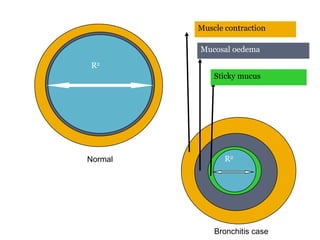
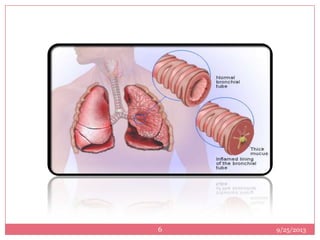
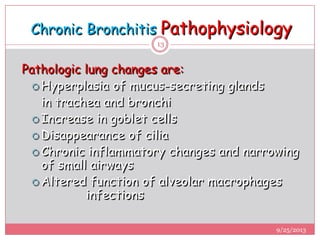
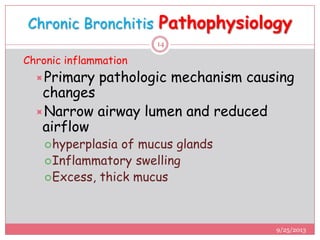
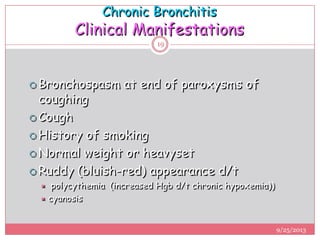
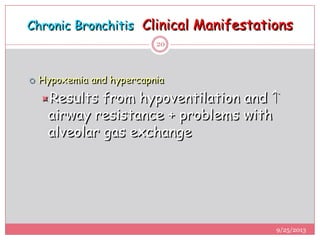
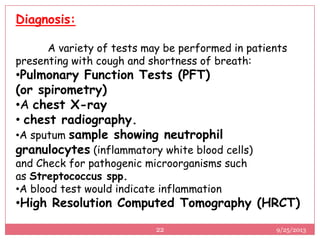
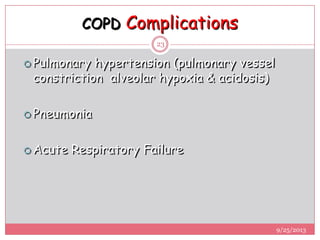
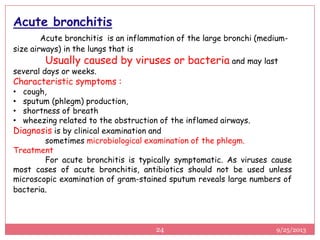
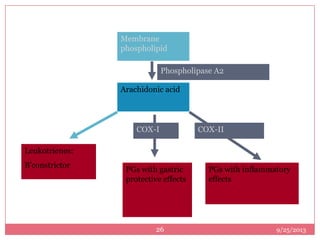
The document provides a detailed overview of bronchitis, a component of chronic obstructive pulmonary disease (COPD), highlighting its types, causes, symptoms, and pathophysiology. Chronic bronchitis is characterized by a persistent productive cough and is typically caused by factors such as smoking and pollution, leading to airway obstruction and inflammation. Treatment options include anti-inflammatory medications and bronchodilators, with a clinical focus on diagnosis and management strategies.
![BY
SROTA DAWN.
M.PHARM [PHARMACOLOGY]
SUBJECT - PHARMACOLOGY -∏
VELS SCHOOL OF PHARMACEUTICAL SCIENCES
BRONCHITIS
[PATHOLOGY & TREATMENT]
9/25/2013
1](https://image.slidesharecdn.com/presentation2bronchitissrota-130925142157-phpapp01/75/bronchitis-pathology-and-treatment-by-srota-dawn-1-2048.jpg)