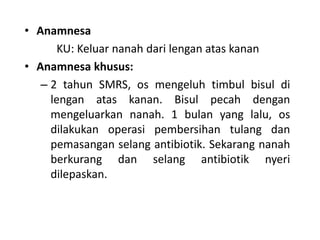
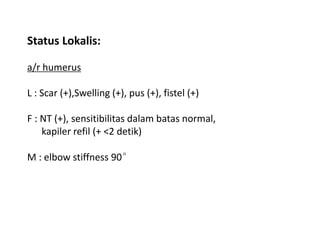
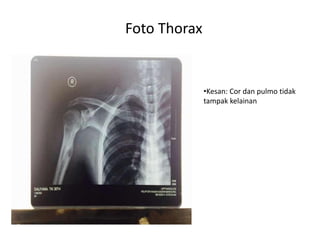
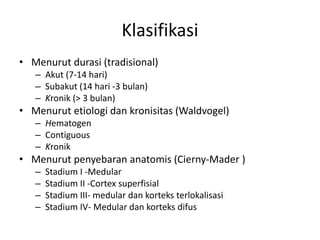
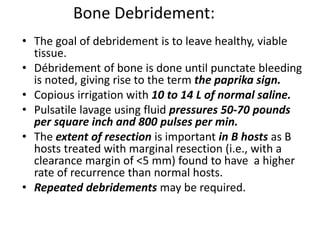
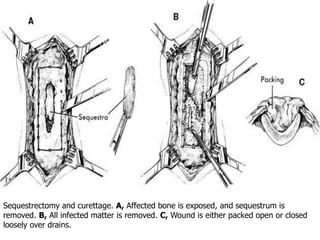
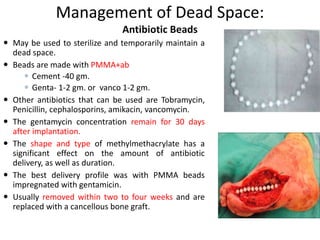
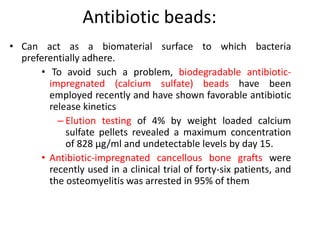
This document presents a detailed case report on chronic osteomyelitis in a 30-year-old male patient, including his medical history, physical examination results, and diagnostic imaging findings. It discusses the treatment methods, such as surgical interventions, antibiotic therapy, and management of complications, alongside the pathophysiology and clinical presentation of osteomyelitis. Additionally, it includes information on various diagnostic techniques and the classification of osteomyelitis, aiming to provide a comprehensive overview for medical professionals.