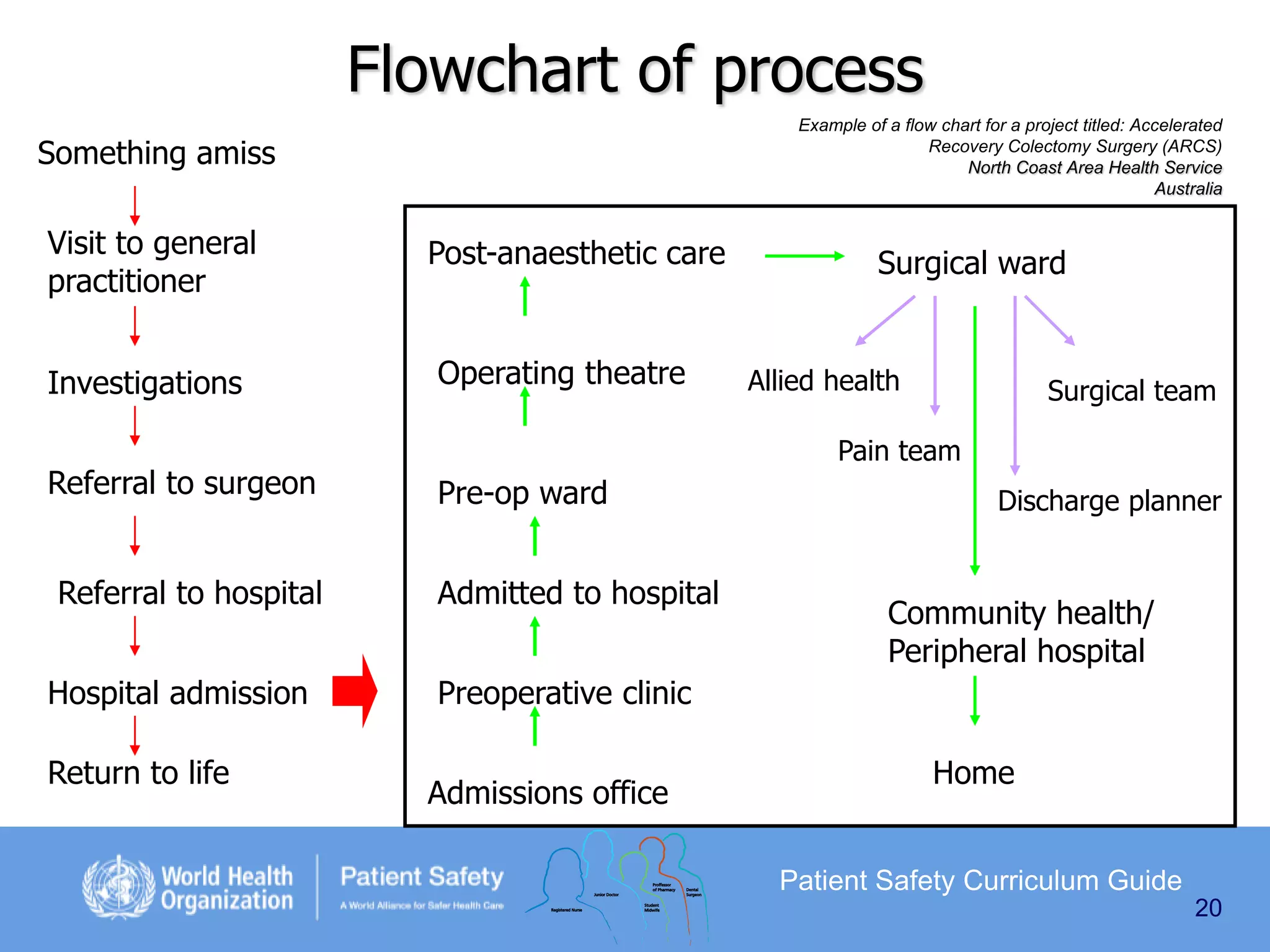
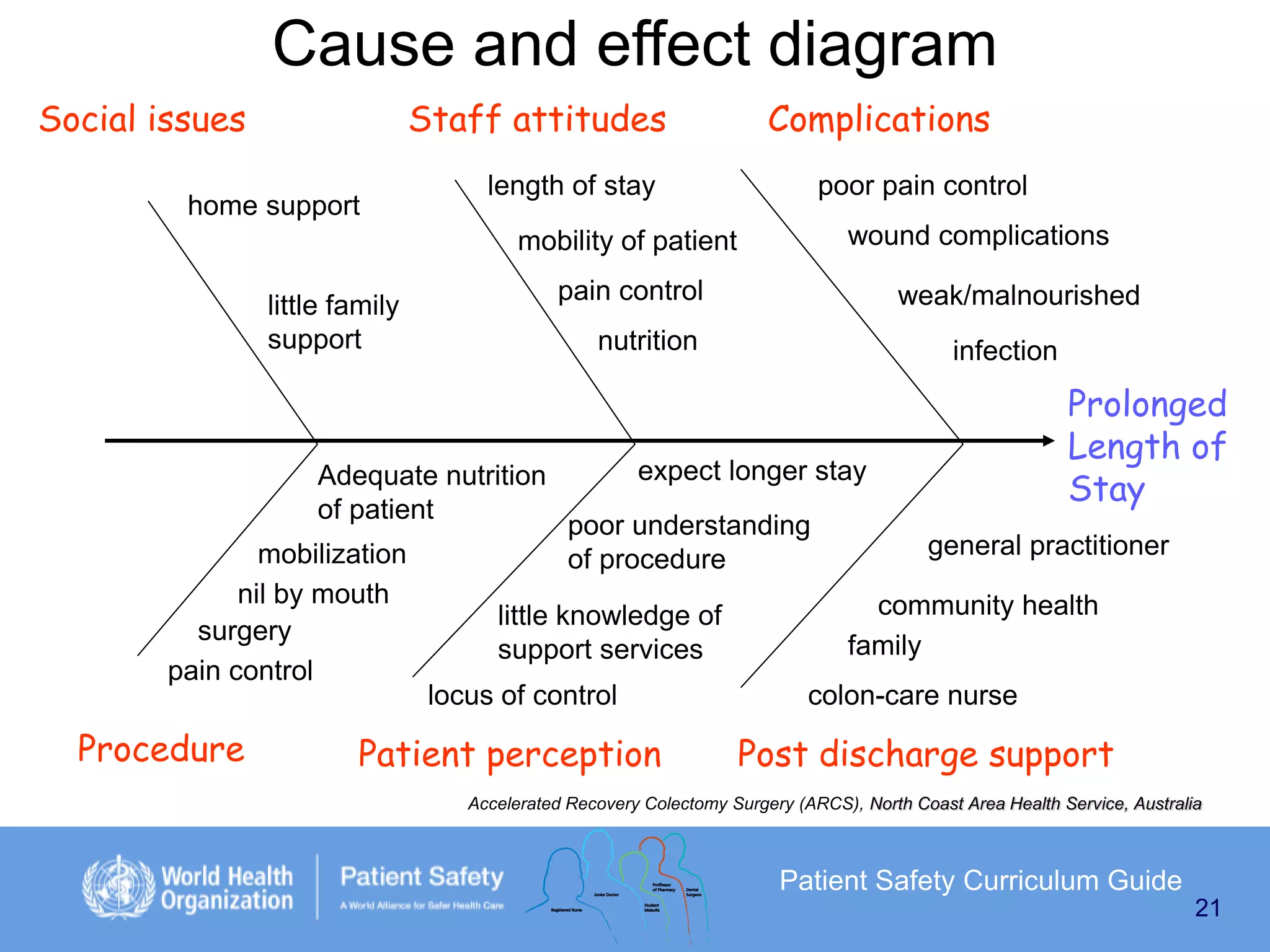
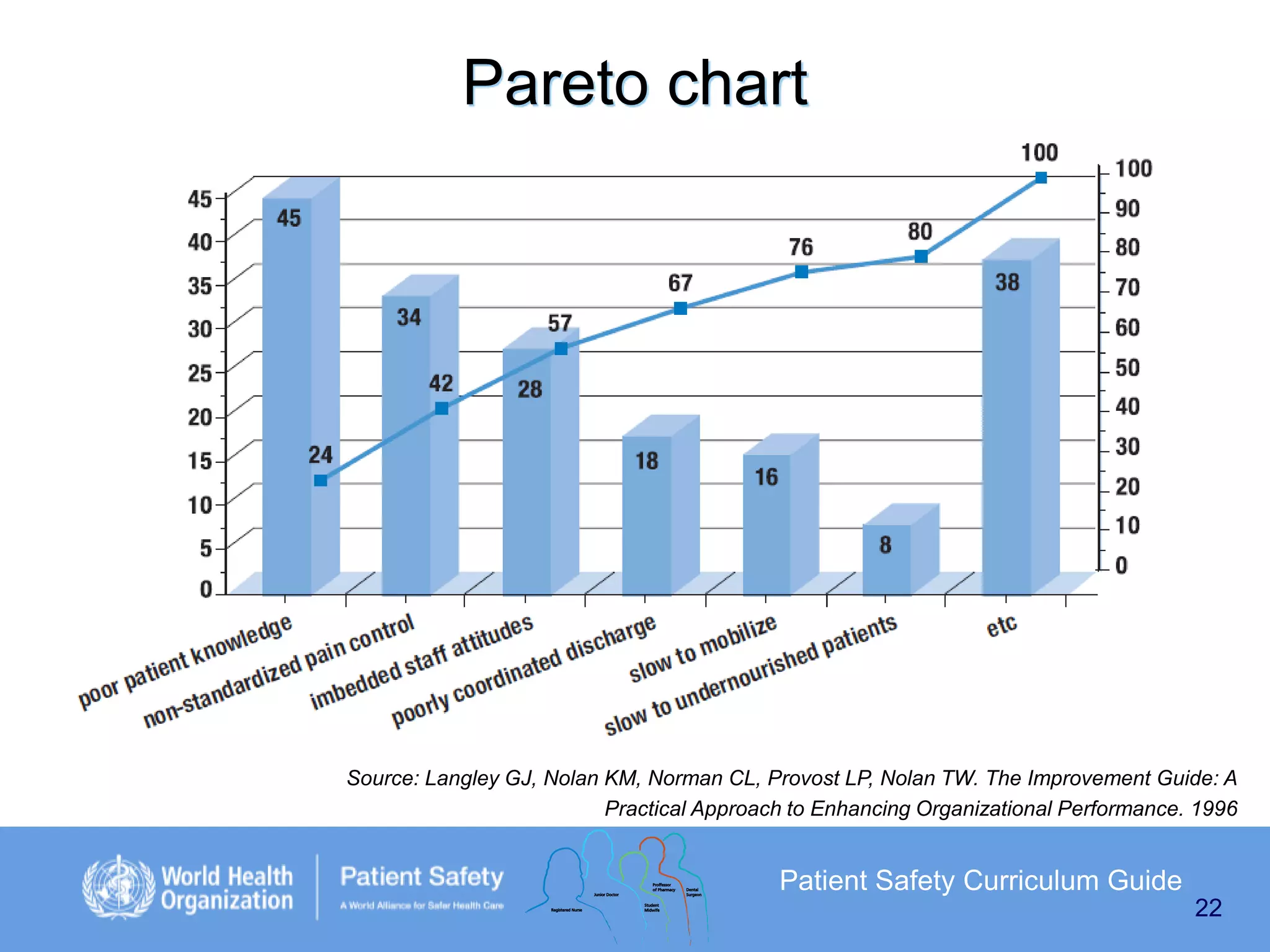
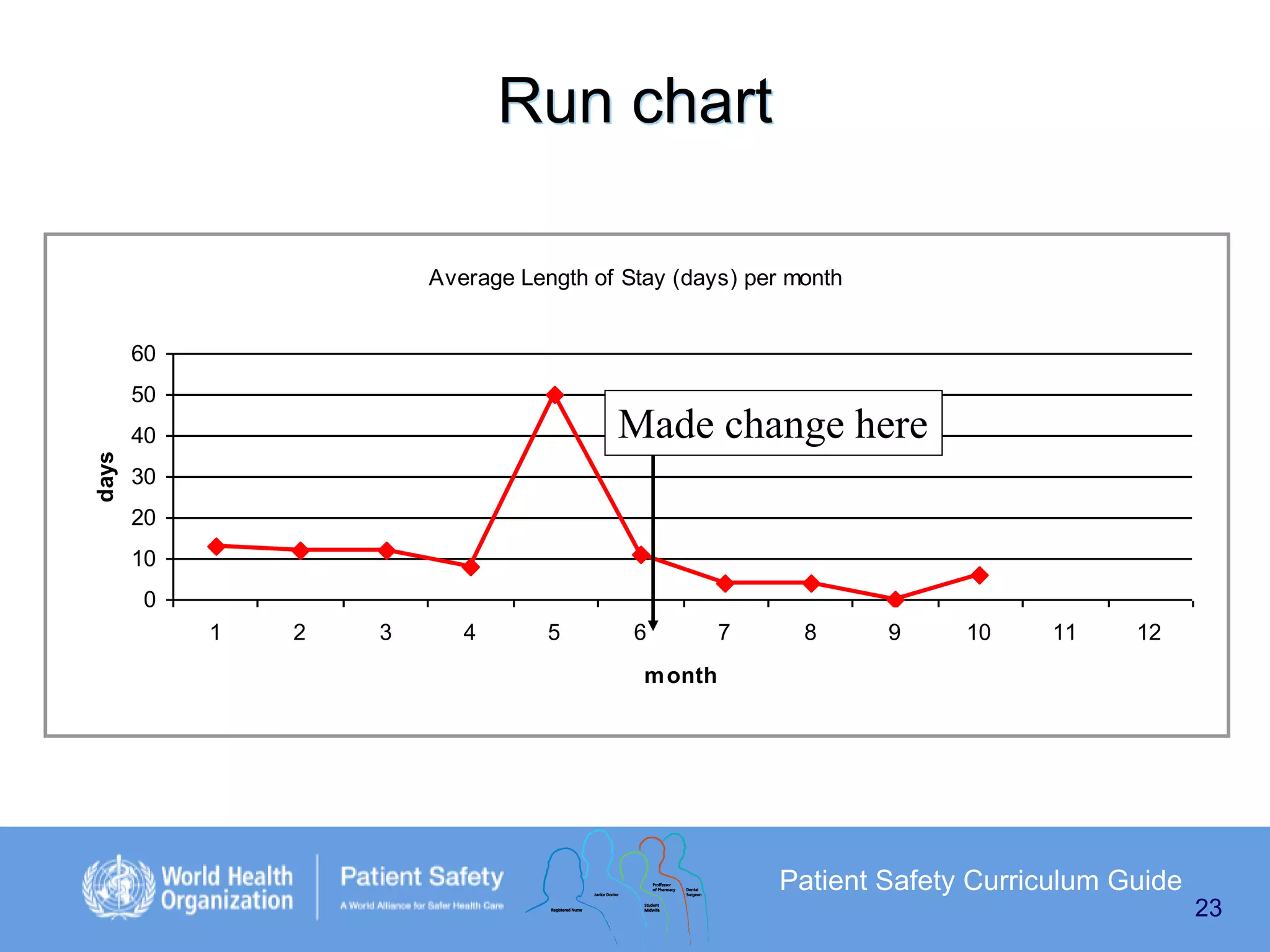
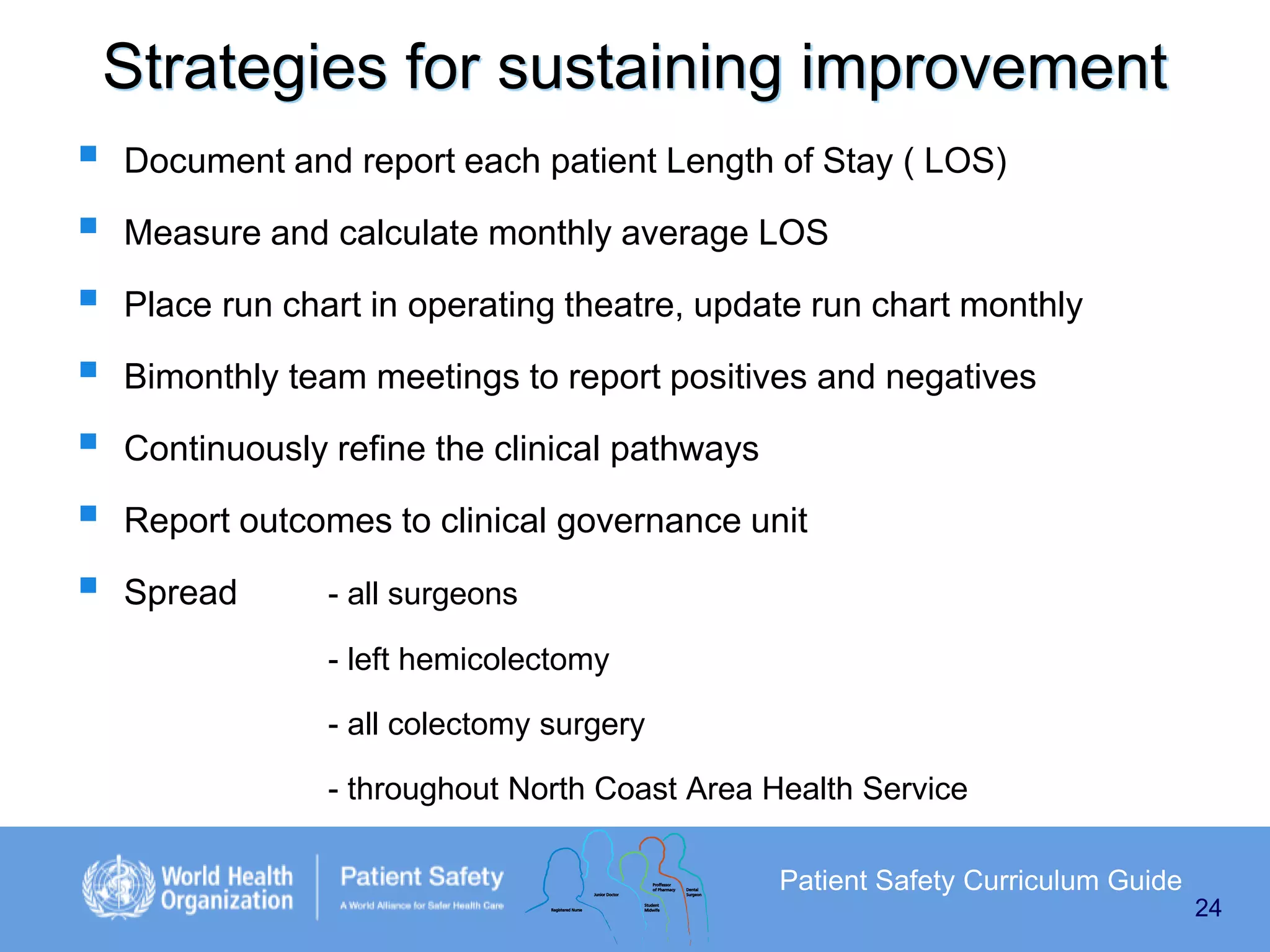
This document outlines the use of quality improvement methods to improve patient care. It describes principles of quality improvement like understanding variation and using the Plan-Do-Study-Act (PDSA) cycle. Tools for improvement include root cause analysis, failure mode and effects analysis, and clinical practice improvement methodology. The PDSA cycle is the core model for testing changes. Measurement is important for both research and learning, and different measures include outcomes, processes, and balancing measures.