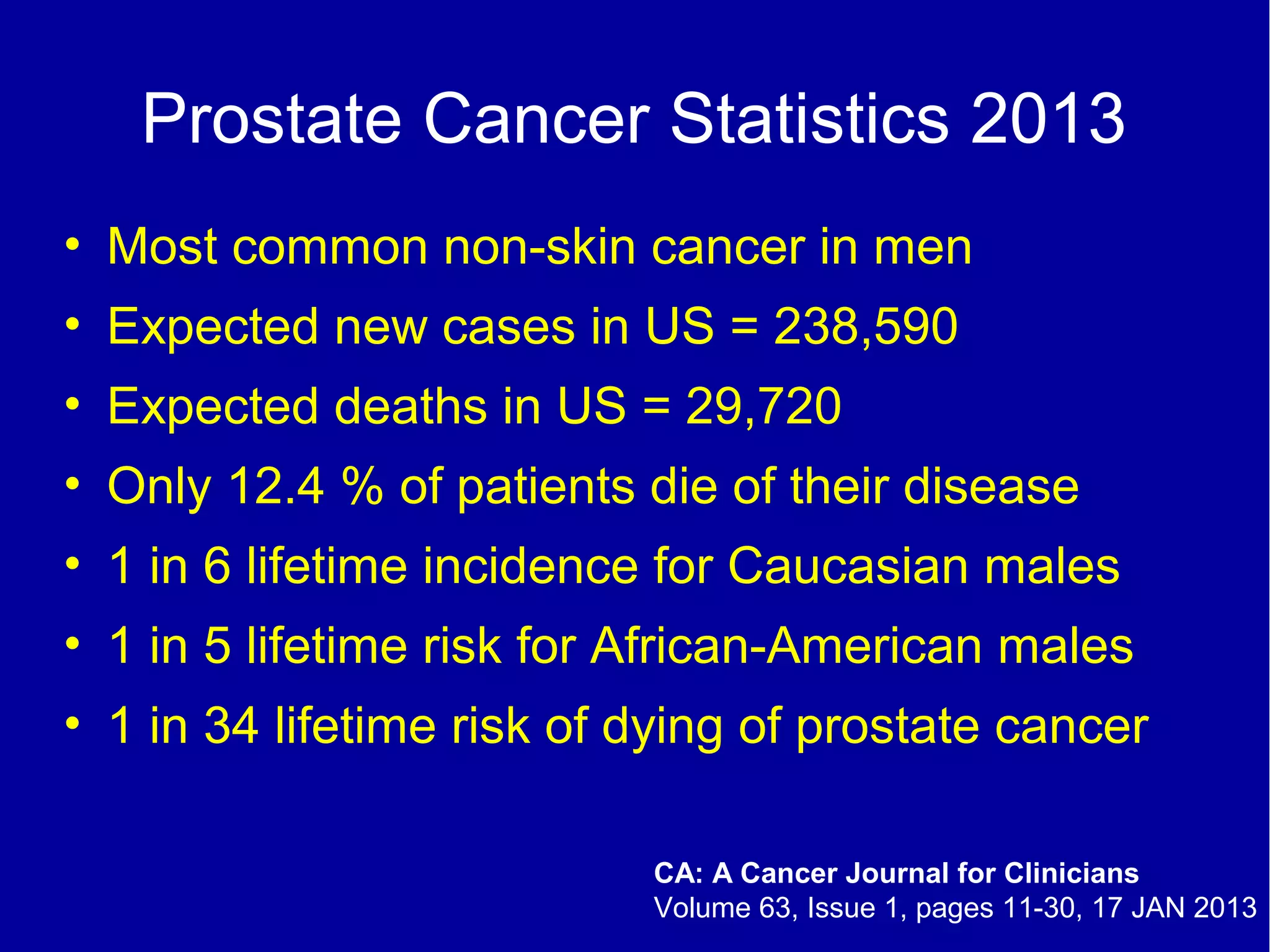
The document discusses prostate cancer screening, highlighting that it is the most common non-skin cancer in men with significant incidence and mortality statistics. It reviews the effectiveness of PSA screening, noting a decline in prostate cancer mortality, yet raises concerns about overdiagnosis and the necessity for individualized screening protocols. It concludes by emphasizing the importance of informed and shared decision-making in screening practices.