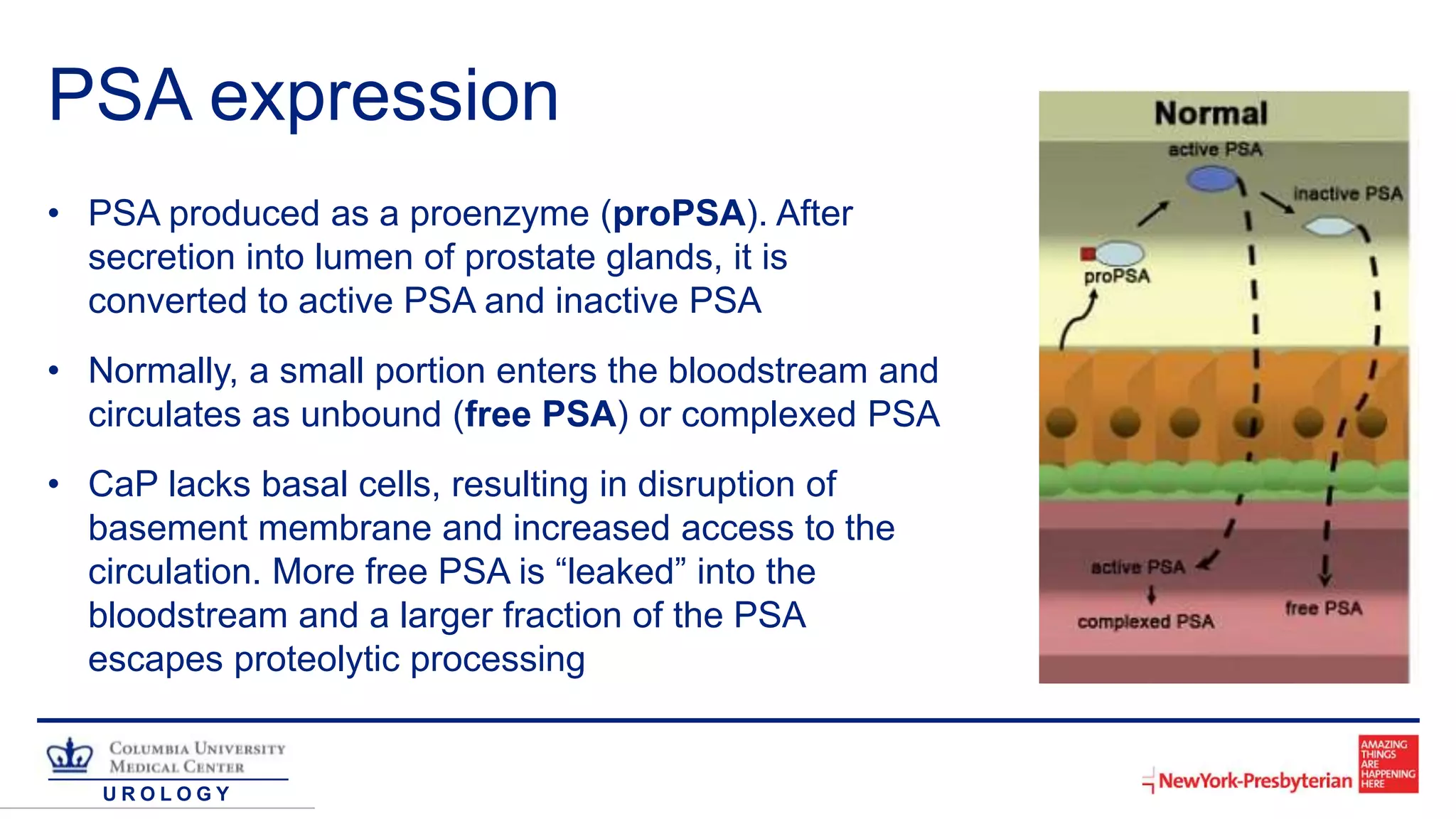
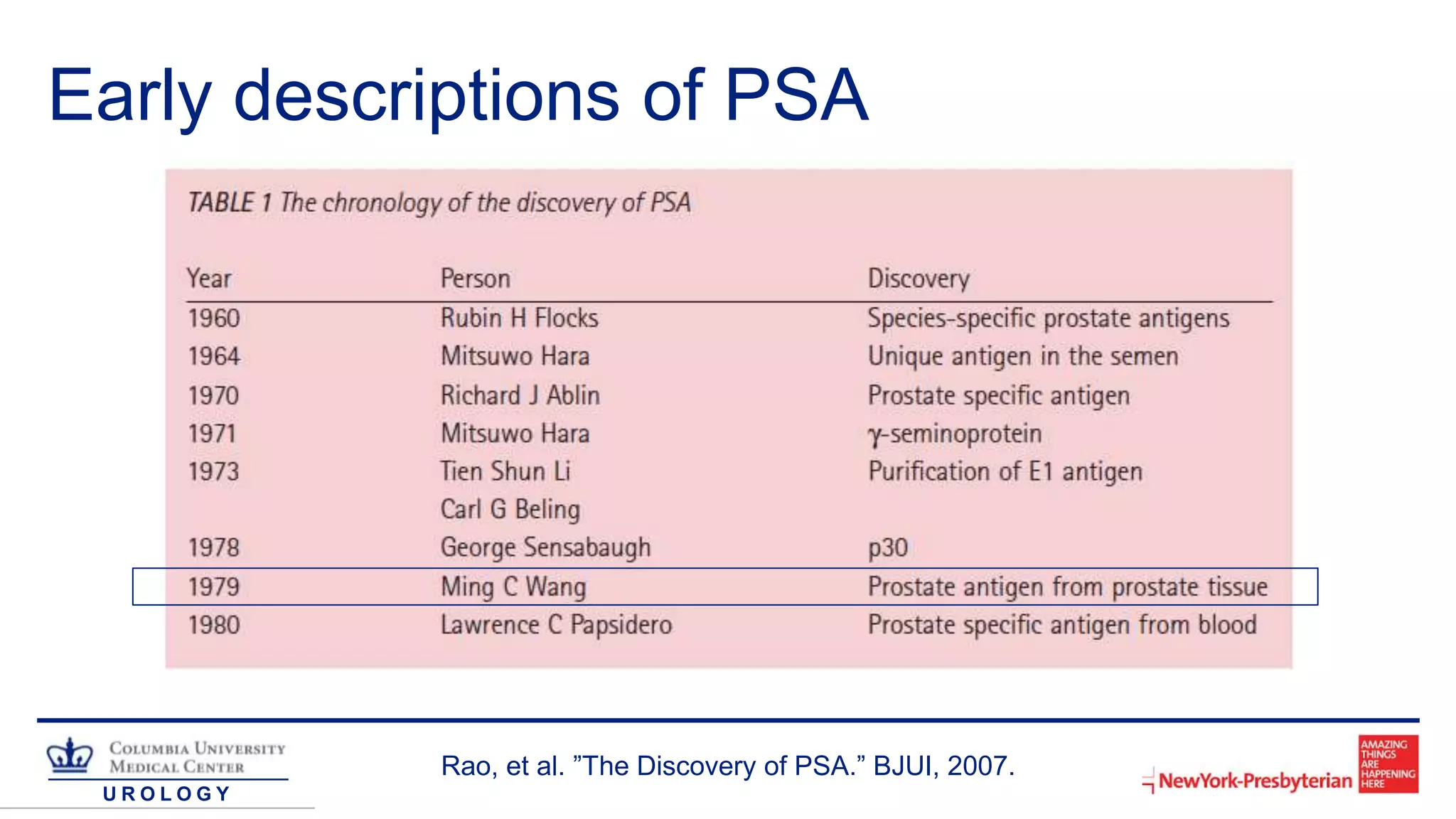
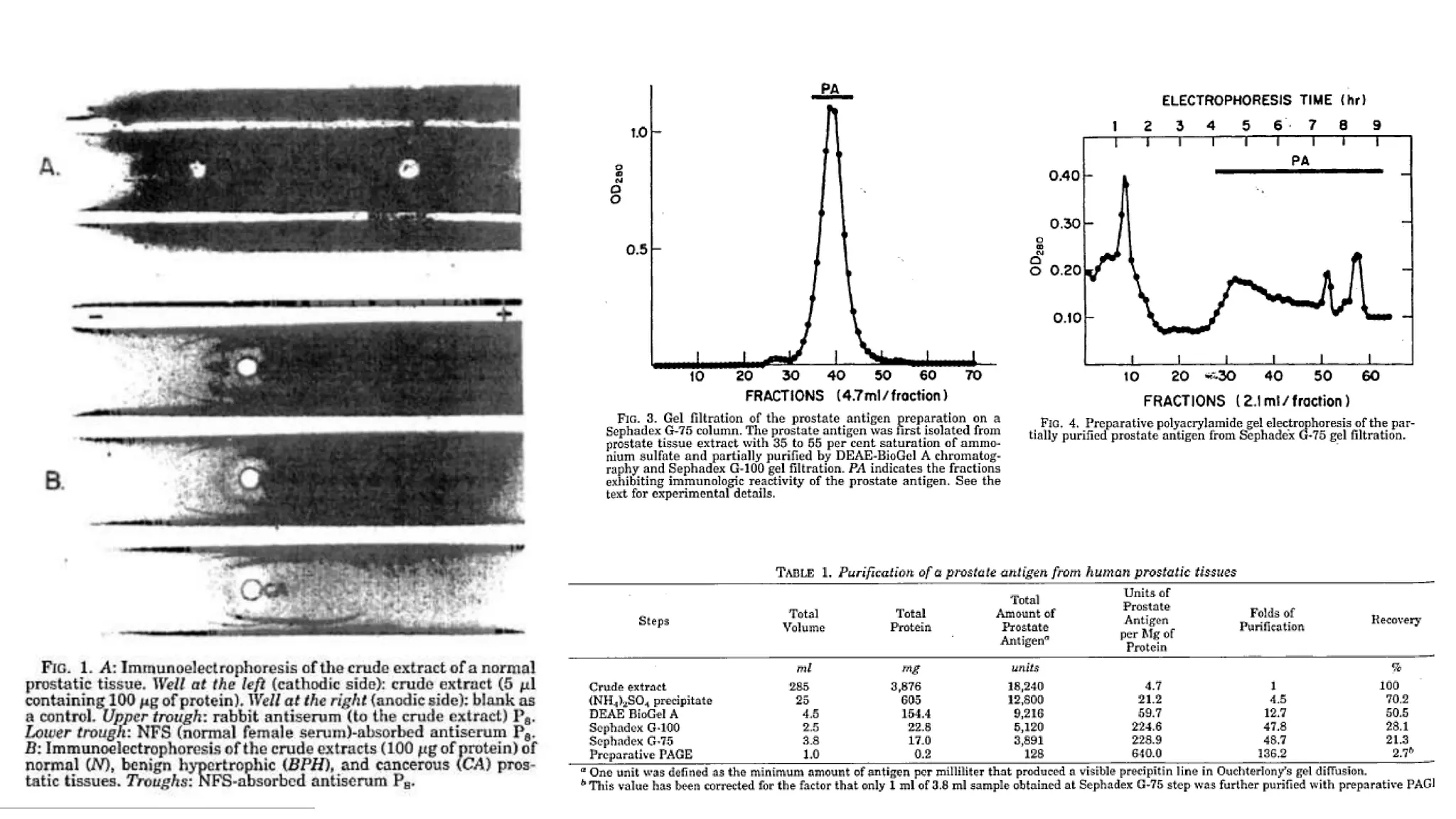
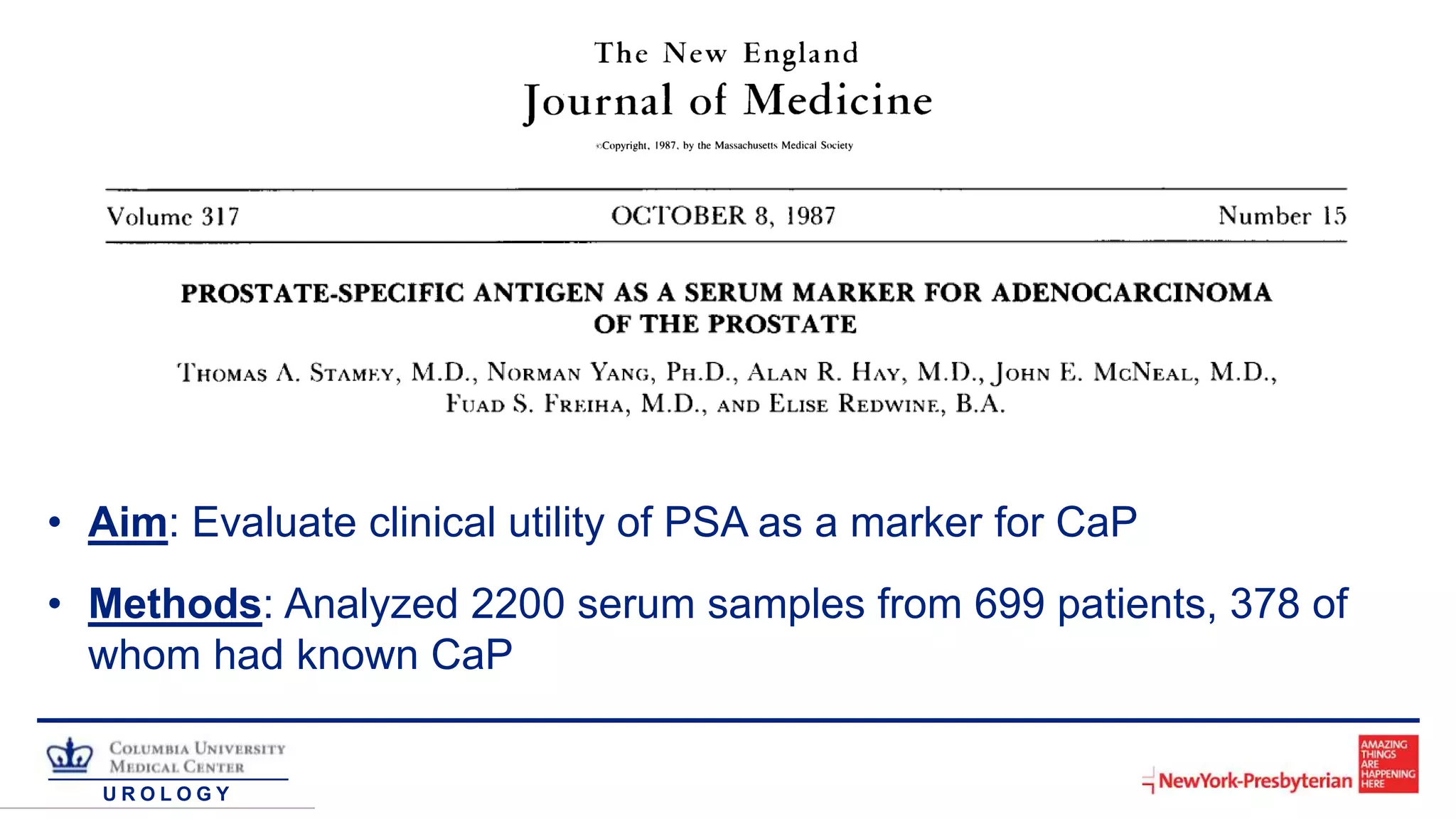
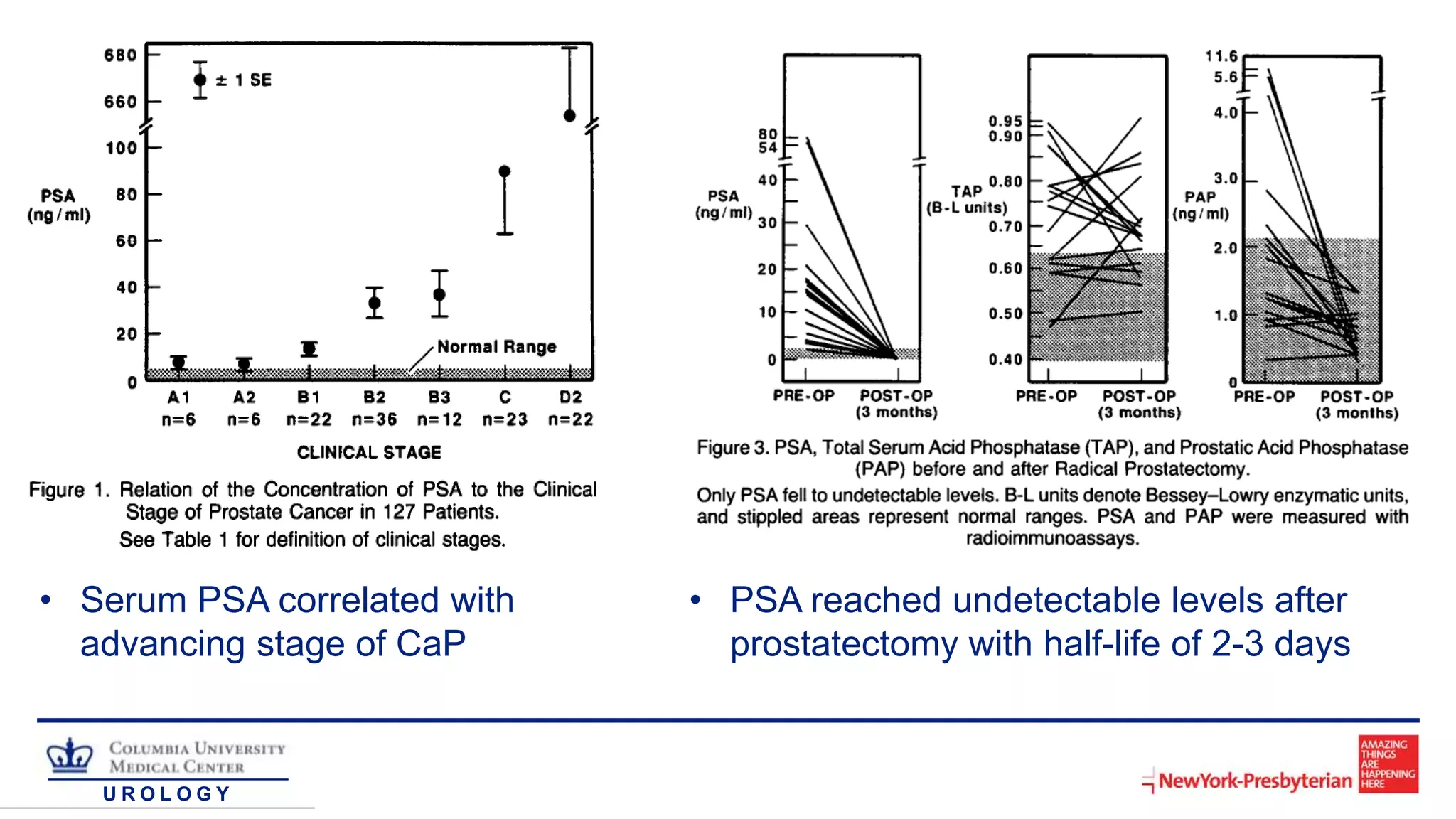
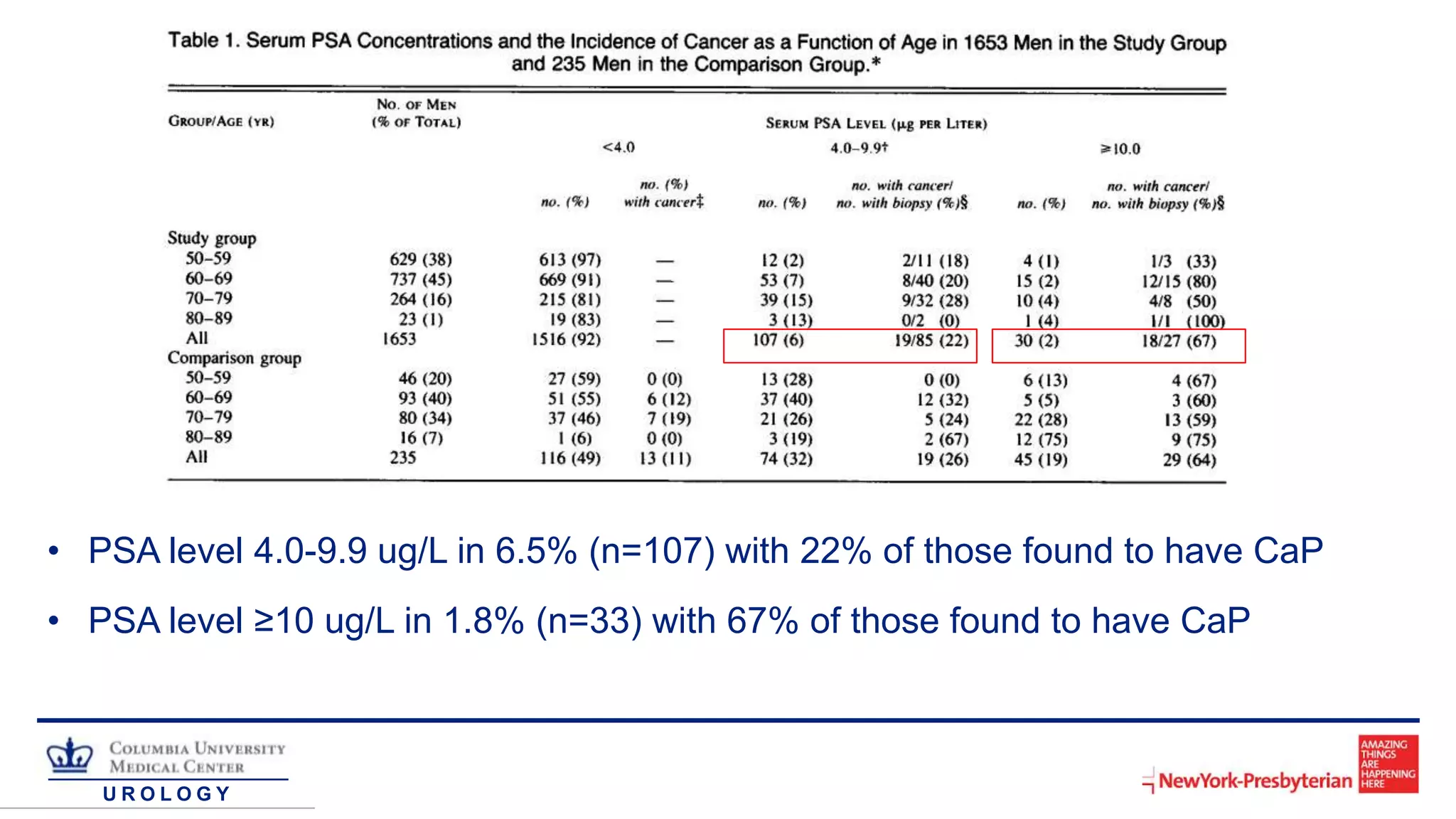
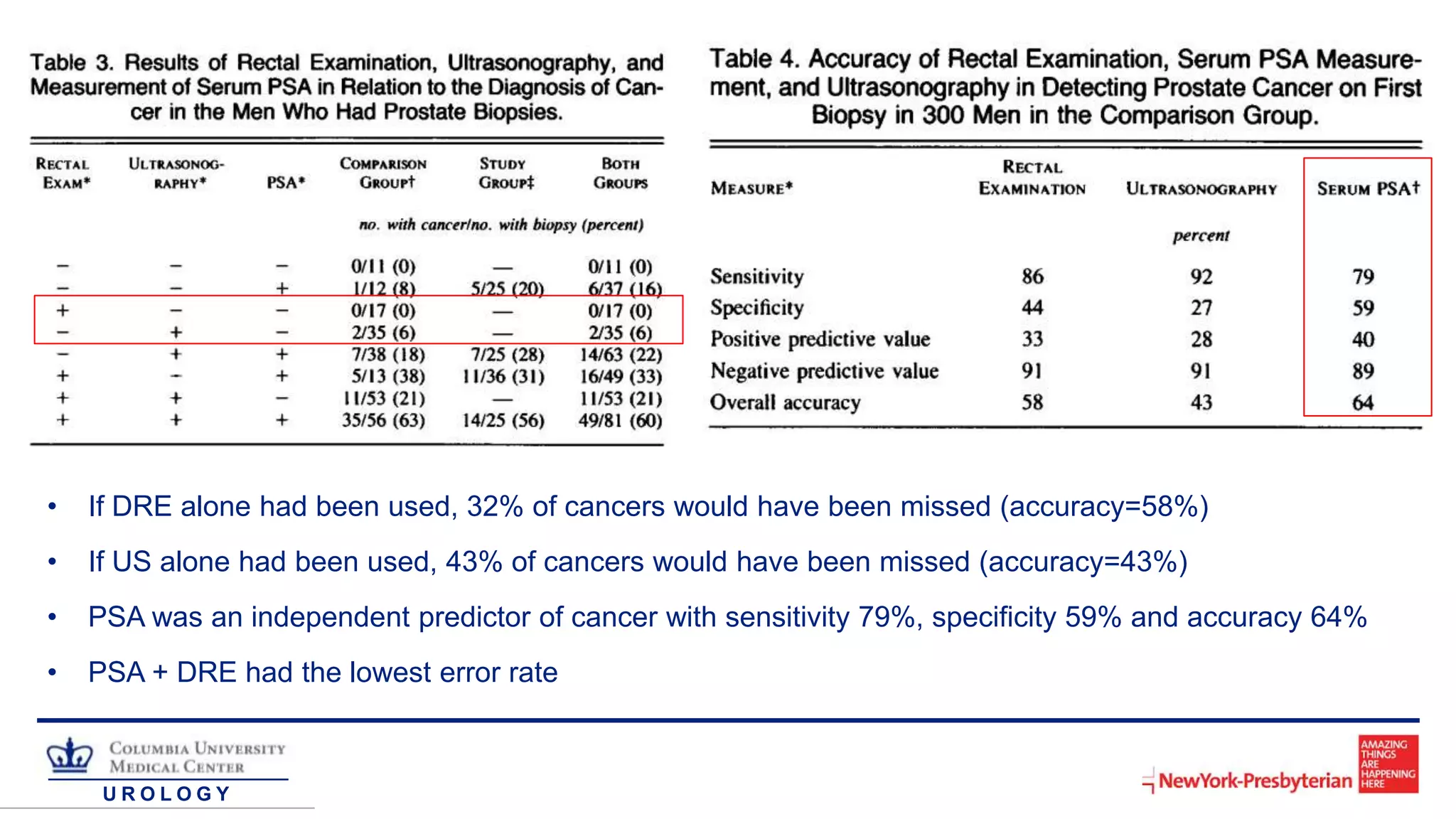
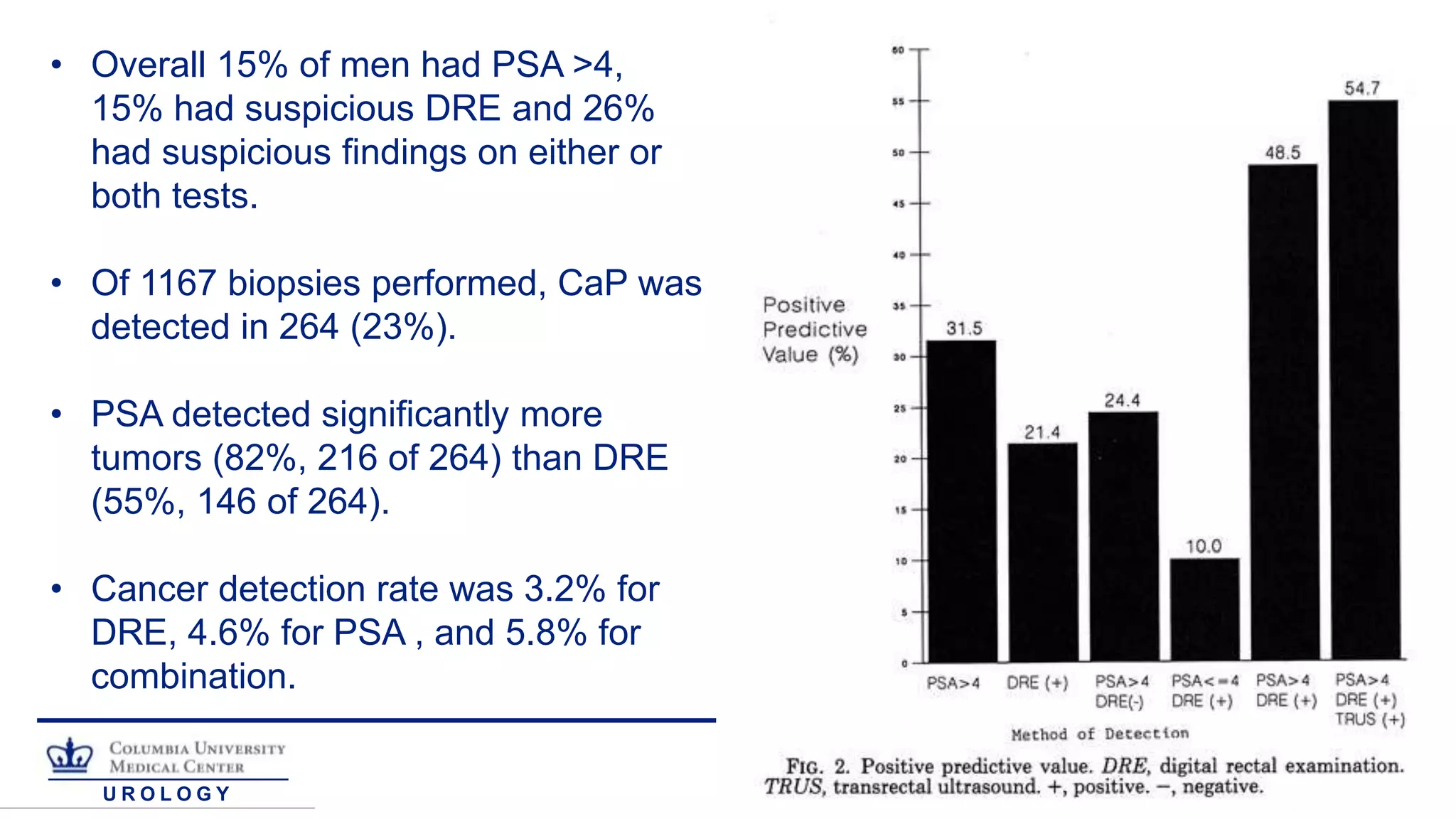
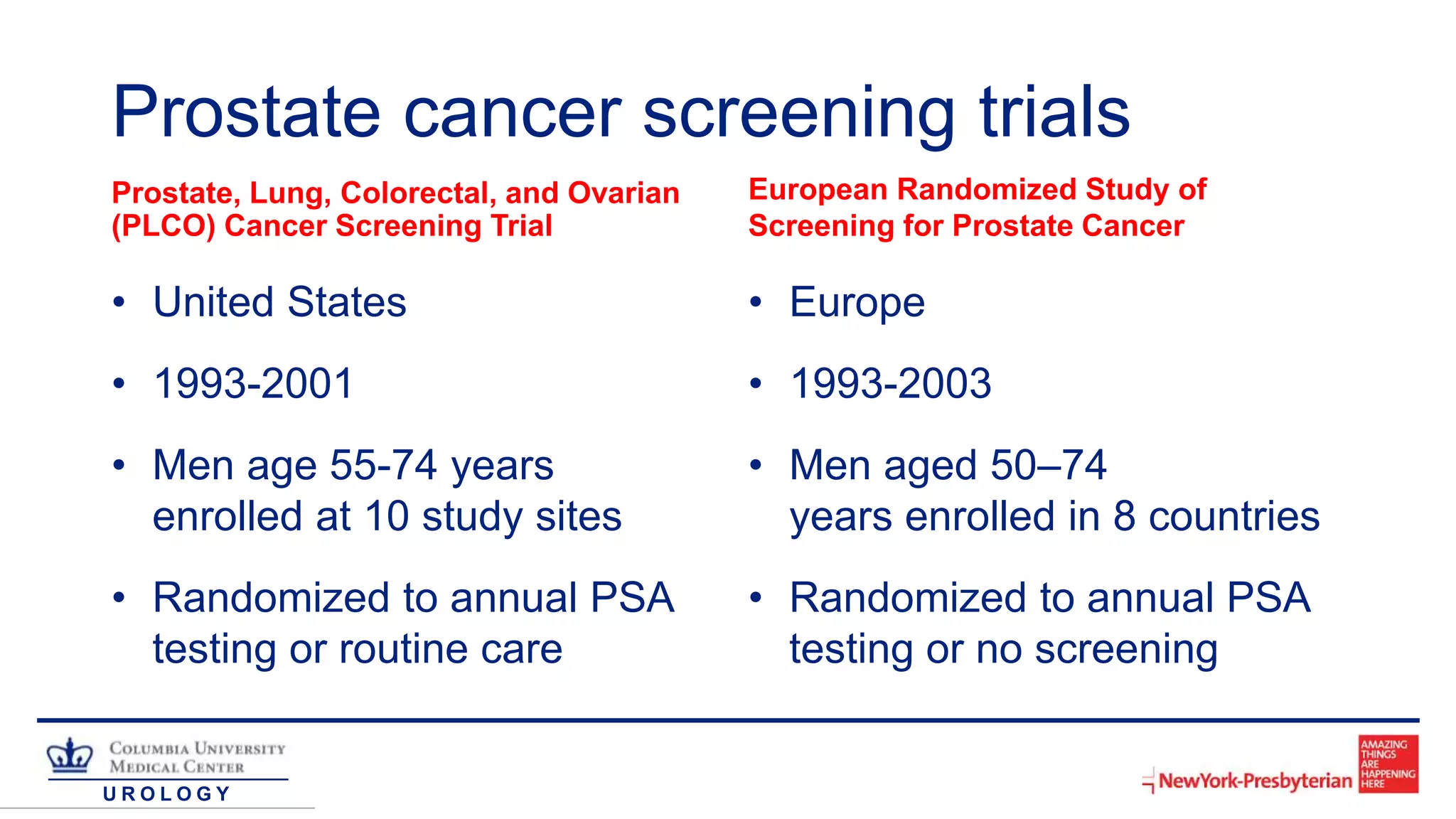
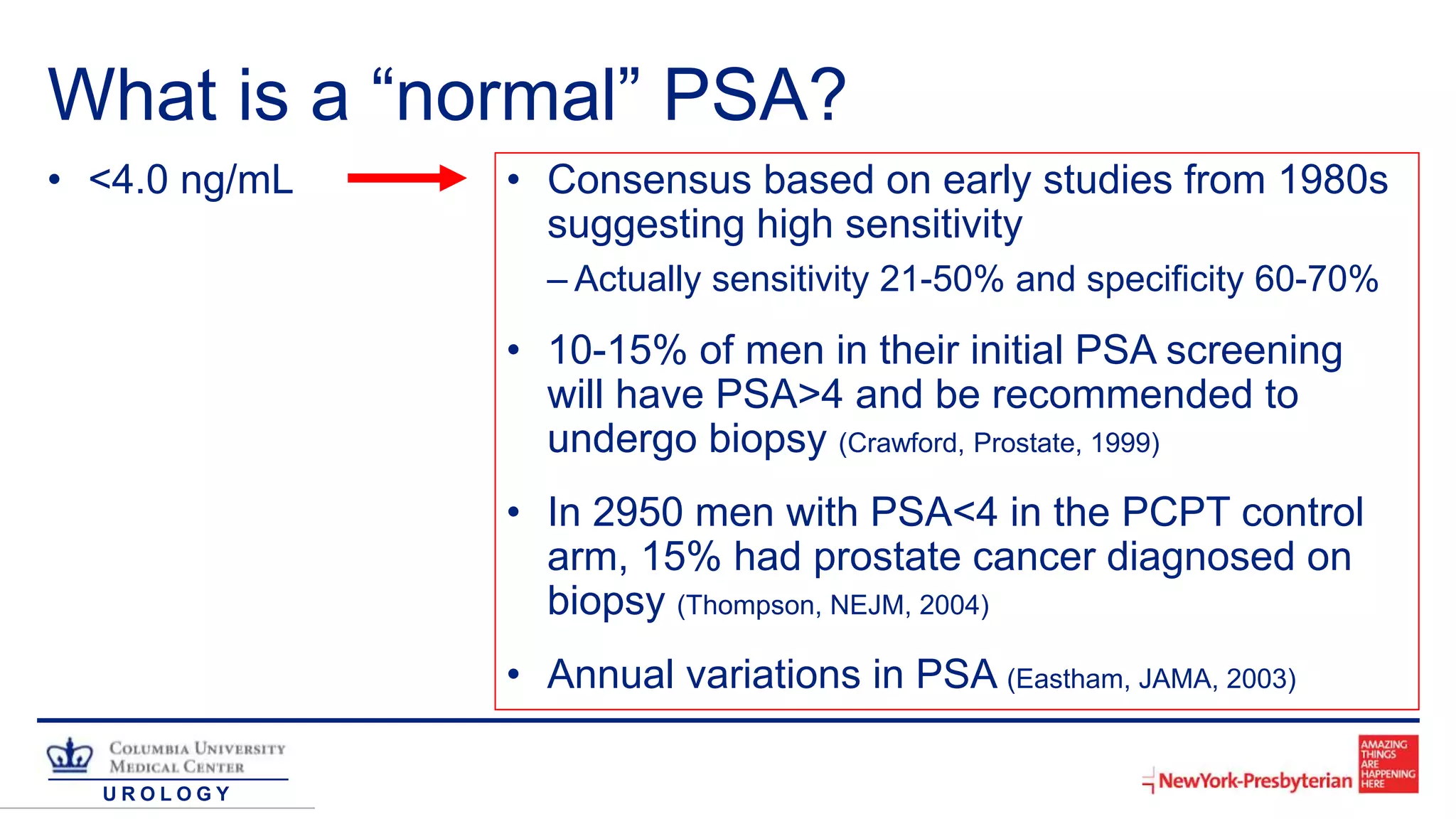
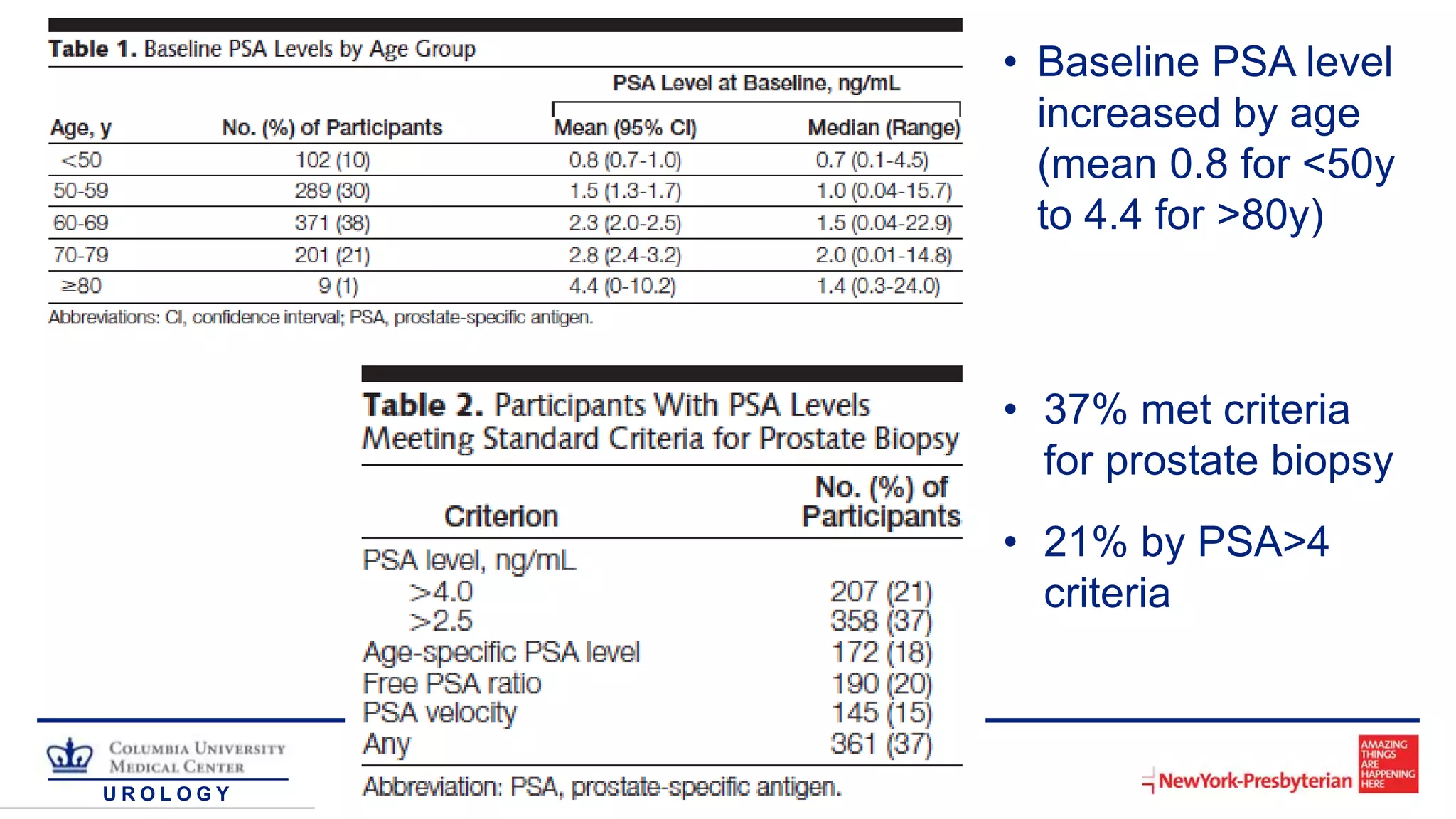
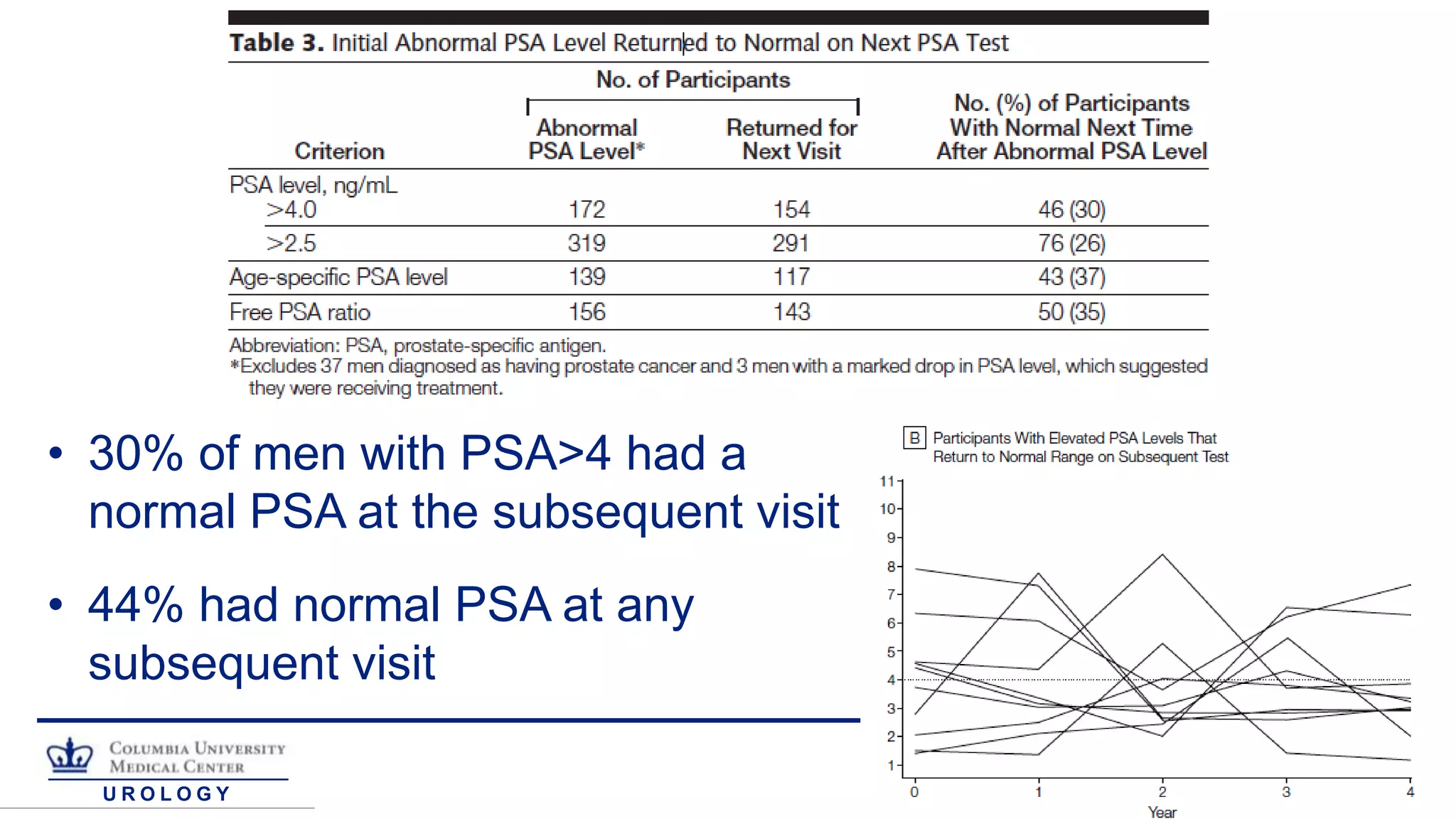
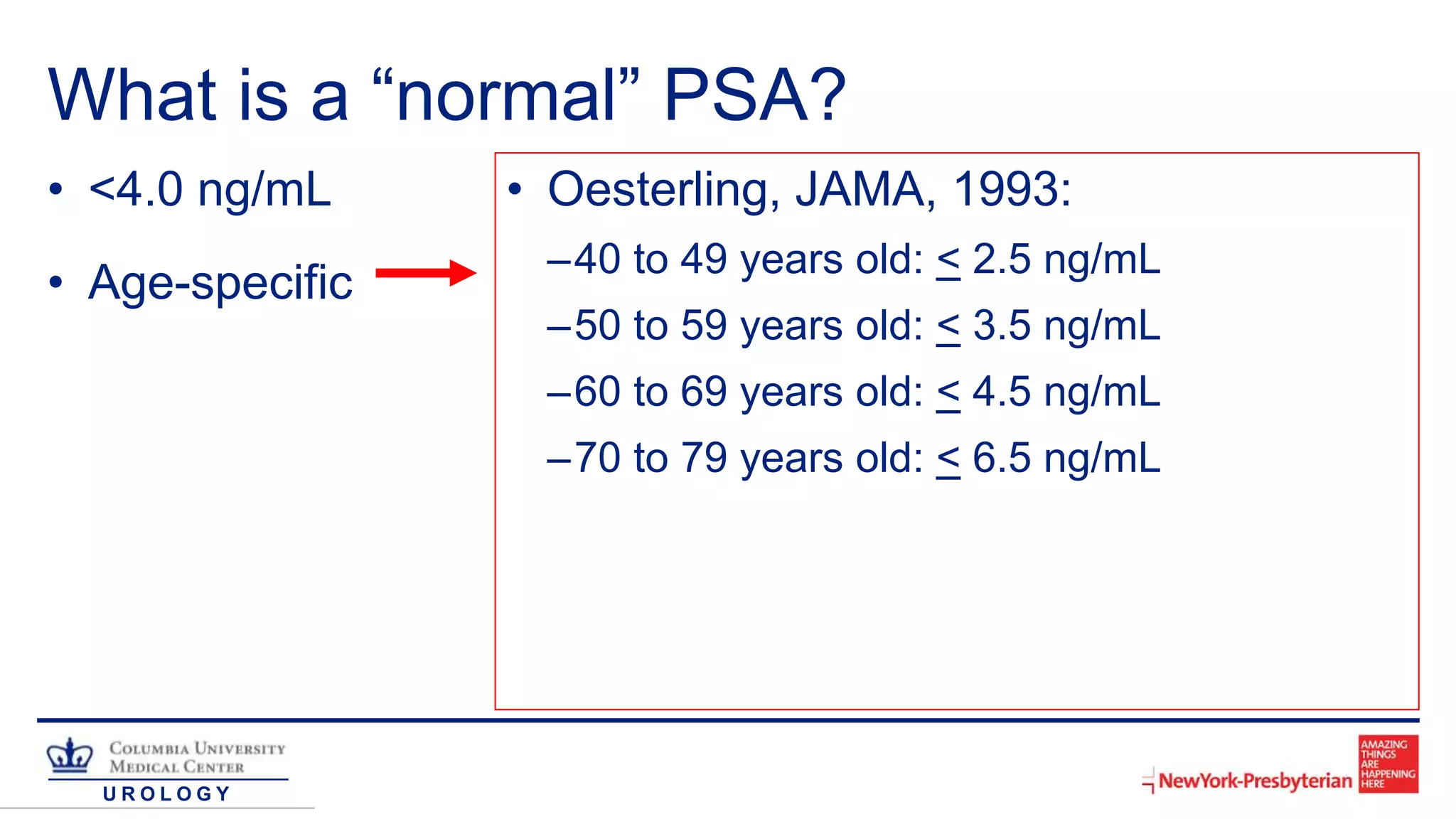
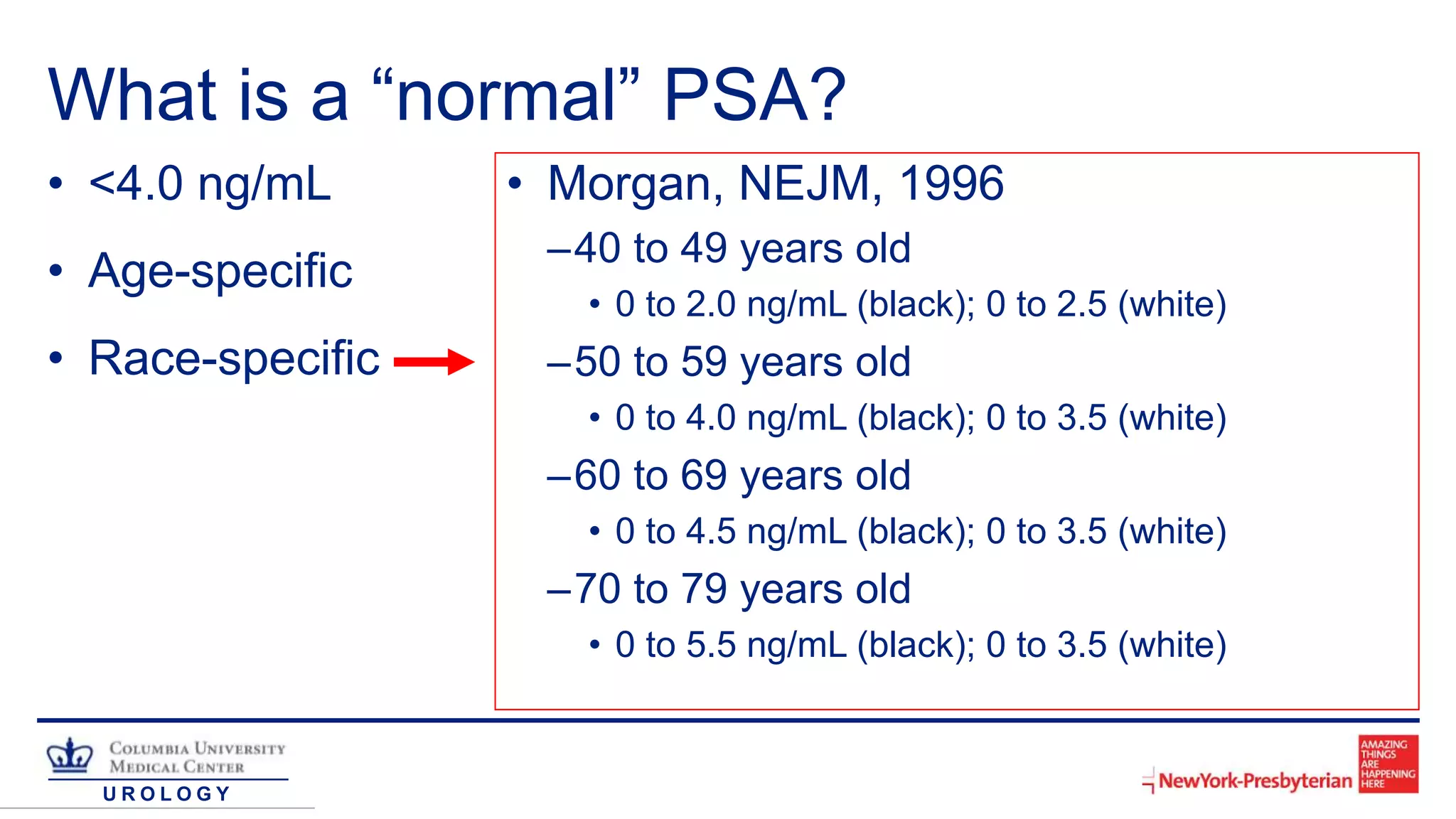
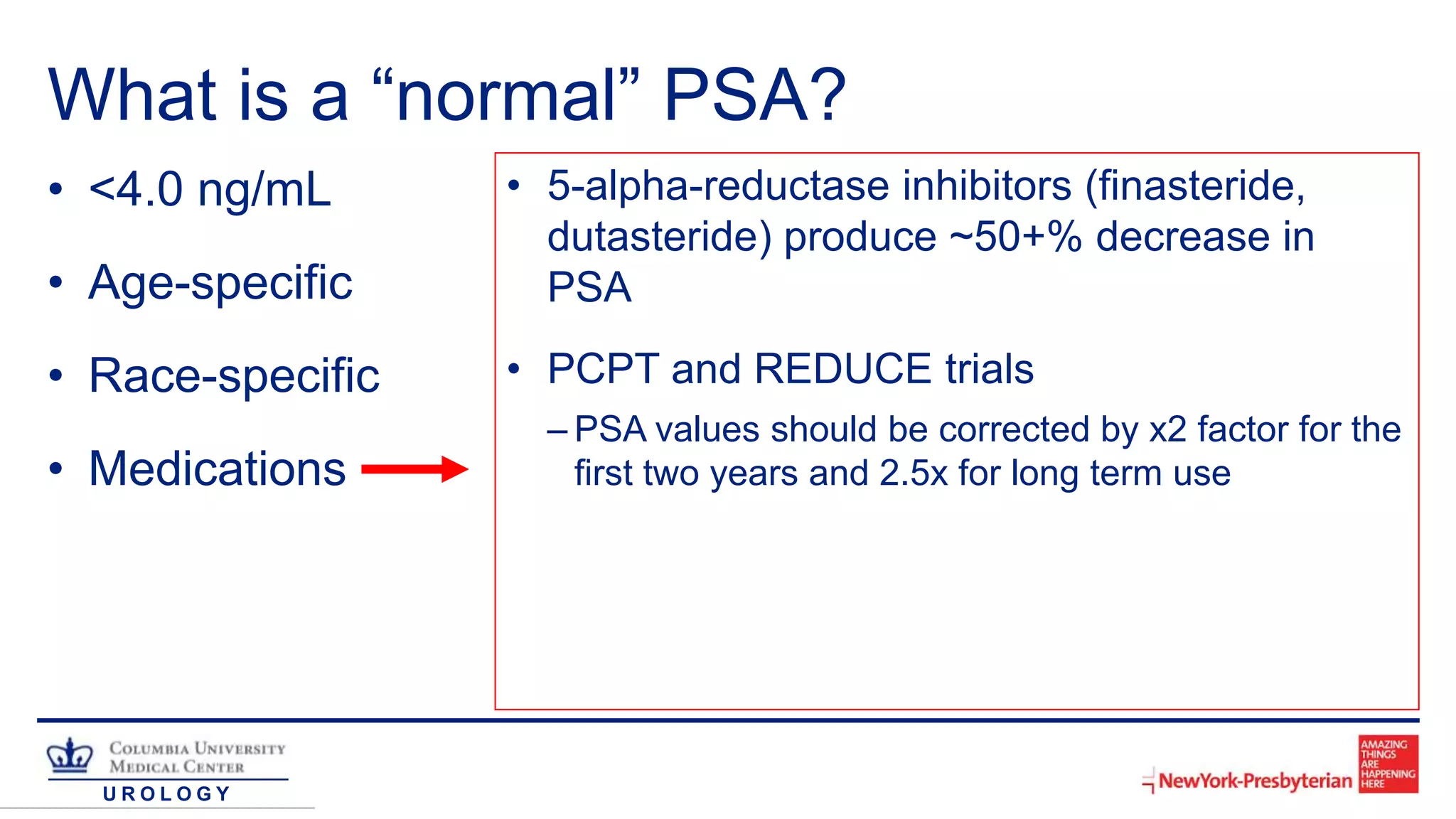
The document discusses the biochemistry, history, and measurement of prostate-specific antigen (PSA), emphasizing its role as a biomarker for prostate cancer detection and staging. It outlines normal PSA values, causes of elevated PSA levels, and the efficacy of PSA in screening compared to digital rectal examination (DRE). The document concludes that while serum PSA is a valuable tool, it has limitations due to a wide range of 'normal' values and various factors that can elevate PSA levels.