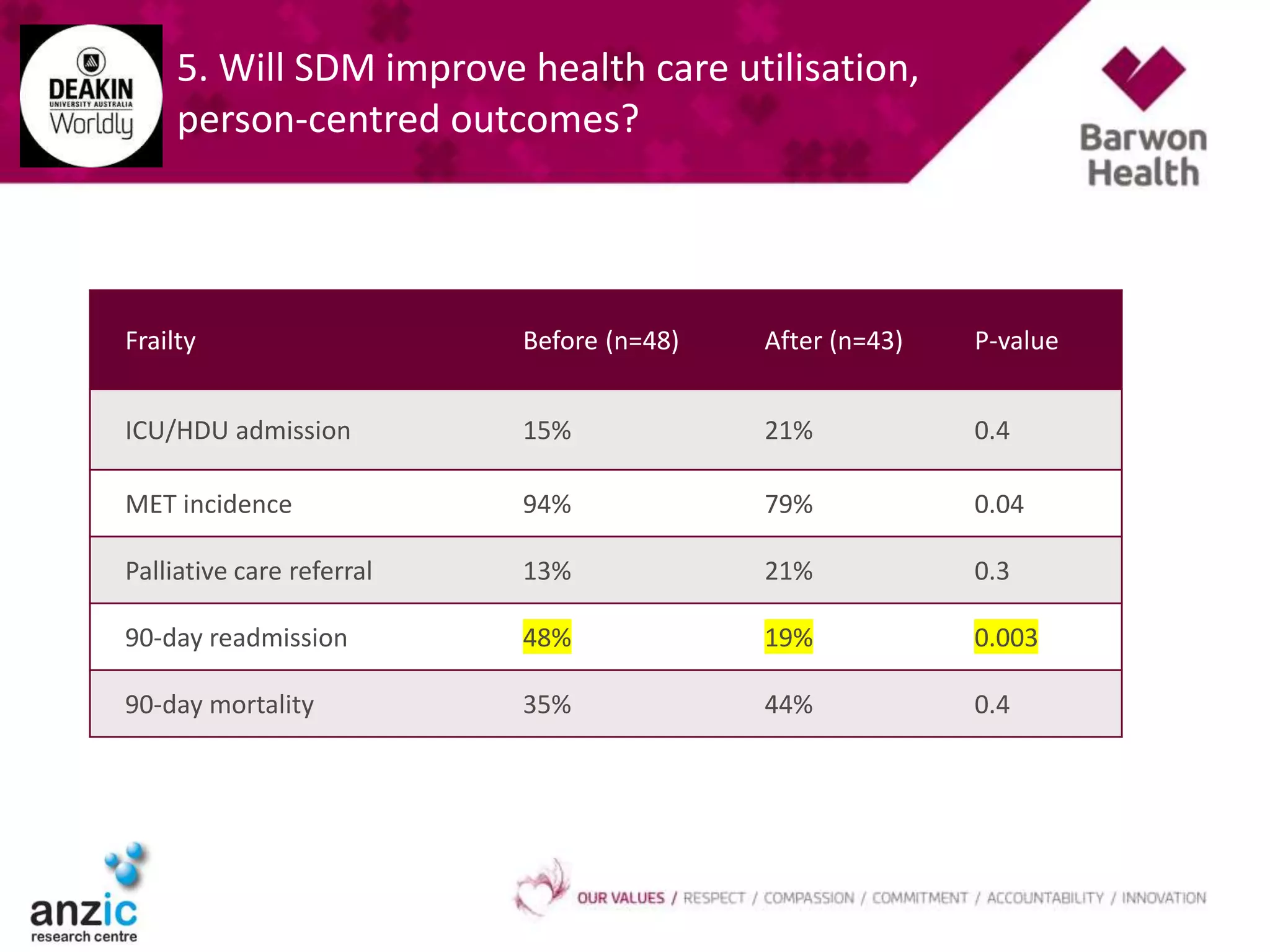
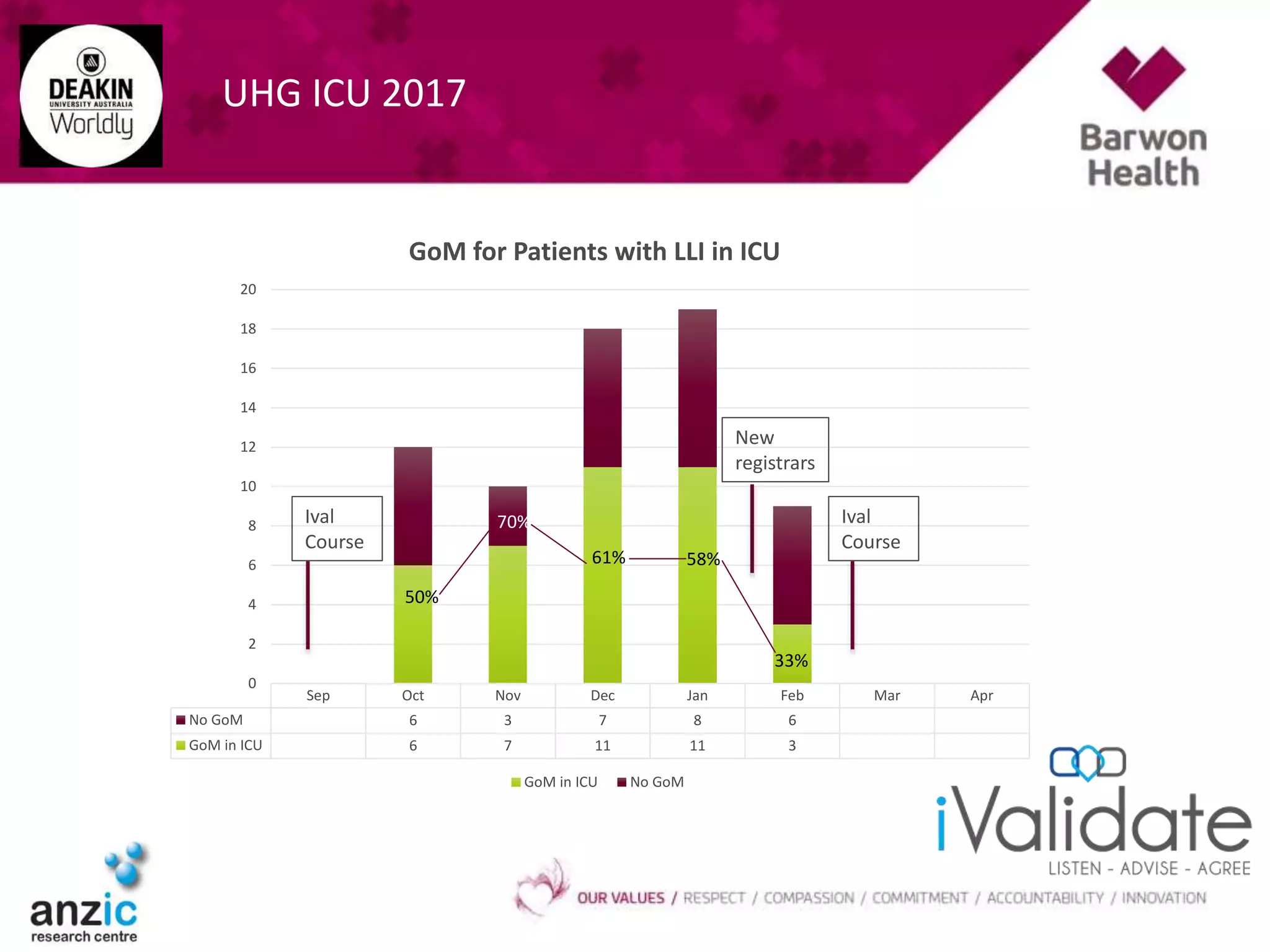
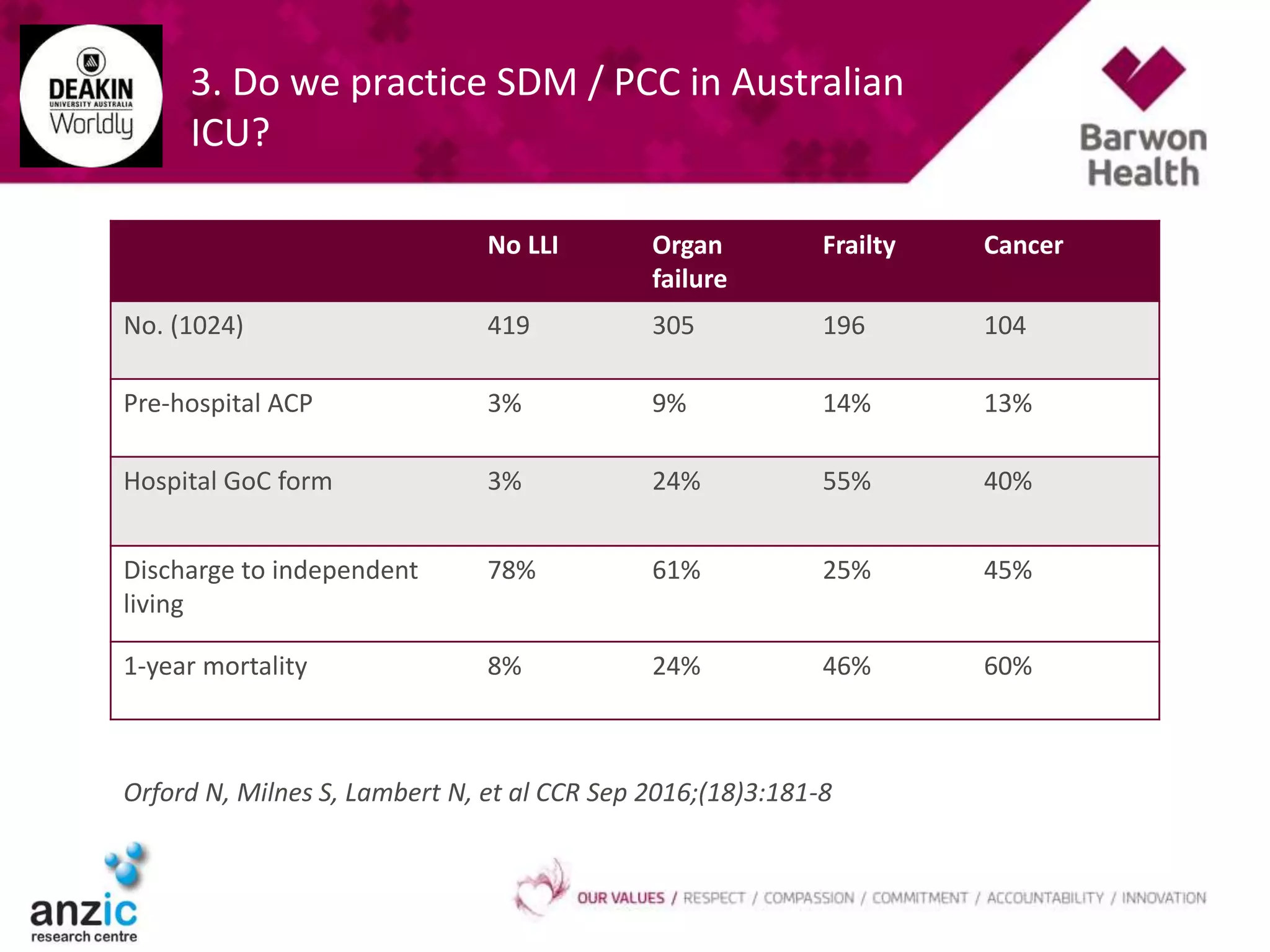
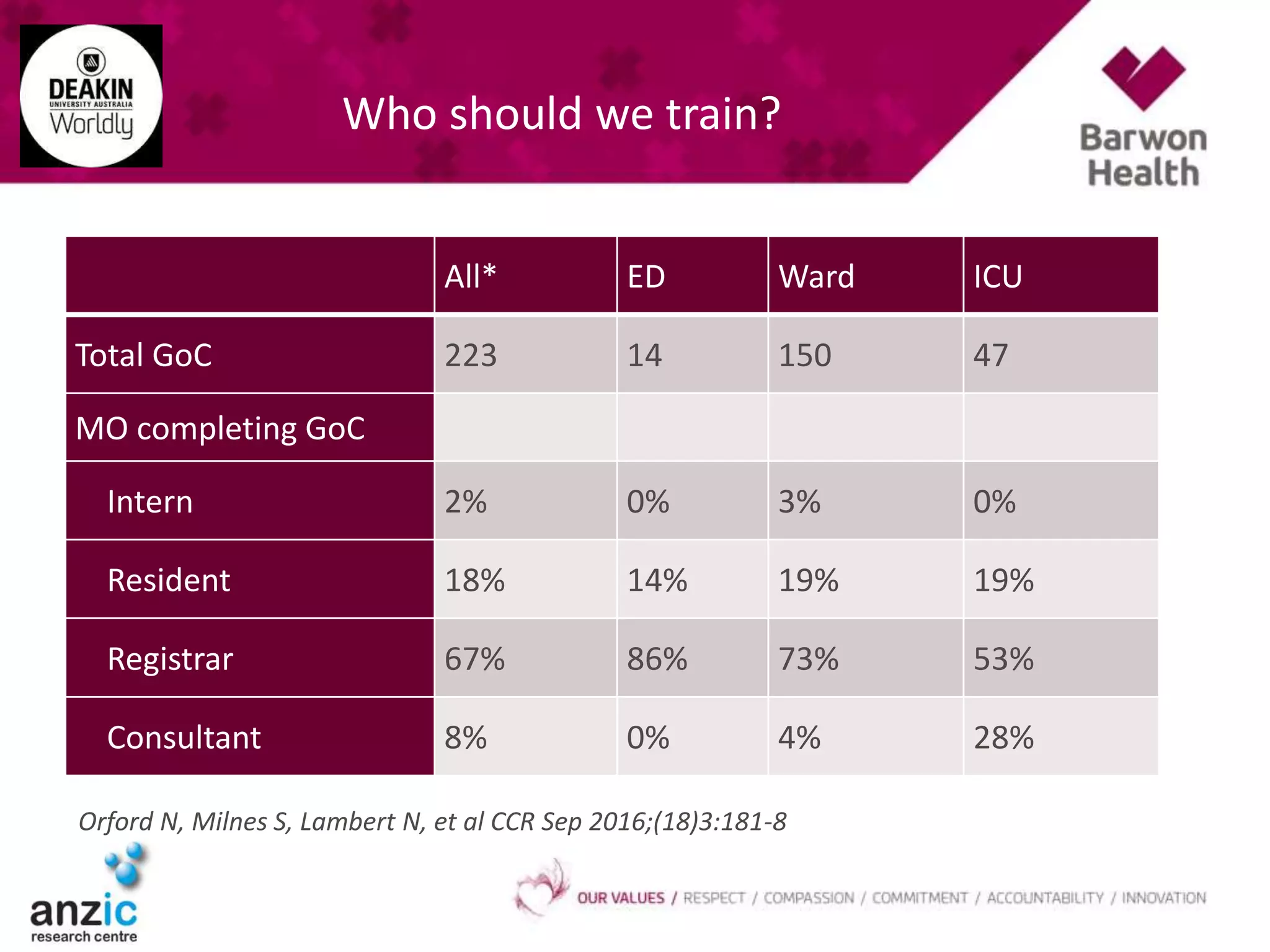
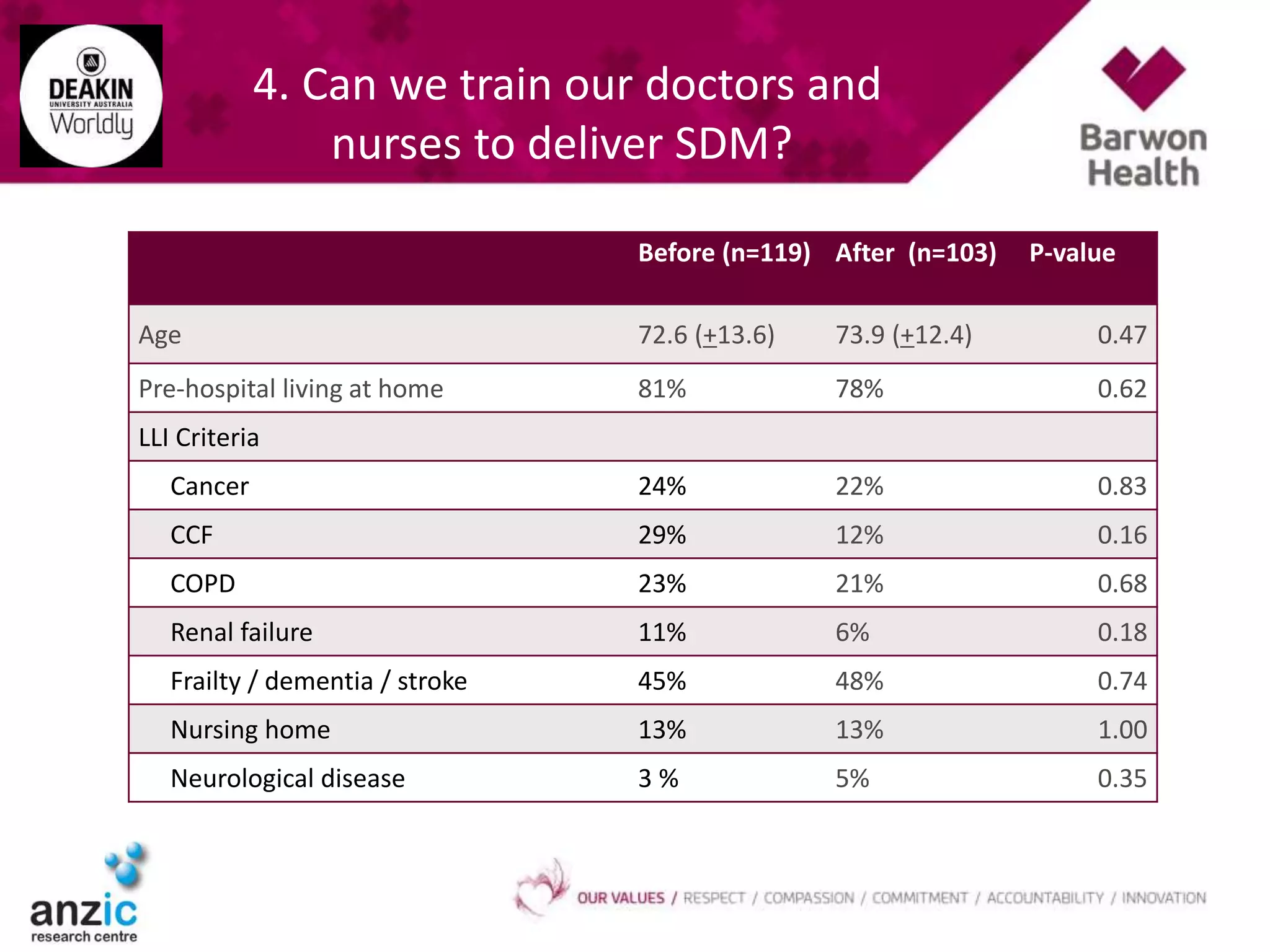
The document discusses the practice of shared decision-making (SDM) and person-centred care (PCC) in Australian ICUs, addressing key questions about identifying high-risk patients, current practices, and training healthcare providers. It presents data on various patient outcomes before and after implementing communication skills training for SDM. The findings suggest that while there are improvements in documentation and discussion of patient values, the overall healthcare utilization and patient-centered outcomes varied, indicating mixed results in the adoption of SDM.










![5. Will SDM improve health care utilisation,
person-centred outcomes?
Before (n=119) After (n=103) P-value
Admission ICU/HDU 21% 29% 0.16
MET call incidence 88% 73% 0.009
Palliative Care referral 24% 24% 0.90
Hosp LOS 9 [4,19] 9 [5,15] 0.80
Hospital mortality 29% 24% 0.47
90-day readmit 39% 31% 0.24
90-day mortality 47% 34% 0.05
Survival for cancer before and after](https://image.slidesharecdn.com/ivalicnno17-170312032845/75/Orford-iValidate-Improving-End-of-Life-Care-in-the-ICU-18-2048.jpg)