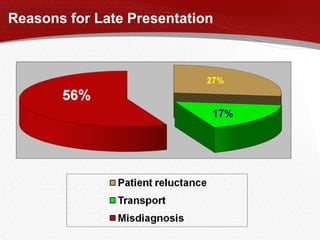
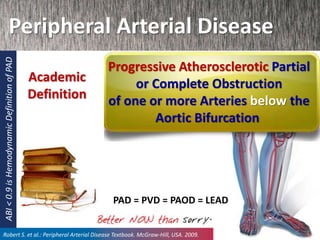
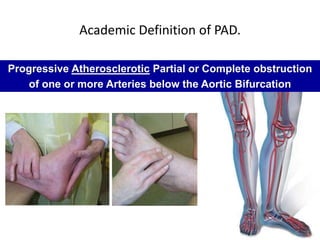
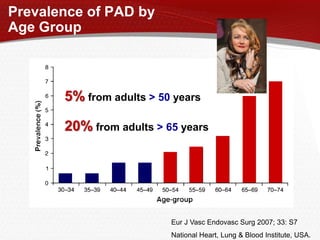
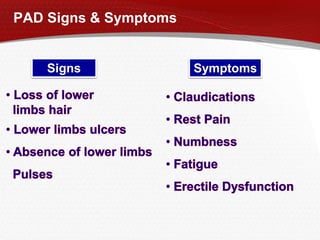
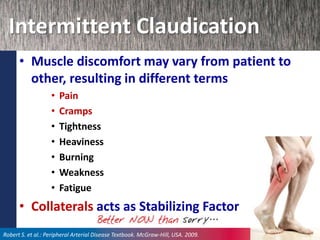
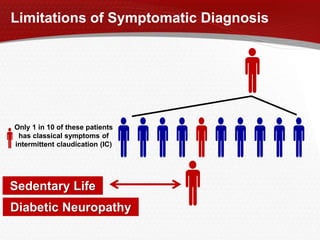
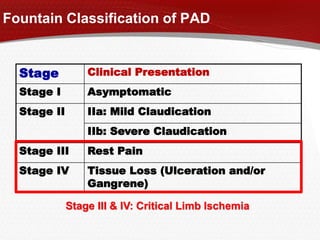
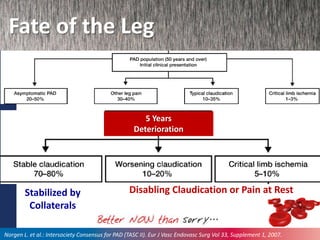
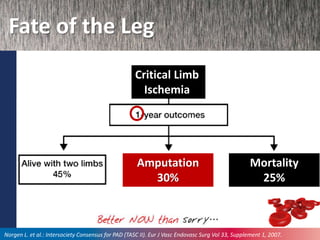
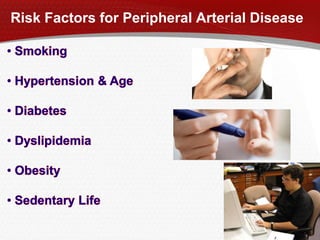
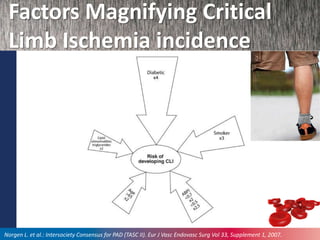
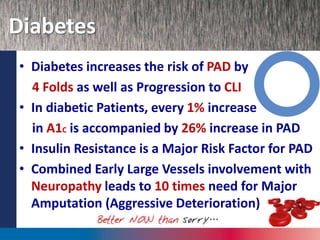
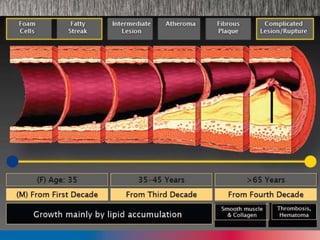
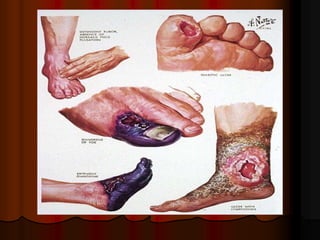
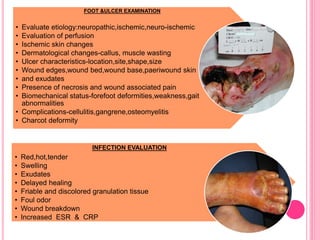
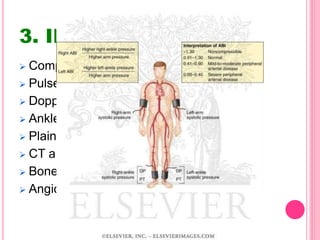
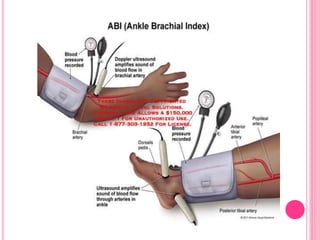
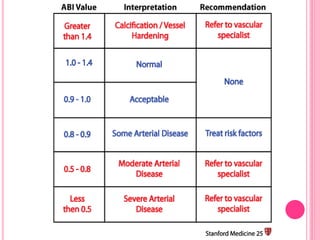
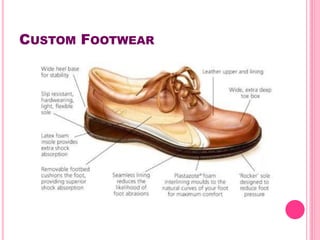
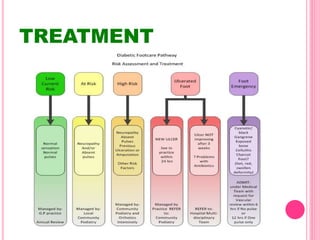
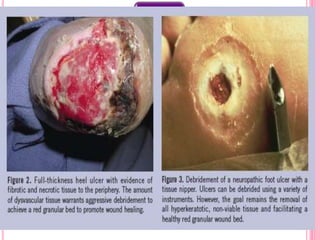
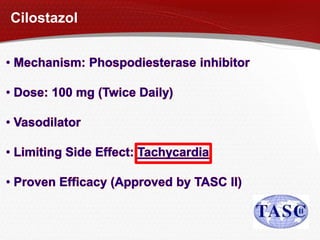
Peripheral Arterial Disease (PAD) is the progressive obstruction of arteries below the aortic bifurcation due to atherosclerosis. It has a prevalence of 5-20% in those over 50 years old. Symptoms range from intermittent claudication to critical limb ischemia with rest pain and tissue loss. Late presentation is common due to asymptomatic or atypical symptoms. Diabetes significantly increases the risk and severity of PAD. Treatment involves risk factor modification, endovascular or surgical revascularization, wound care, and in severe cases amputation. Regular screening and multidisciplinary care can help prevent amputation in those with PAD and foot ulcers.