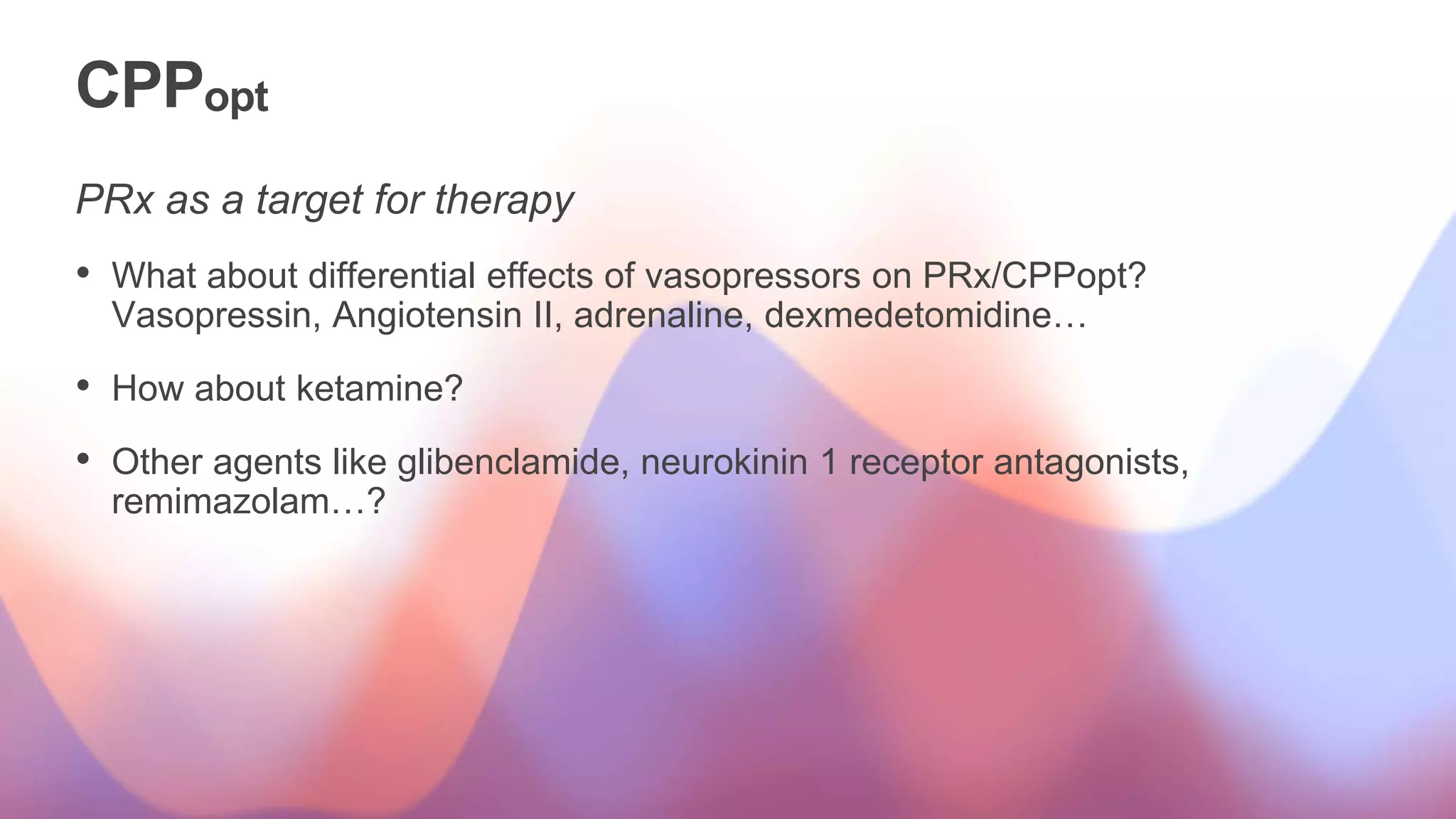
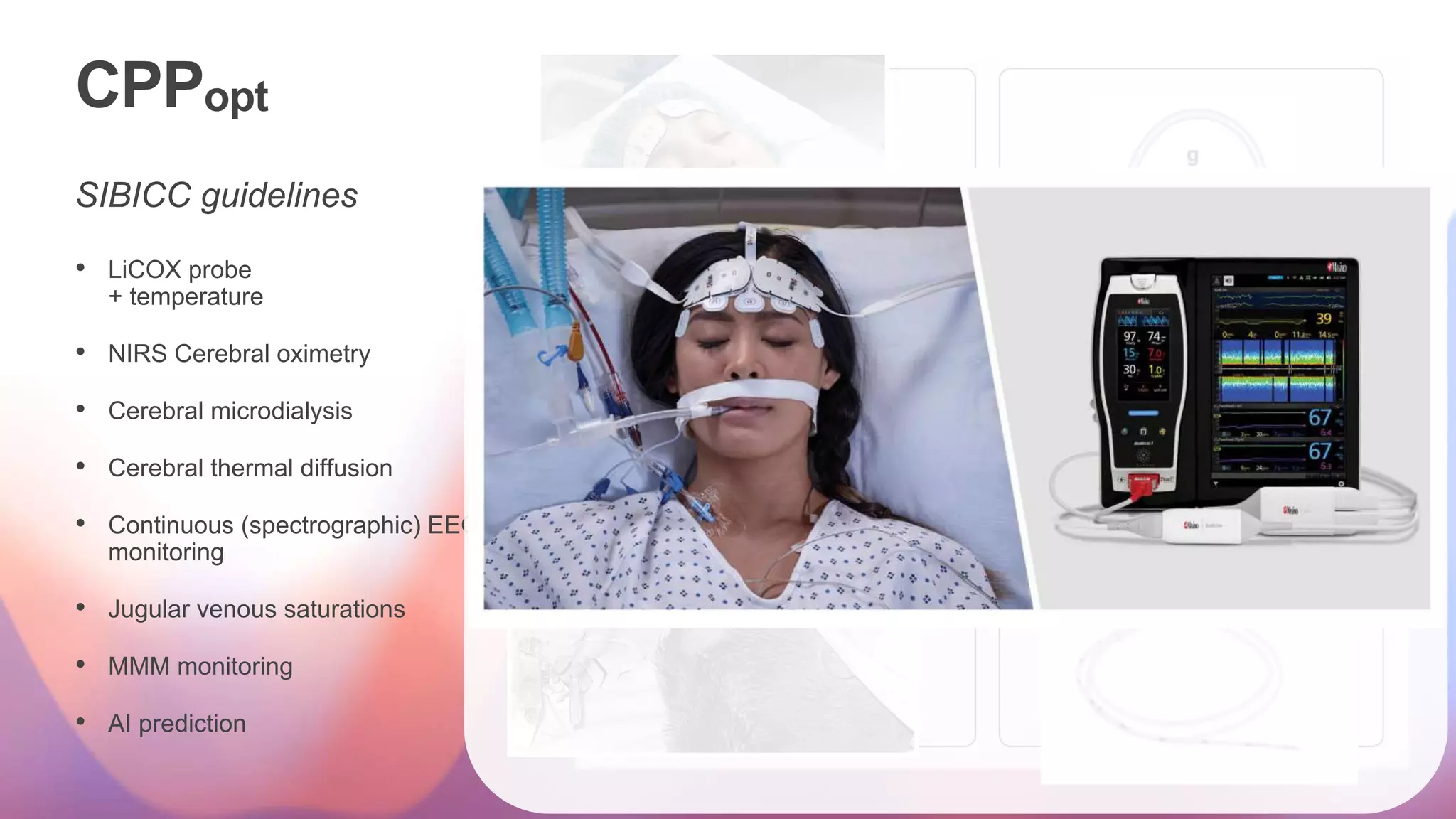
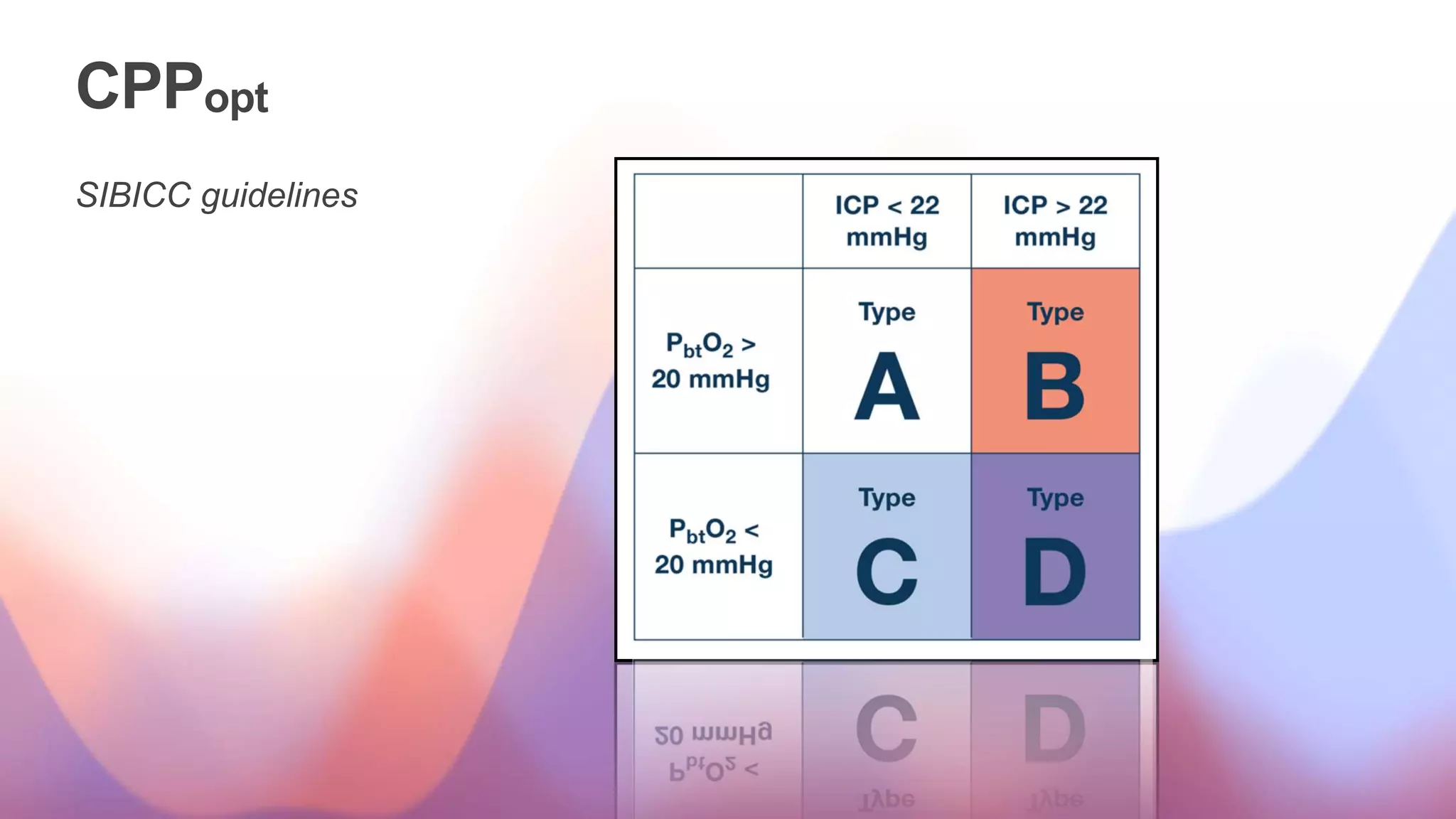
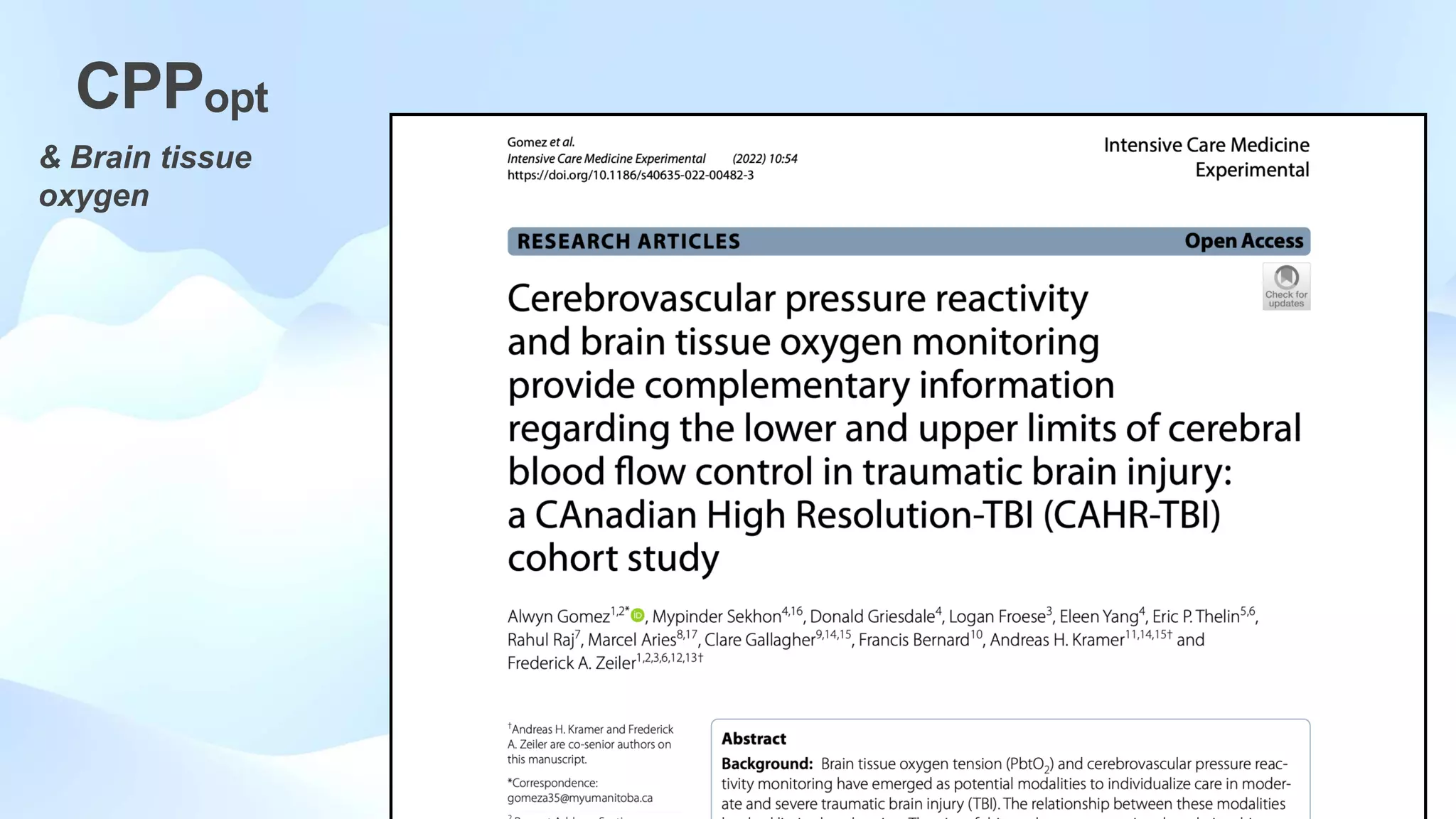
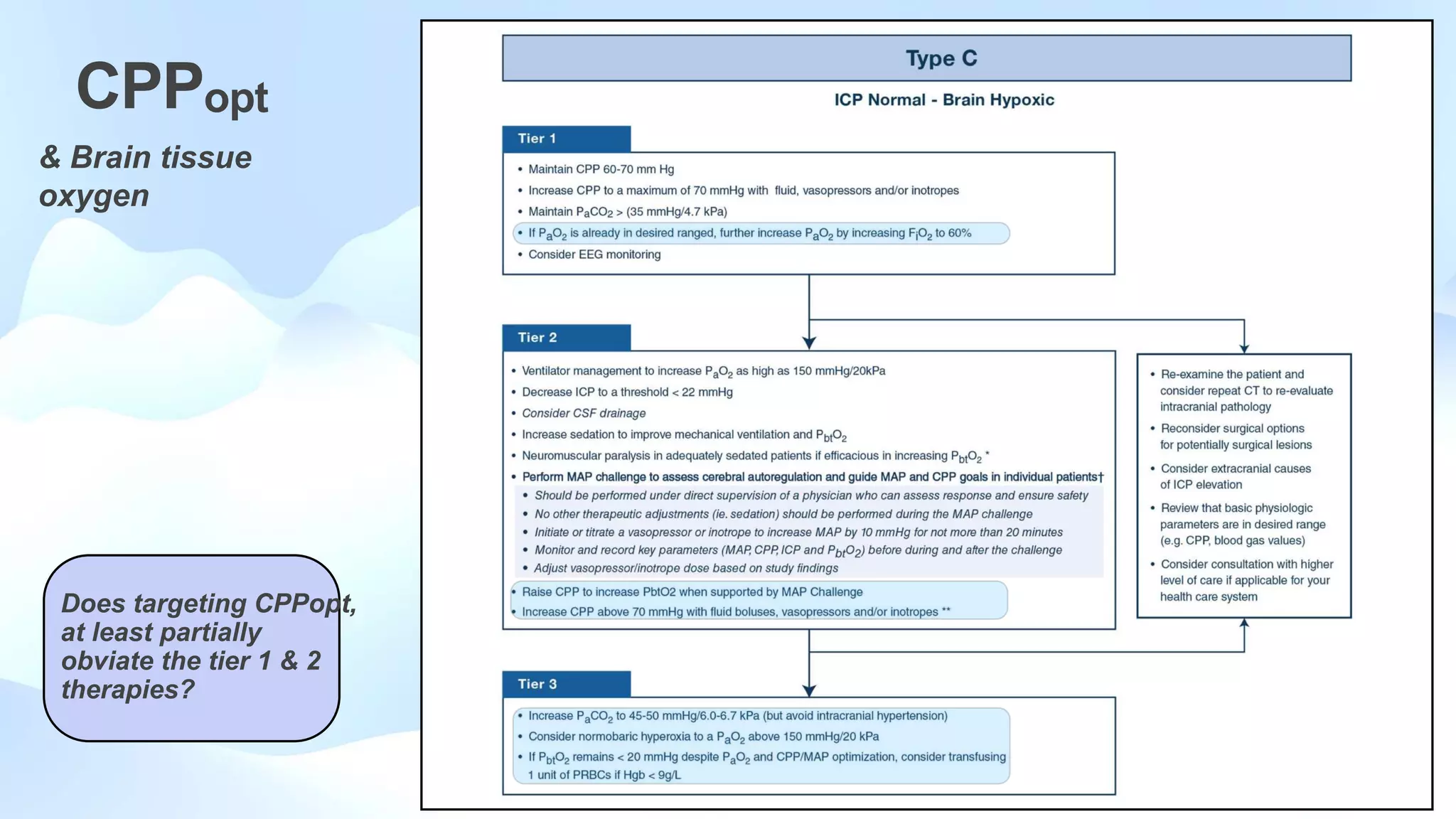
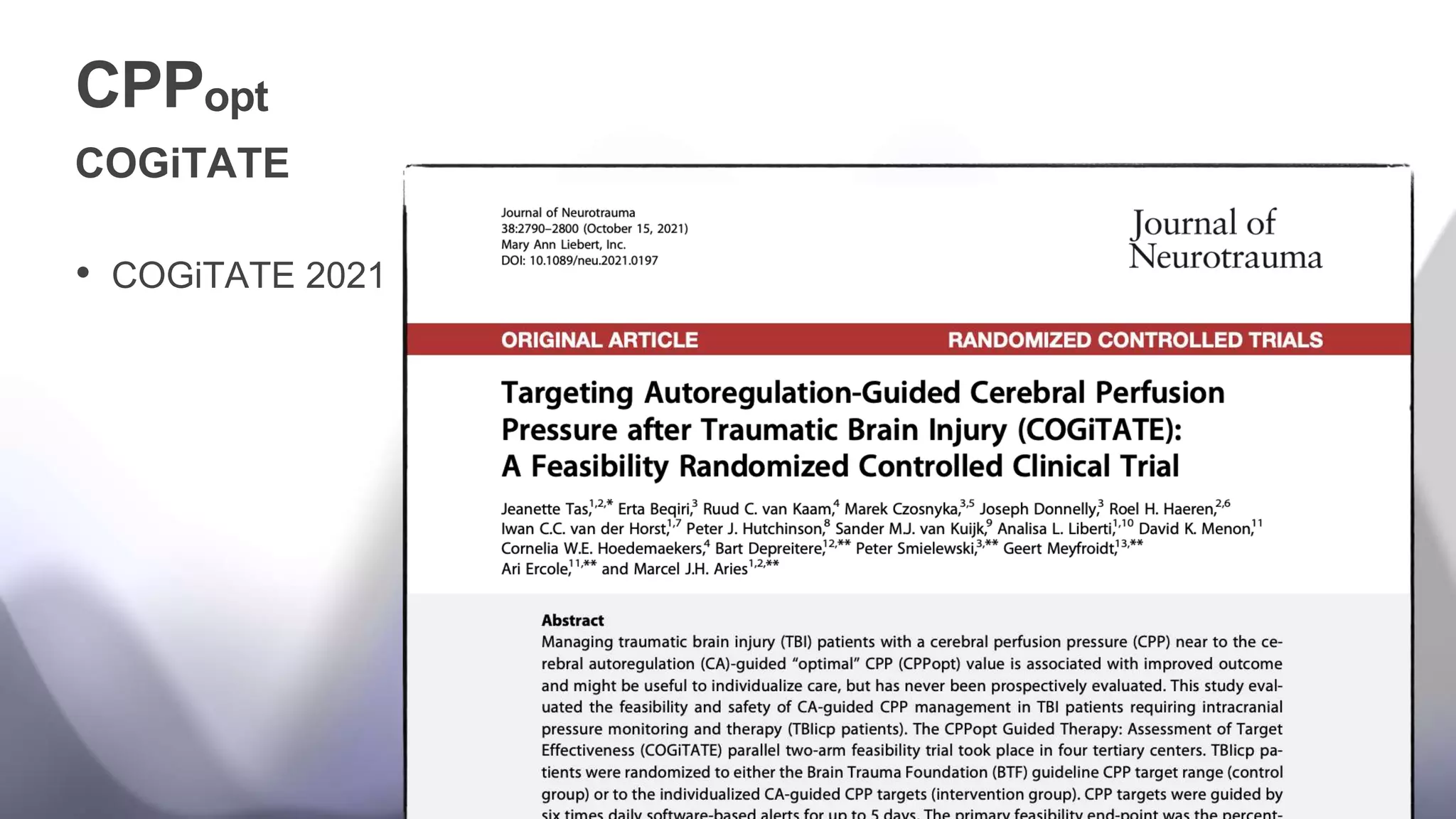
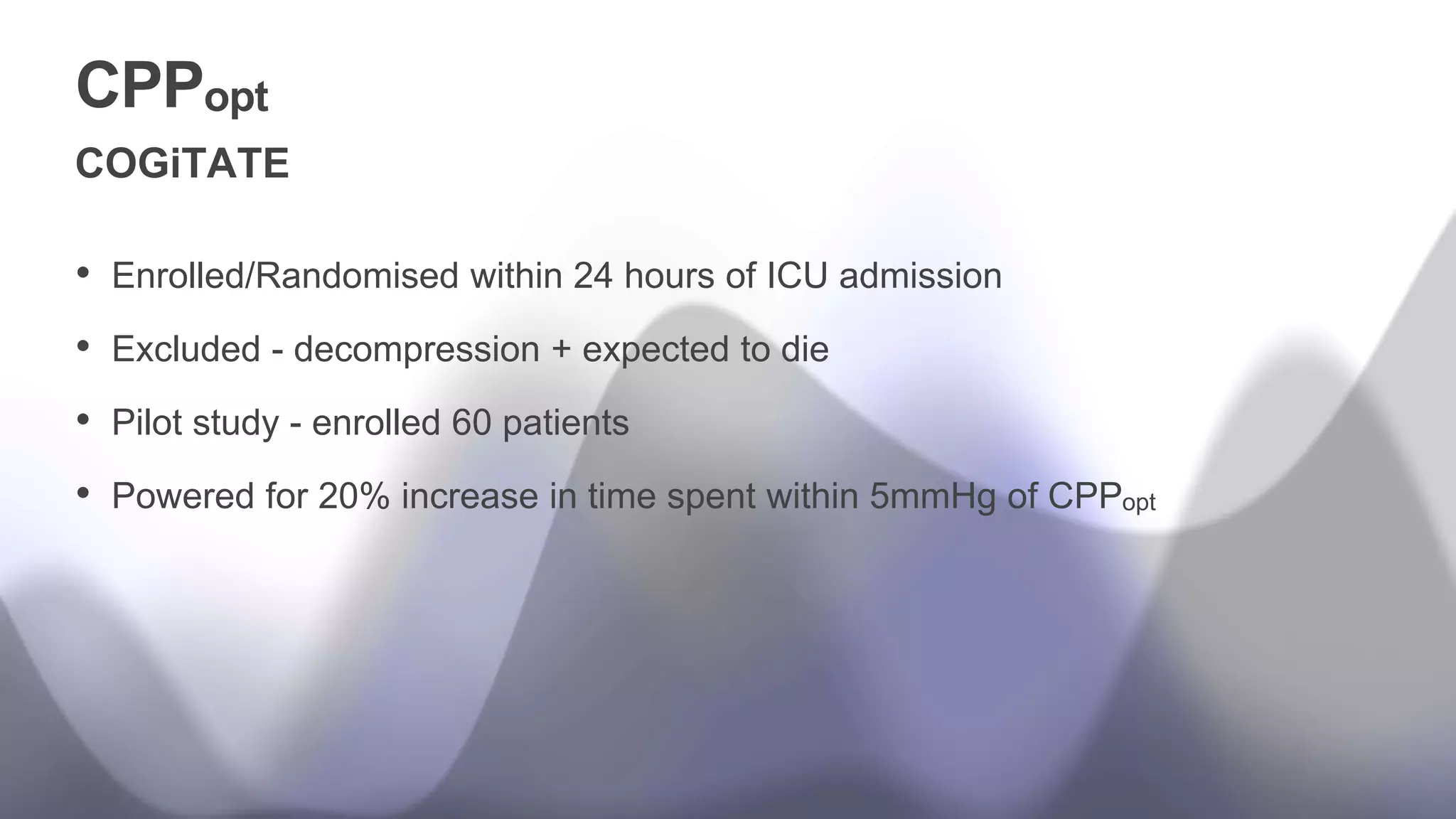
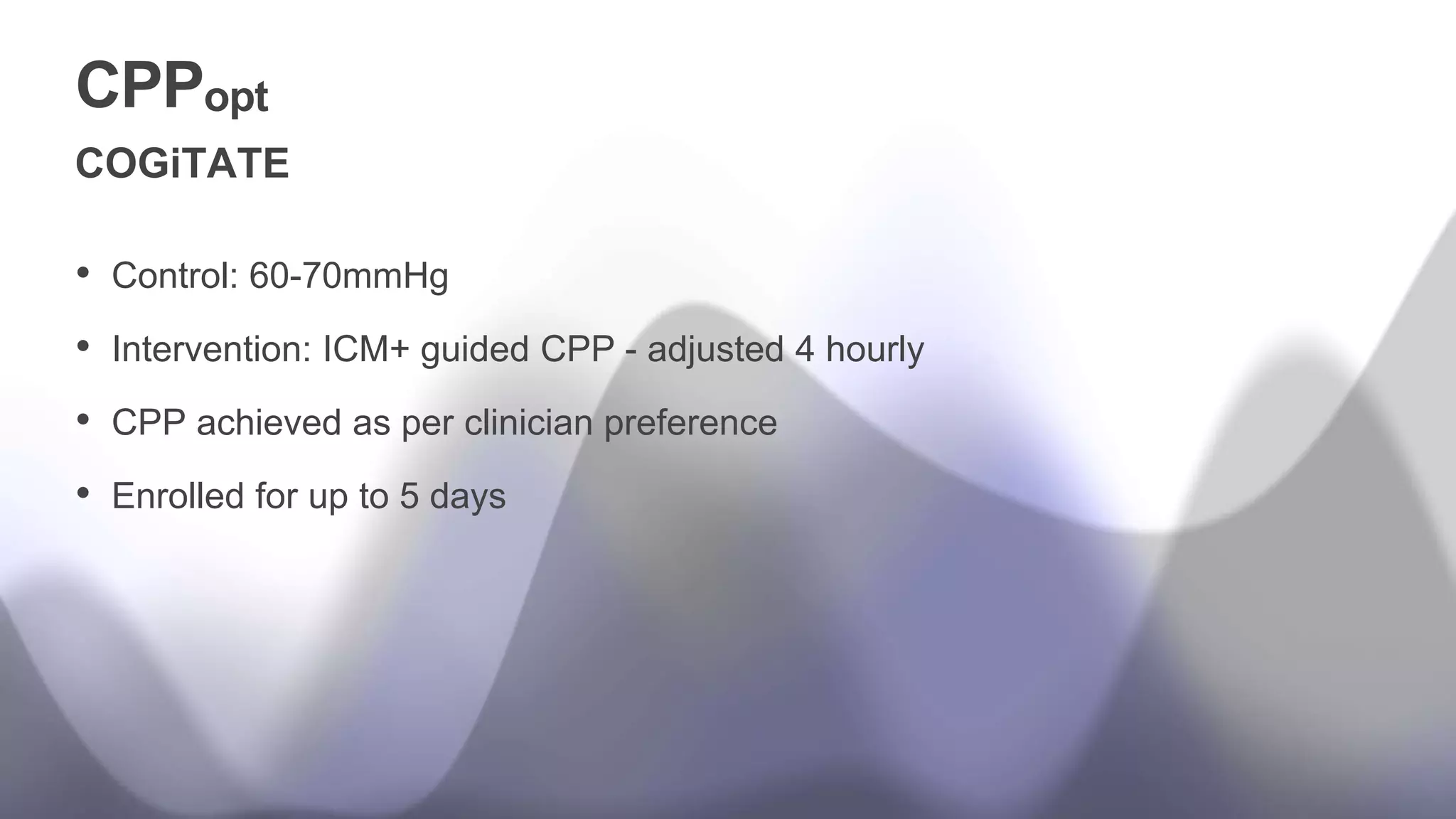
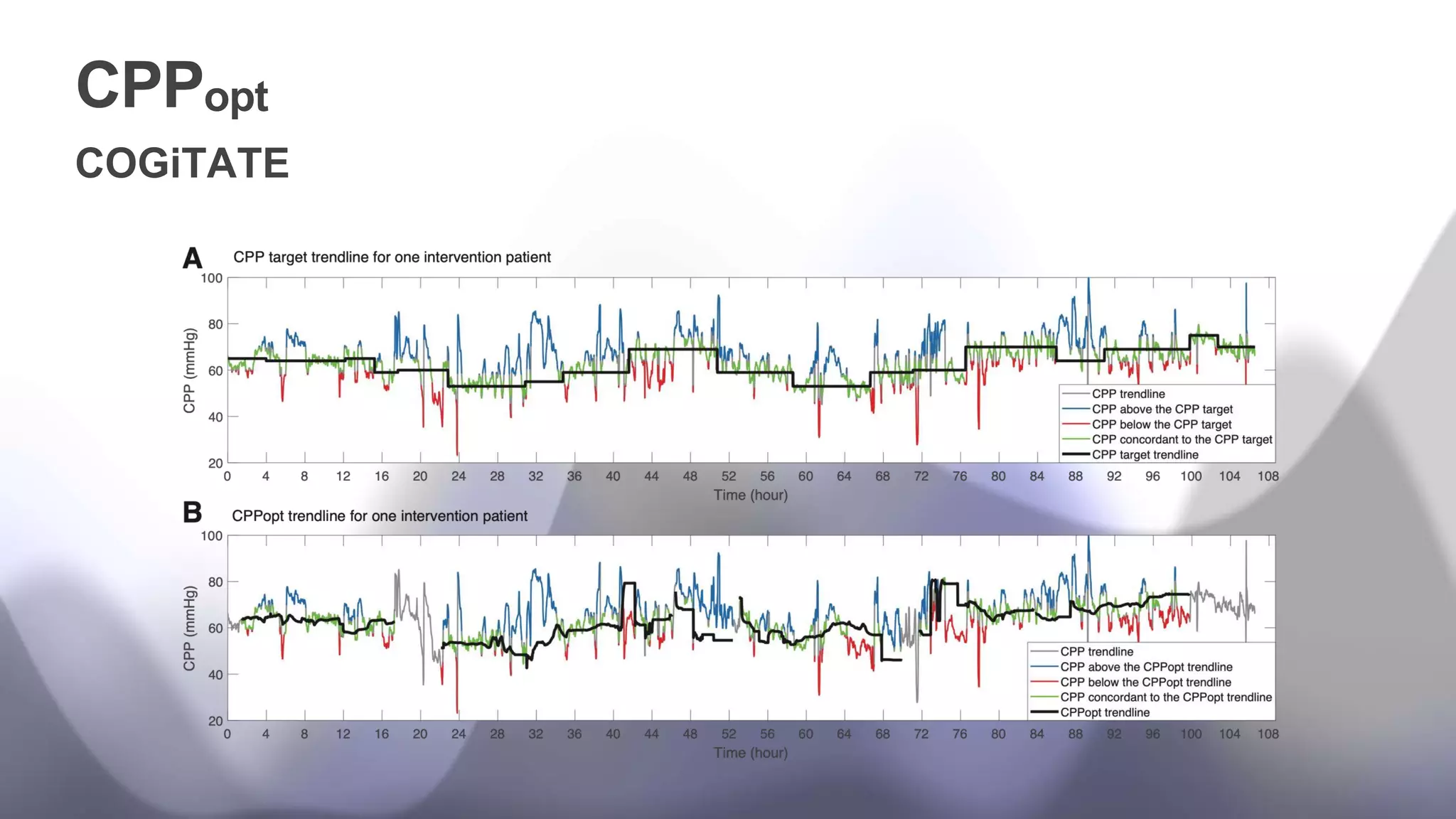
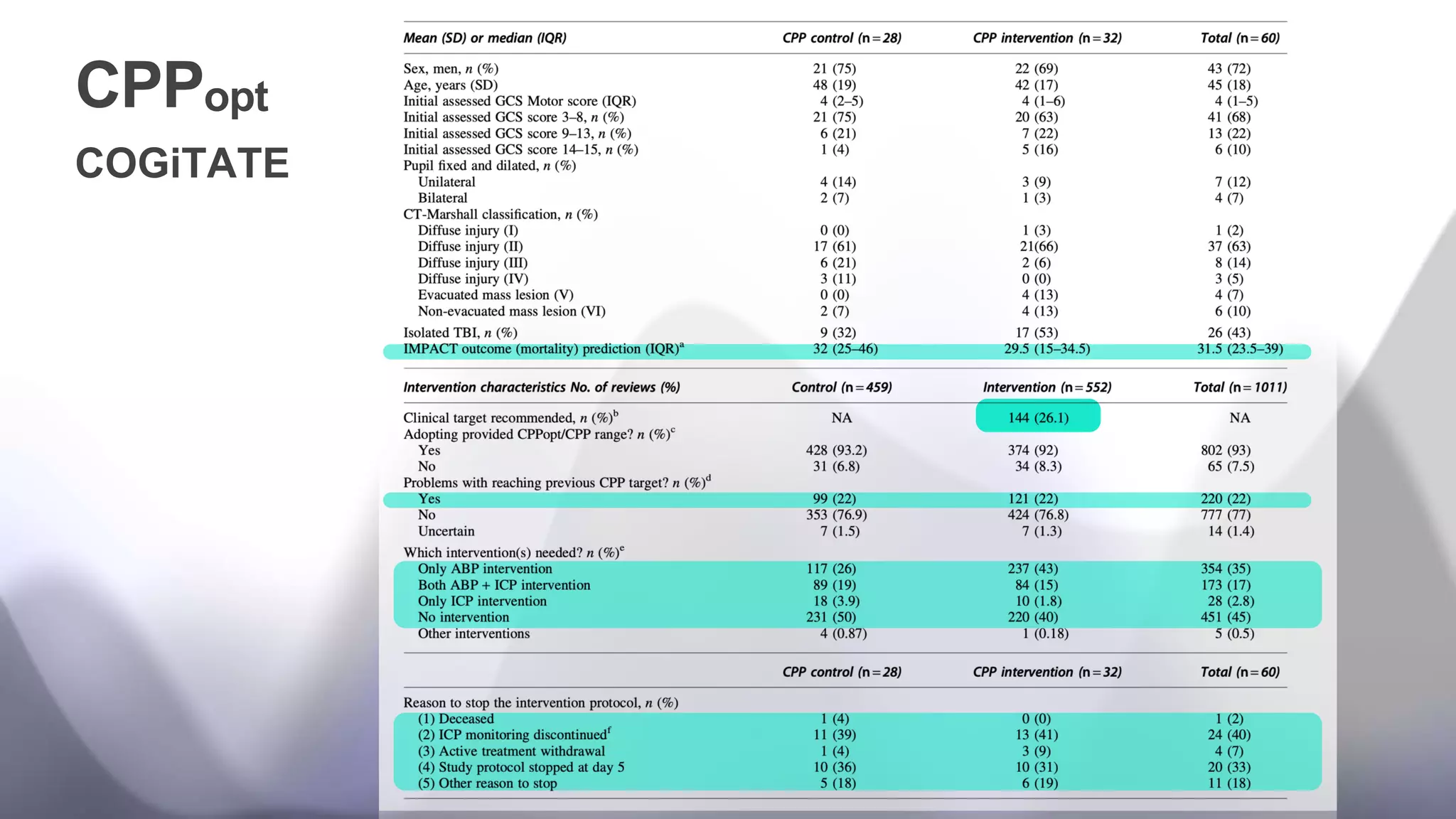
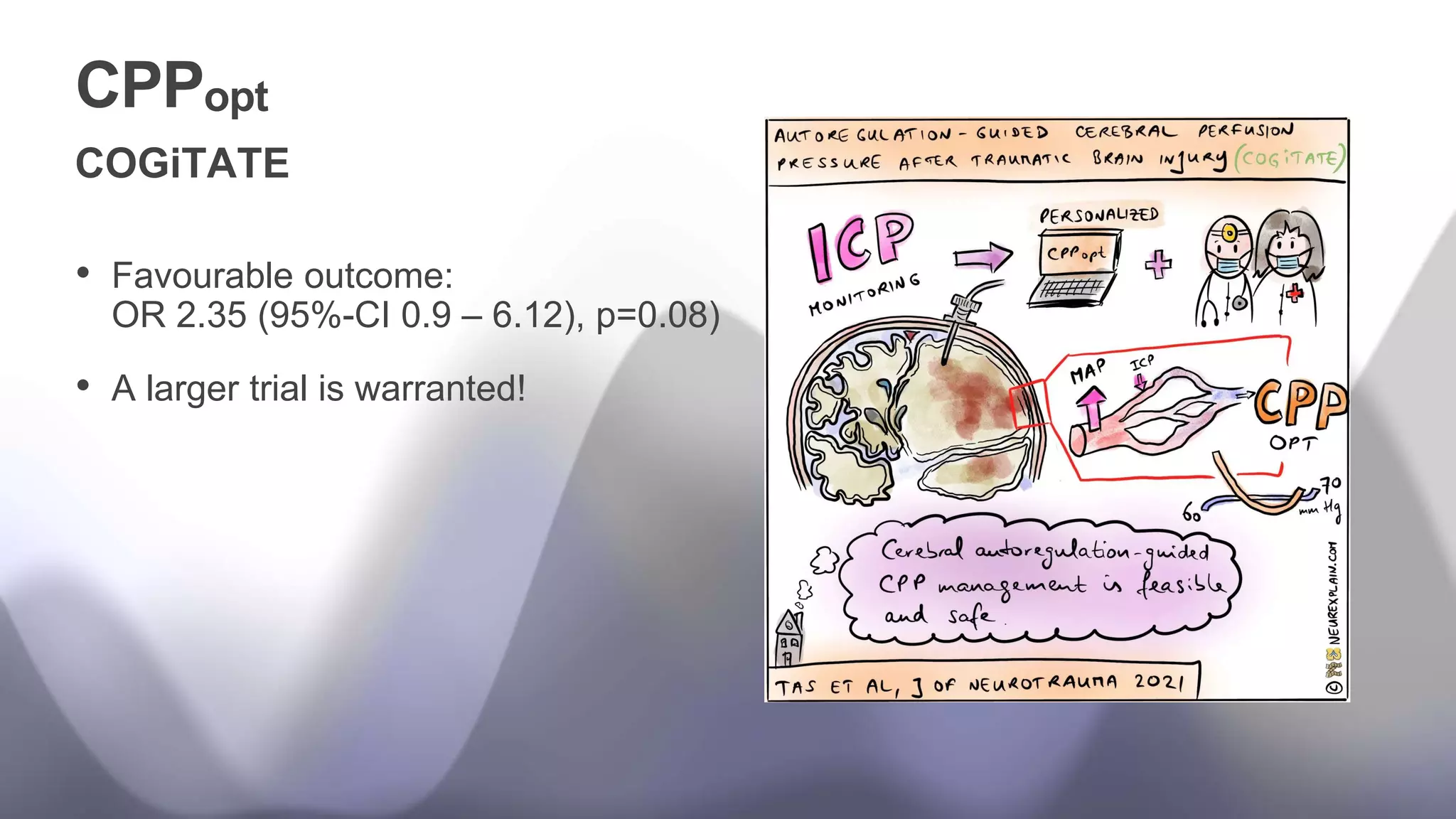
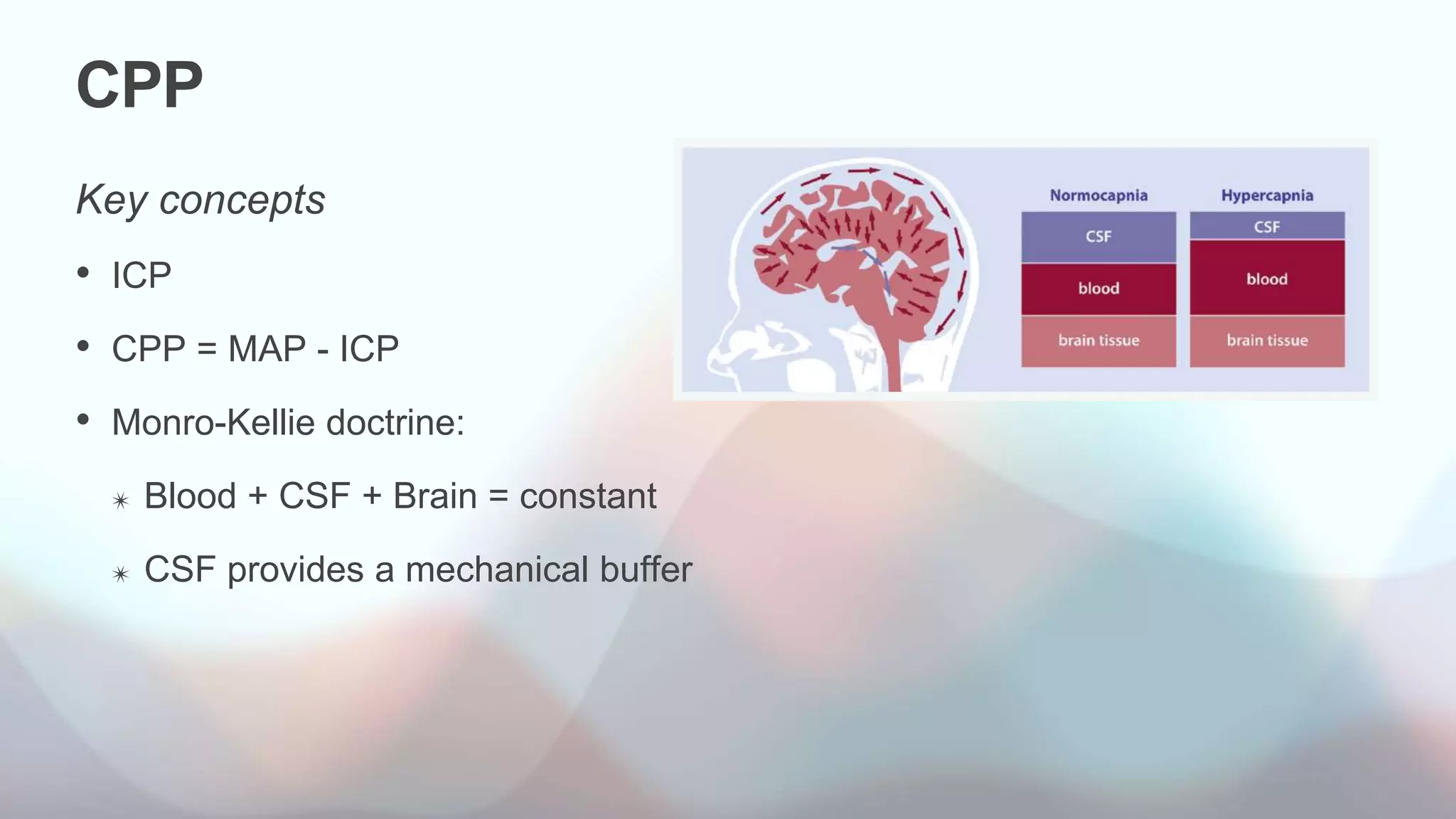
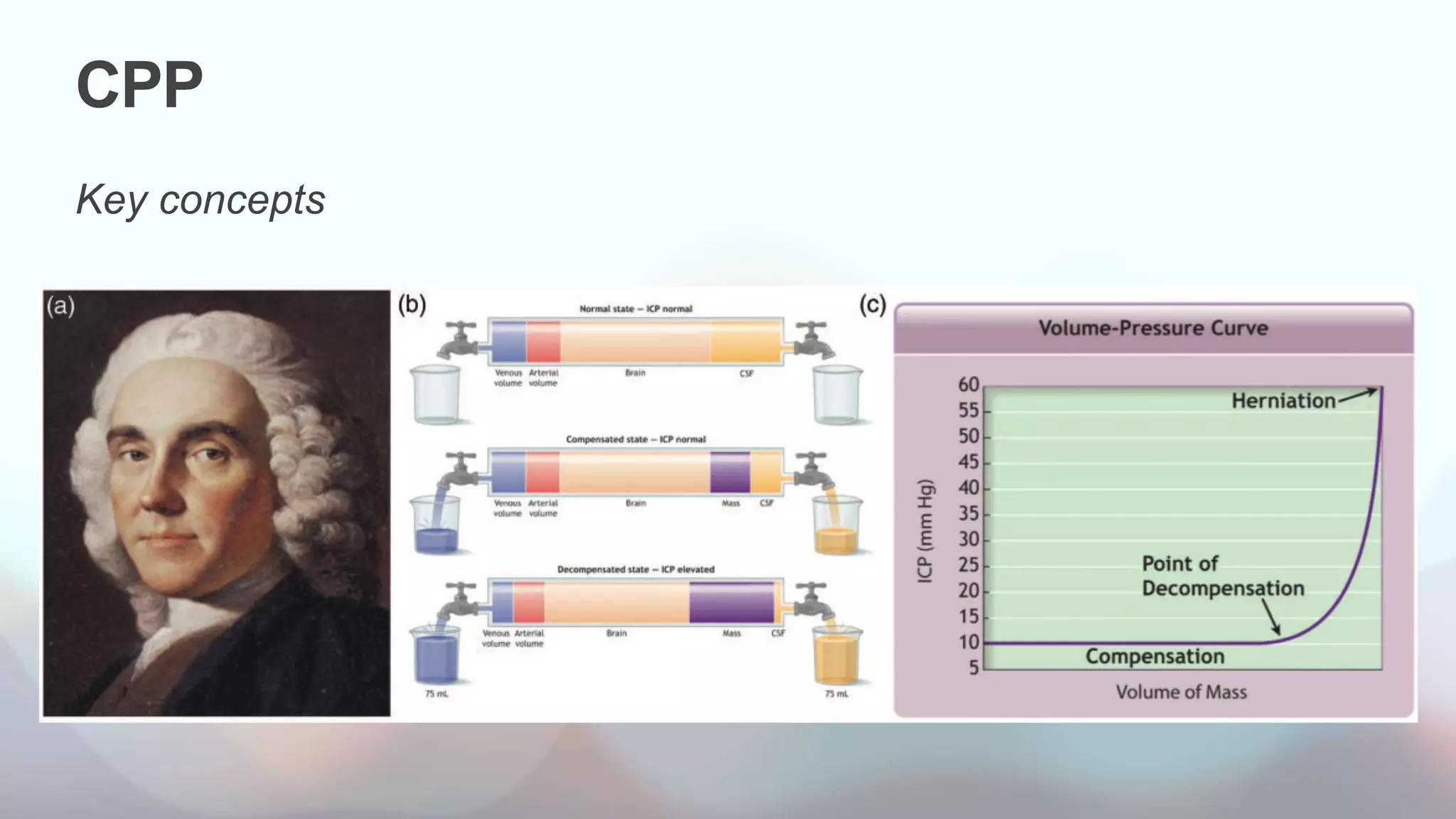
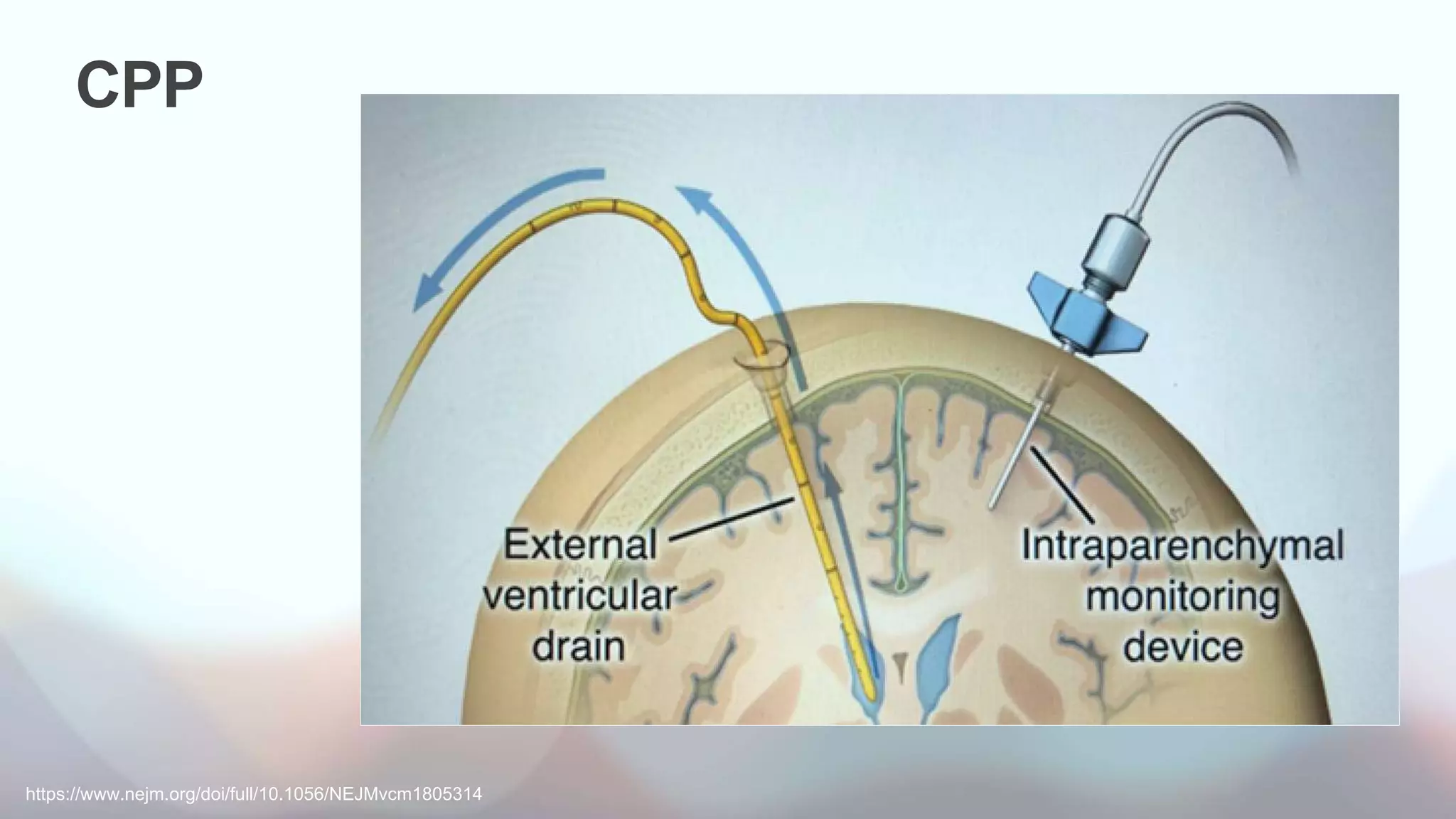
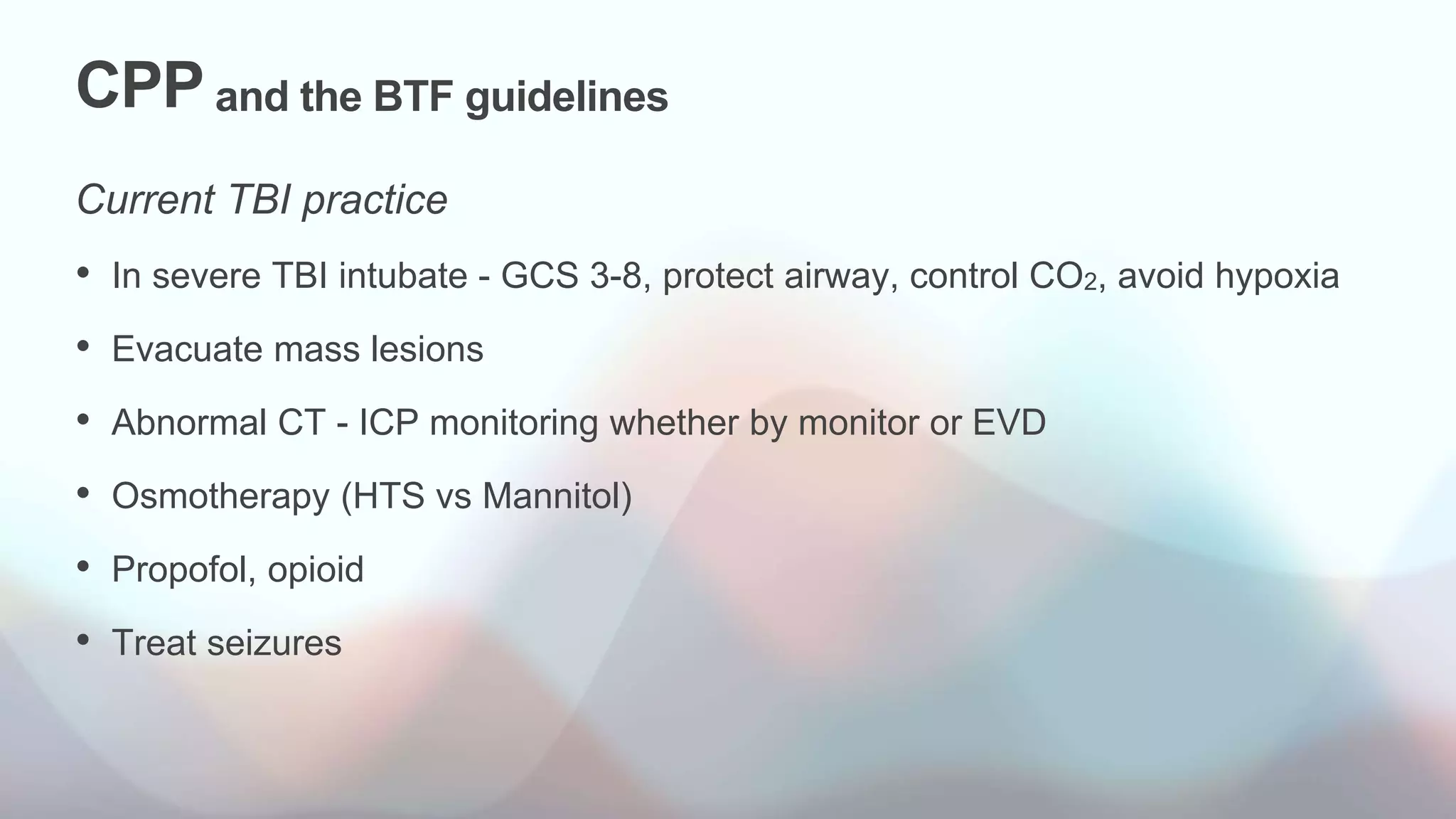
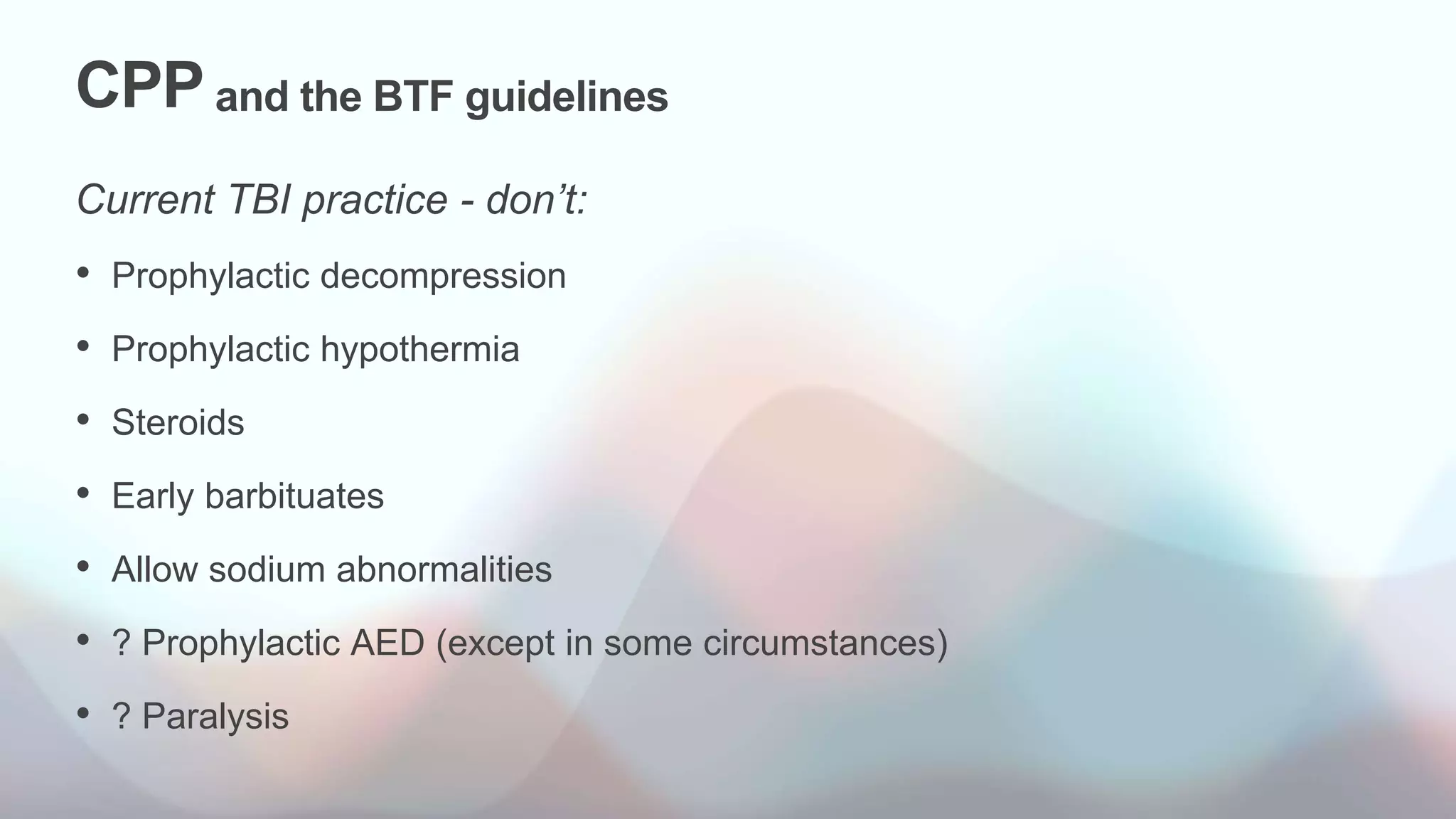
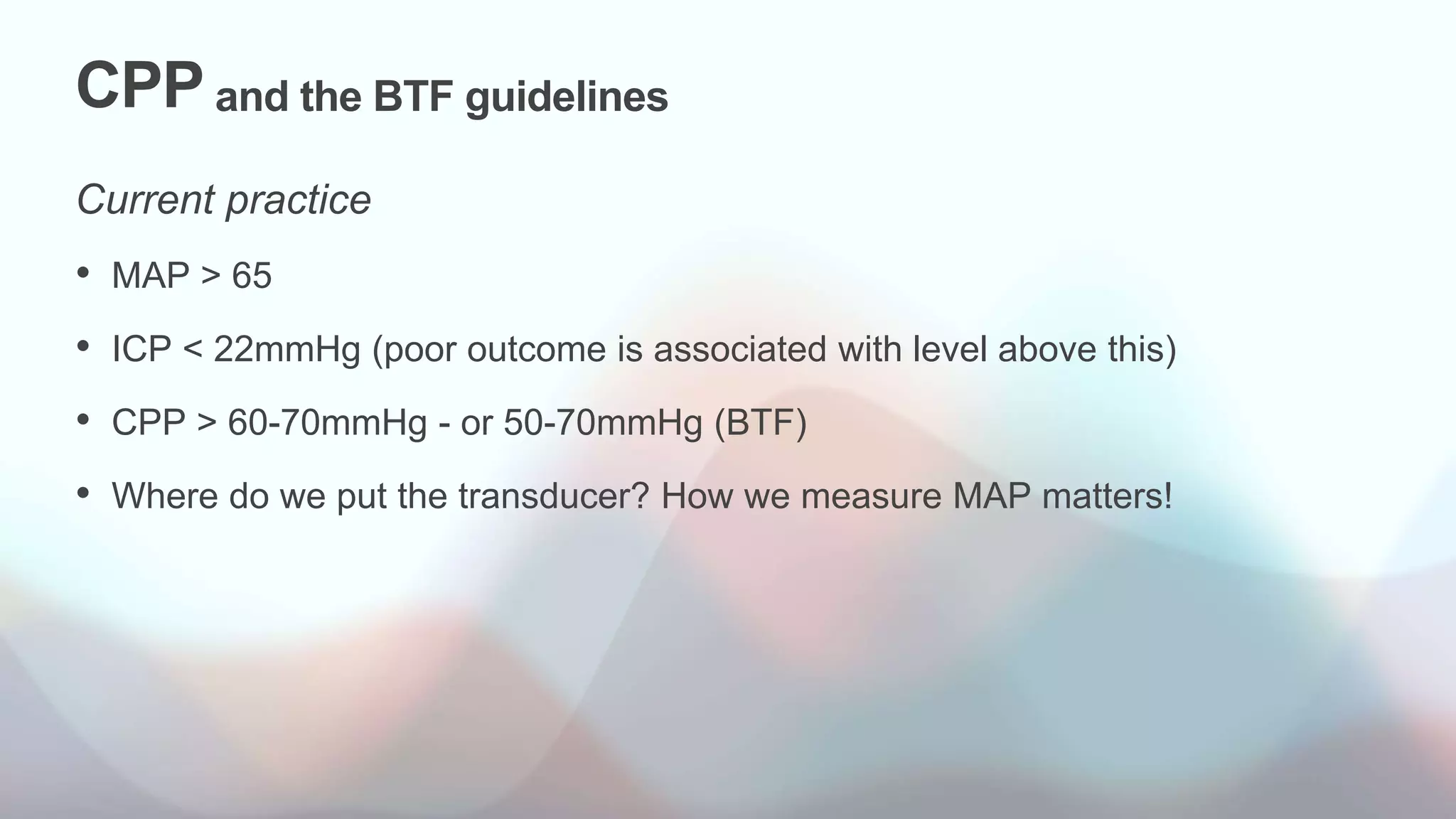
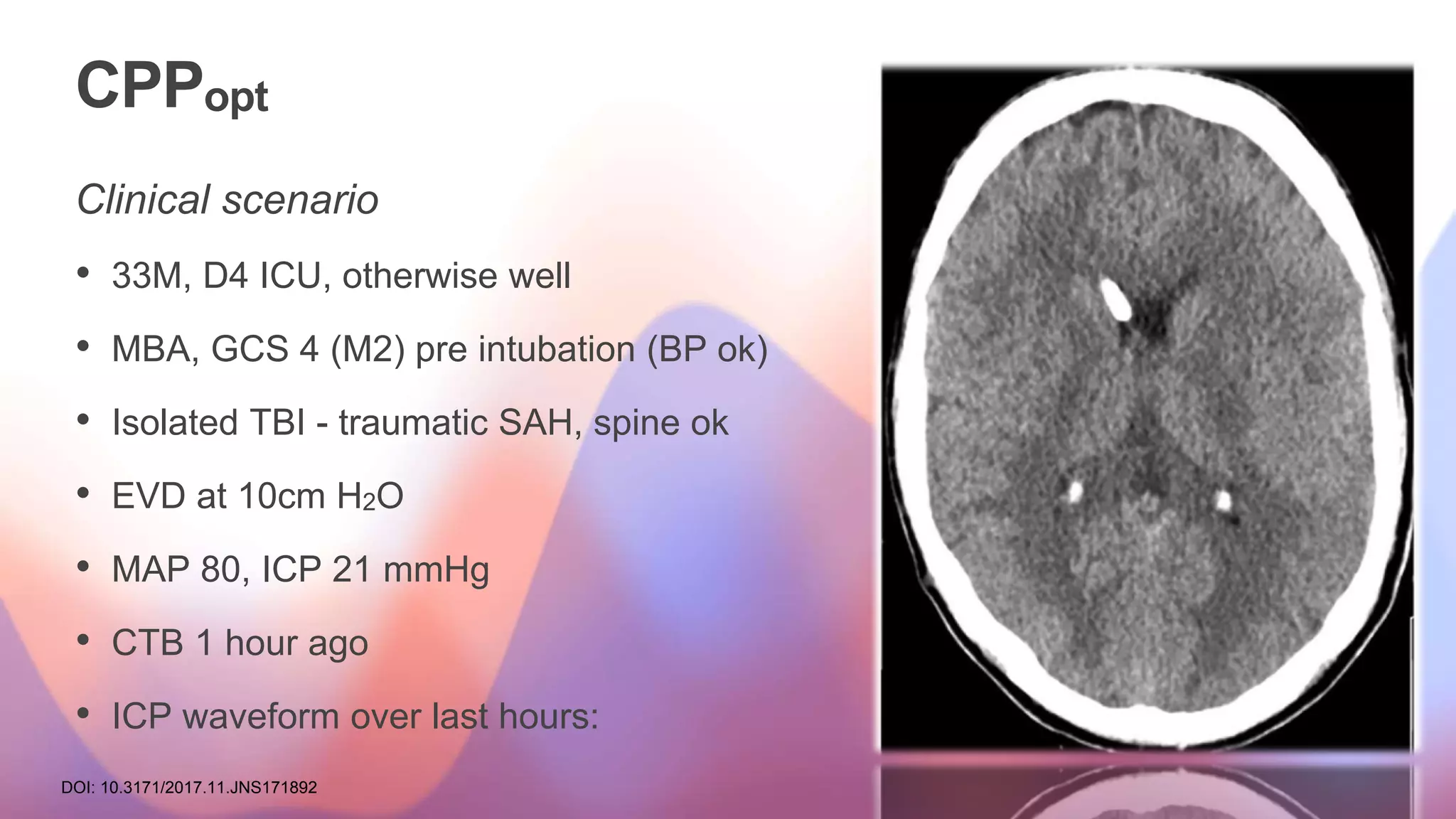
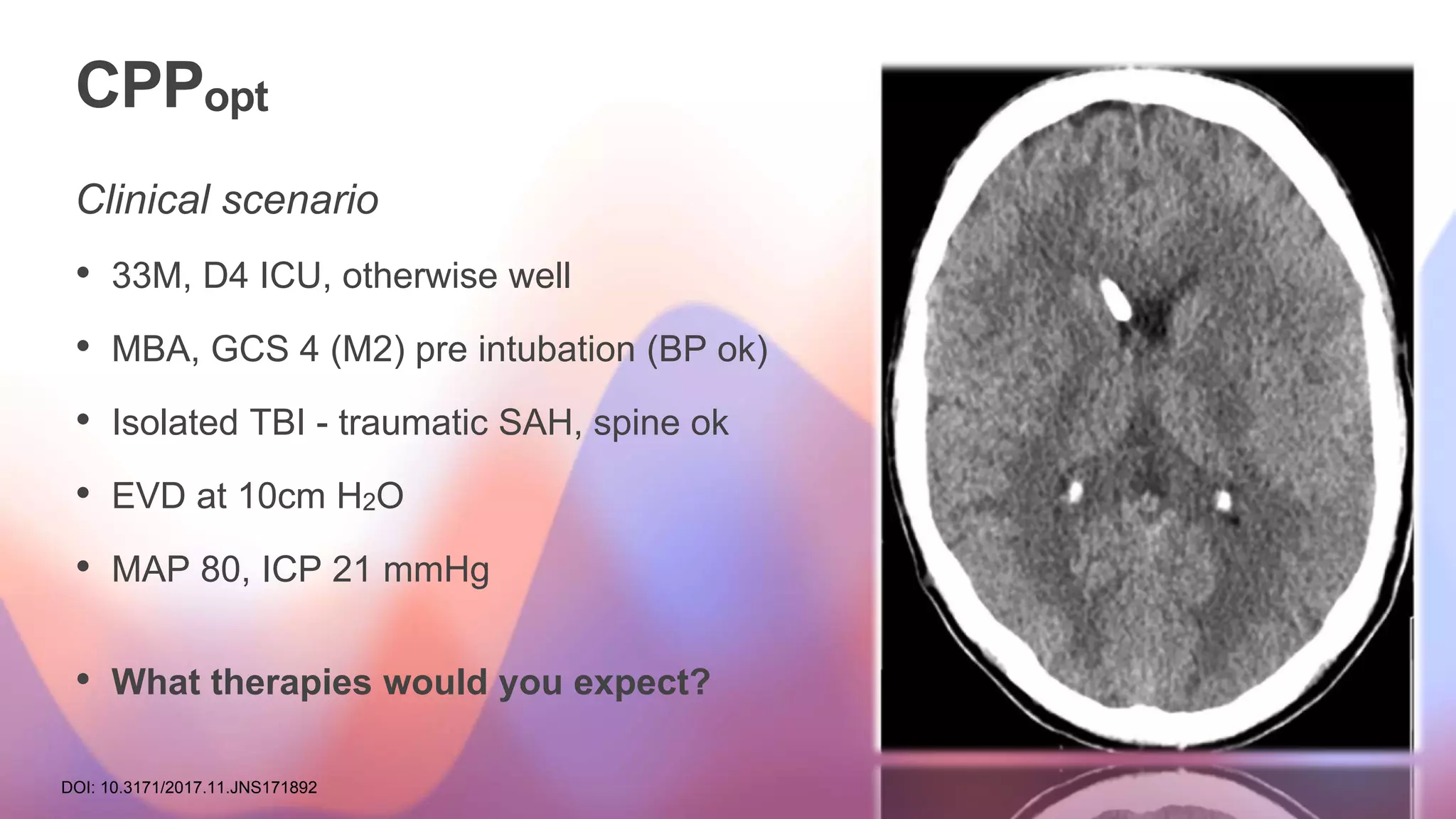
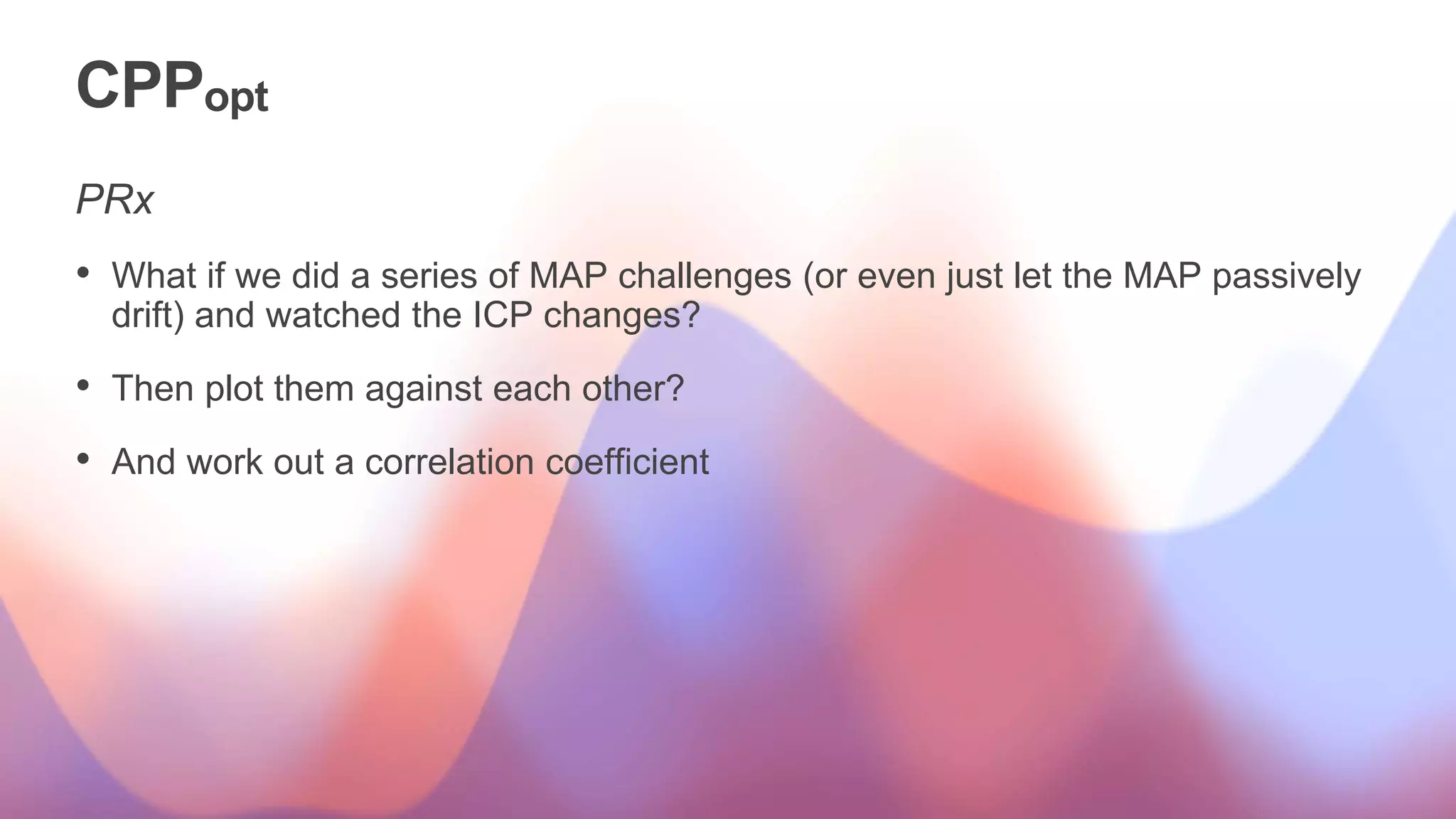
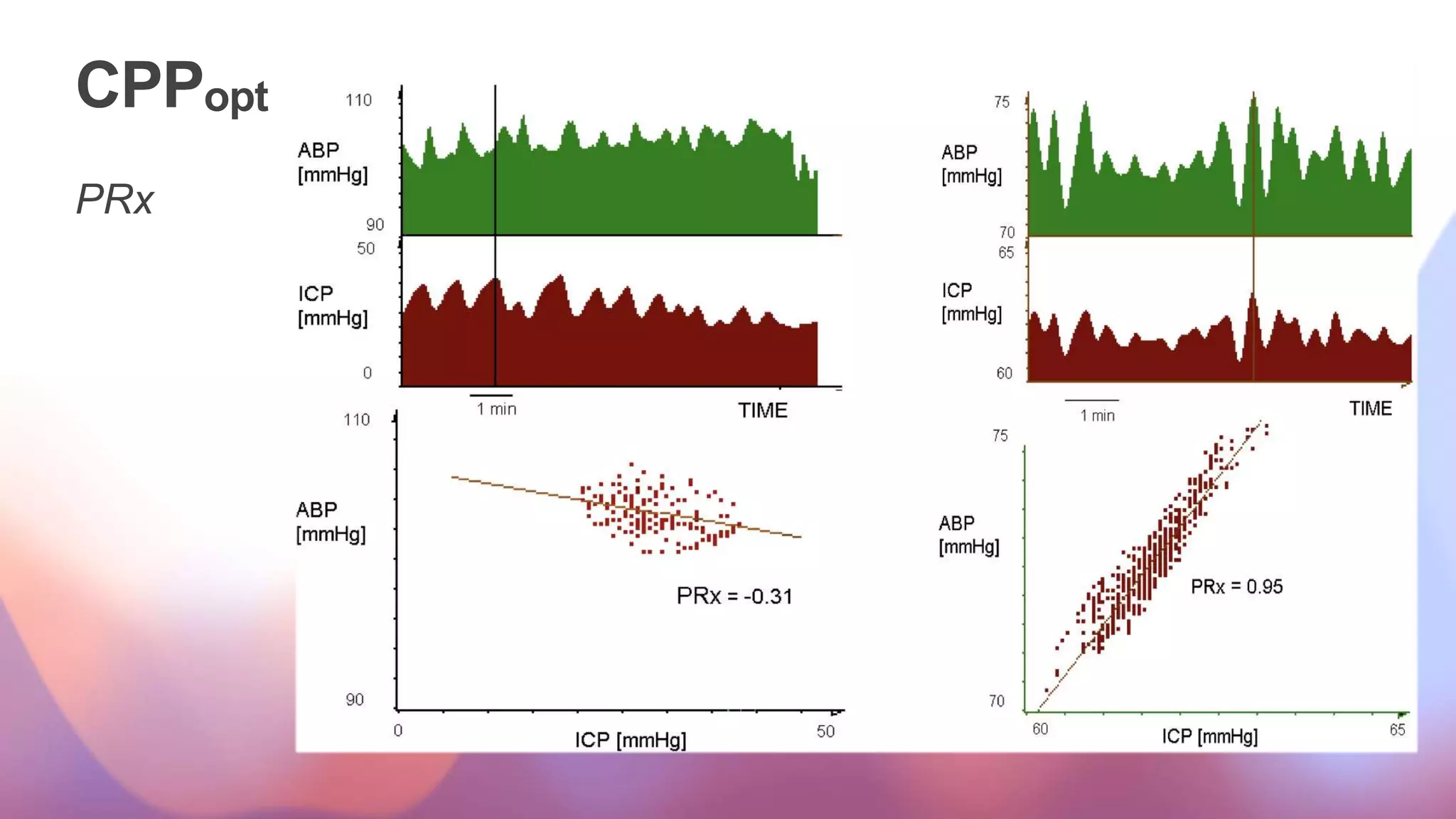
The document discusses key concepts regarding cerebral perfusion pressure (CPP) and intracranial pressure (ICP) management in patients with traumatic brain injury (TBI), following the Brain Trauma Foundation guidelines. It highlights the importance of maintaining specific CPP and ICP levels, the relationship between CPP and ICP, and various treatment options and monitoring techniques, including vasopressor therapy and advanced technology use. The document also emphasizes the need for further research and clinical trials to optimize treatment approaches for TBI patients.


![CPPopt
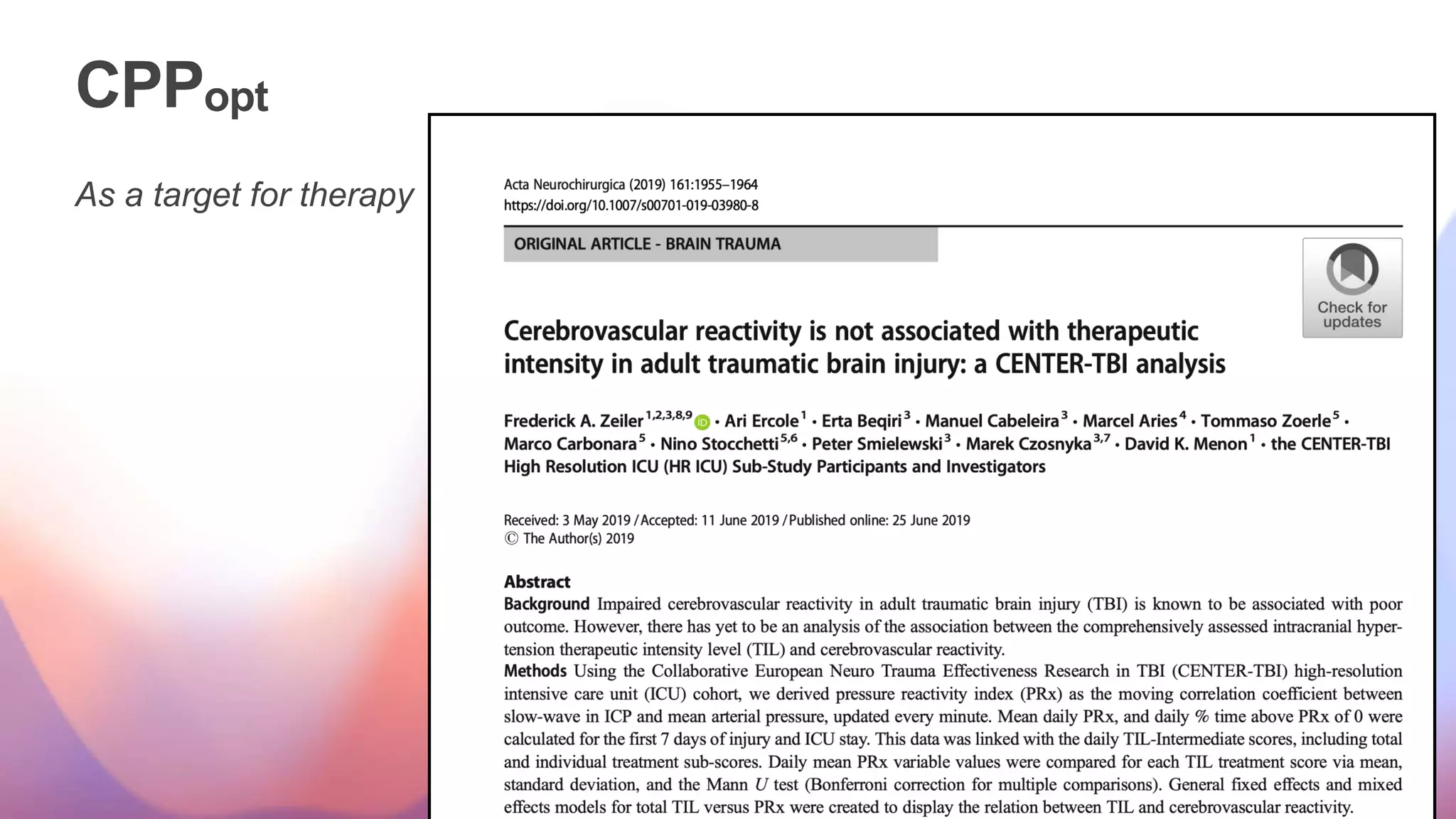
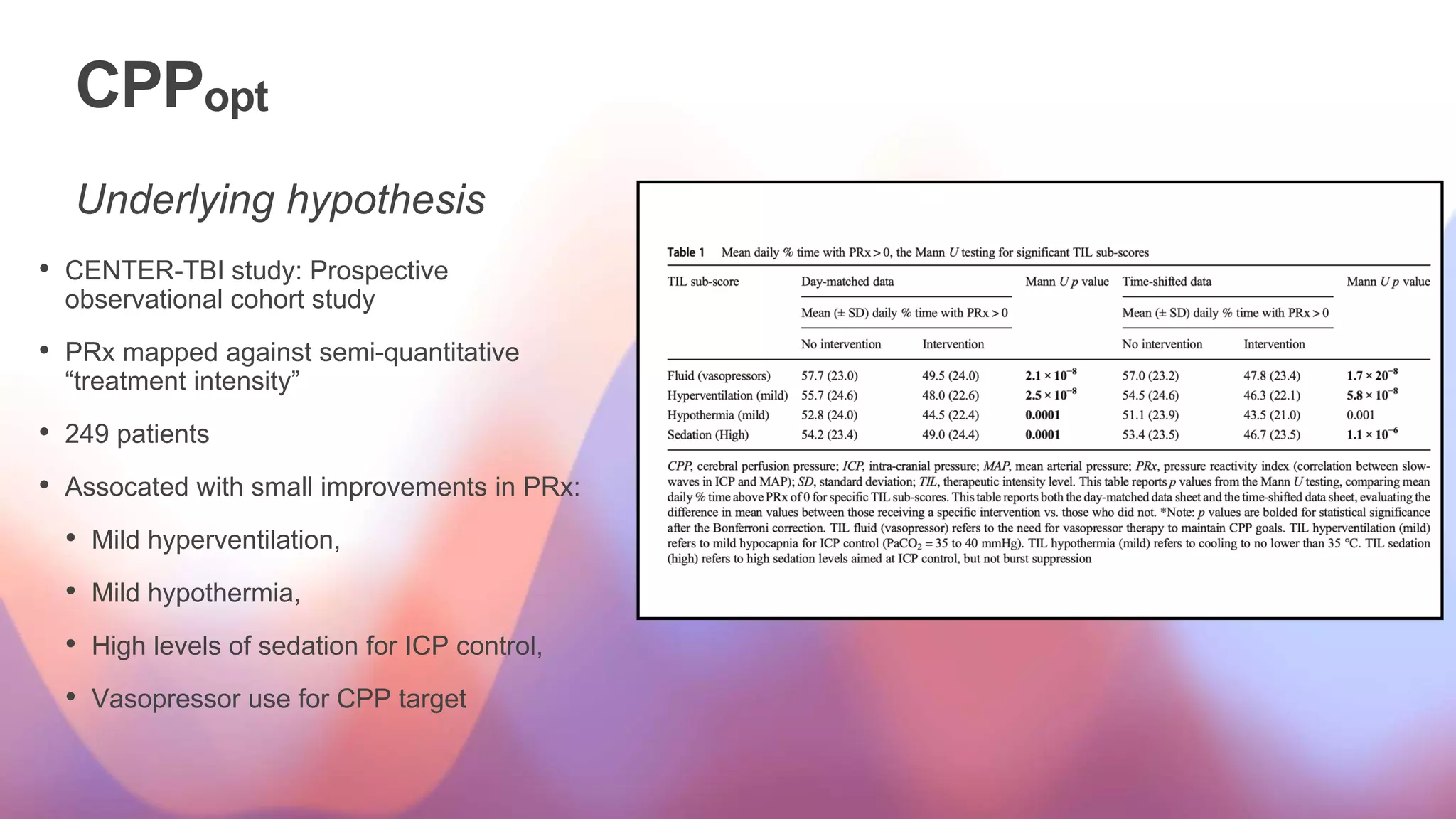
As a target for therapy
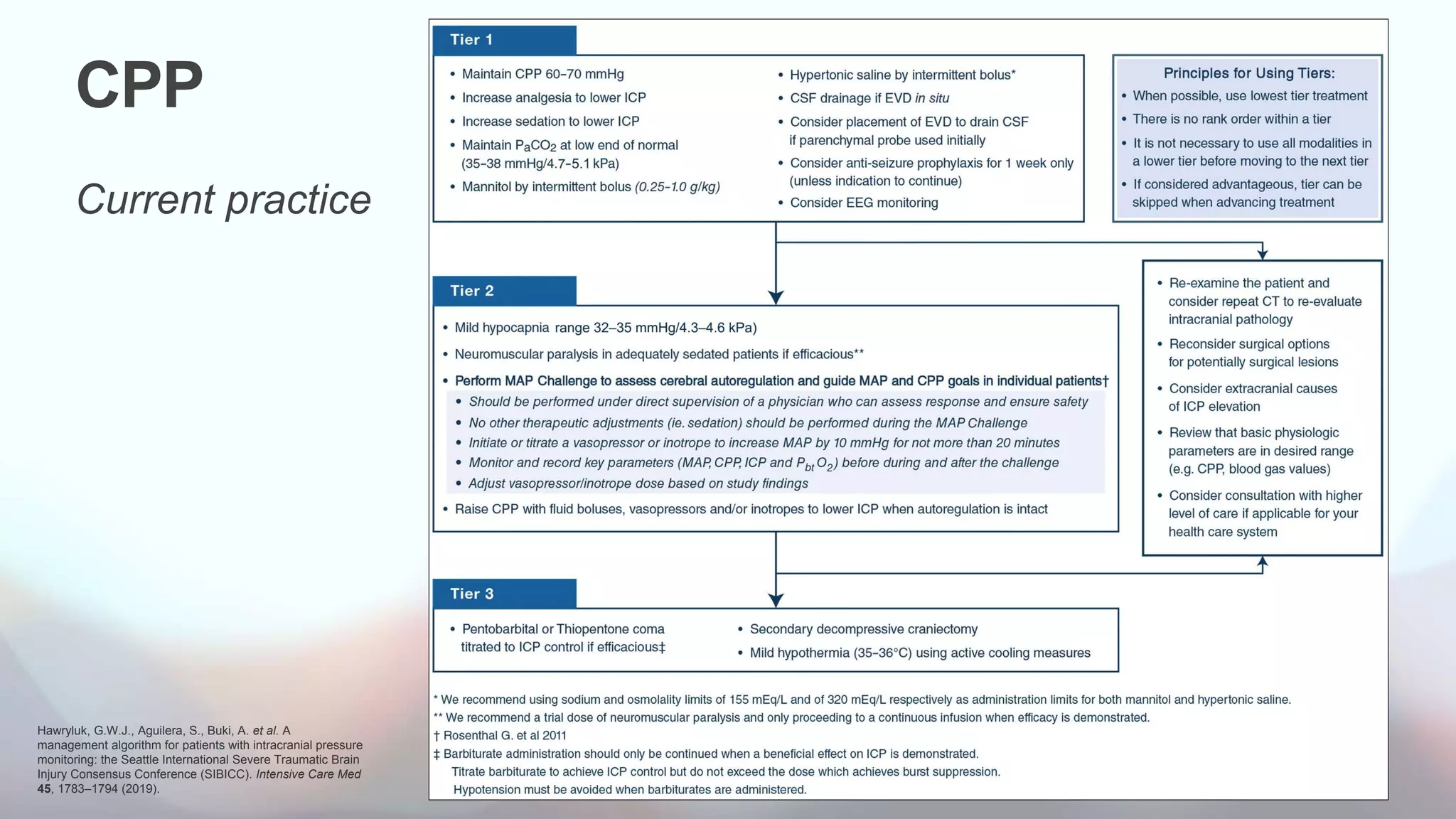
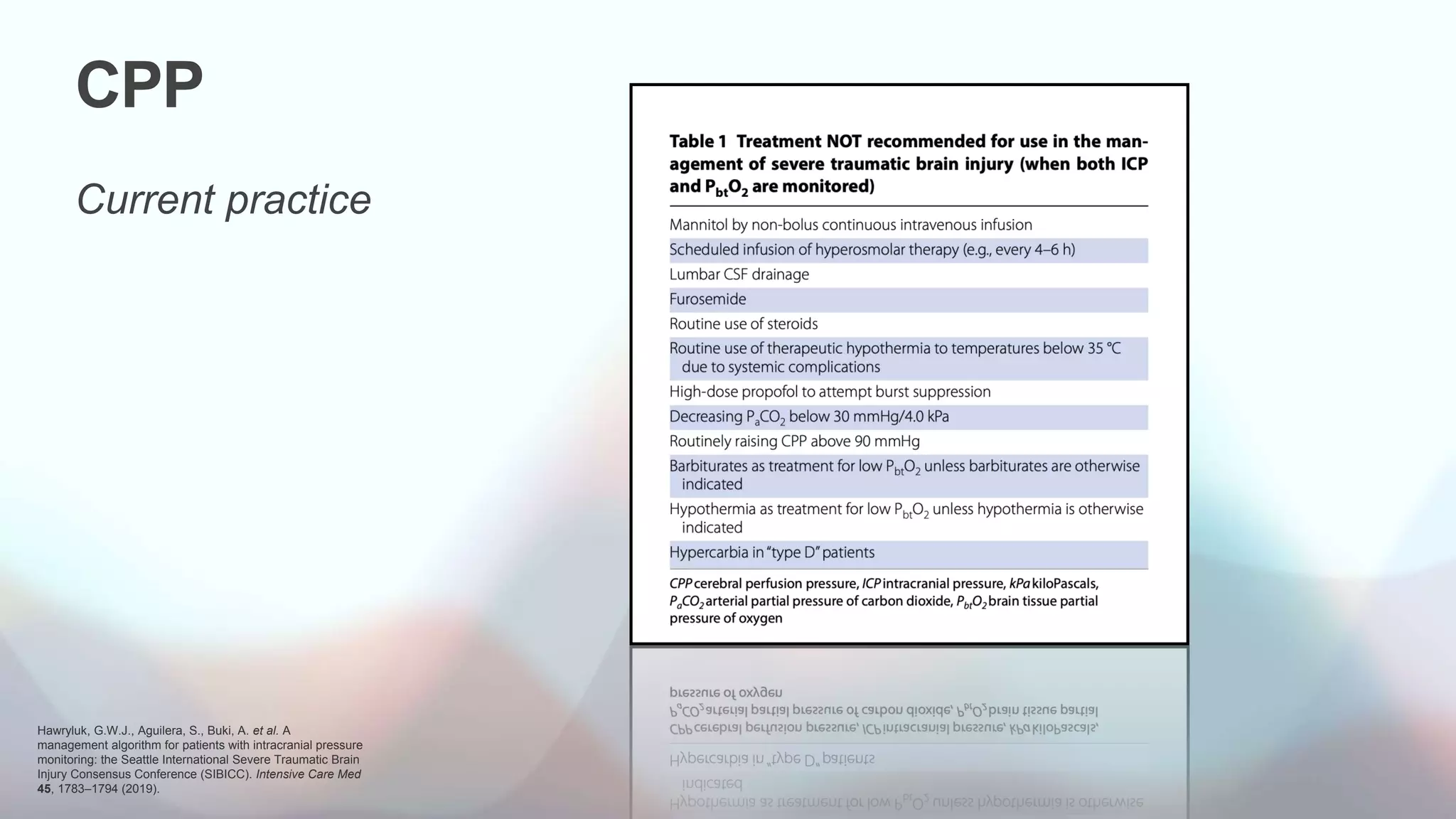
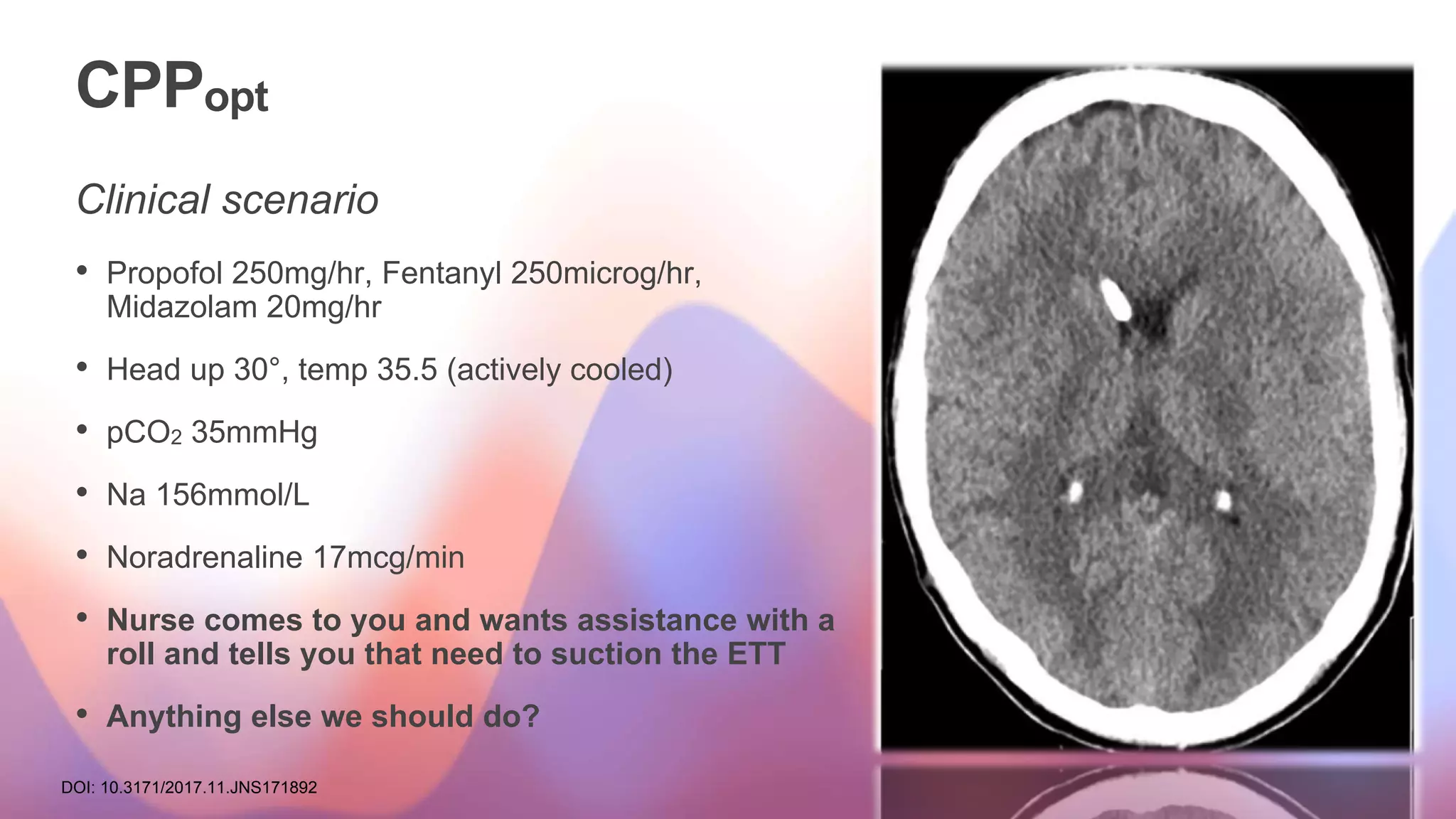
TIL Sub-Category Intervention
Positioning Head elevation for ICP control
Nursed flat (180o) for CPP management
Sedation Level Sedation (low-dose as required for mechanical ventilation)
Higher-dose sedation for ICP control (not aiming for burst suppression)
Metabolic suppression for ICP control with high-dose barbiturates or propofol
NMBA Neuromuscular blockade (paralysis)
CSF Drainage CSF drainage < 120 mL/d (<5 mL/h)
CSF drainage ≤ 120 mL/d (≤5 mL/h)
Fluid/Vasopressor Therapy Fluid loading for maintenance of cerebral perfusion
Vasopressor therapy required for management of cerebral perfusion
Hyperventilation Mild hypocapnia for ICP control (PaCO2 4.6–5.3 kPa [35–40 mm Hg])
Moderate hypocapnia for ICP control (PaCO2 ≤ 4 kPa [30 mm Hg])
Intensive hypocapnia for ICP control (PaCO2 < 4 kPa [30 mm Hg])
Hyperosmolar Therapy Hyperosmolar therapy with mannitol up to 2 gm/kg/24 h
Hyperosmolar therapy with hypertonic saline up to 0.3 gm/kg/24 h
Hyperosmolar therapy with mannitol > 2 gm/kg/24 h
Hyperosmolar therapy with hypertonic saline > 0.3 gm/kg/24 h
Temperature Management Treatment of fever (>38C) or spontaneous temperature of 34.5C
Mild hypothermia for ICP control with a lower limit of 35C
Hypothermia below 35C
Surgery for ICP Control Intracranial operation for progressive mass lesion, not scheduled on admission
Decompressive craniectomy](https://image.slidesharecdn.com/cppopt-redux-230711064757-7069f5ad/75/Optimal-Cerebral-Perfusion-Pressure-40-2048.jpg)
![CPPopt
As a target for therapy
TIL Sub-Category Intervention
Positioning Head elevation for ICP control
Nursed flat (180o) for CPP management
Sedation Level Sedation (low-dose as required for mechanical ventilation)
Higher-dose sedation for ICP control (not aiming for burst suppression)
Metabolic suppression for ICP control with high-dose barbiturates or propofol
NMBA Neuromuscular blockade (paralysis)
CSF Drainage CSF drainage < 120 mL/d (<5 mL/h)
CSF drainage ≤ 120 mL/d (≤5 mL/h)
Fluid/Vasopressor Therapy Fluid loading for maintenance of cerebral perfusion
Vasopressor therapy required for management of cerebral perfusion
Hyperventilation Mild hypocapnia for ICP control (PaCO2 4.6–5.3 kPa [35–40 mm Hg])
Moderate hypocapnia for ICP control (PaCO2 ≤ 4 kPa [30 mm Hg])
Intensive hypocapnia for ICP control (PaCO2 < 4 kPa [30 mm Hg])
Hyperosmolar Therapy Hyperosmolar therapy with mannitol up to 2 gm/kg/24 h
Hyperosmolar therapy with hypertonic saline up to 0.3 gm/kg/24 h
Hyperosmolar therapy with mannitol > 2 gm/kg/24 h
Hyperosmolar therapy with hypertonic saline > 0.3 gm/kg/24 h
Temperature Management Treatment of fever (>38C) or spontaneous temperature of 34.5C
Mild hypothermia for ICP control with a lower limit of 35C
Hypothermia below 35C
Surgery for ICP Control Intracranial operation for progressive mass lesion, not scheduled on admission
Decompressive craniectomy](https://image.slidesharecdn.com/cppopt-redux-230711064757-7069f5ad/75/Optimal-Cerebral-Perfusion-Pressure-43-2048.jpg)