Embed presentation
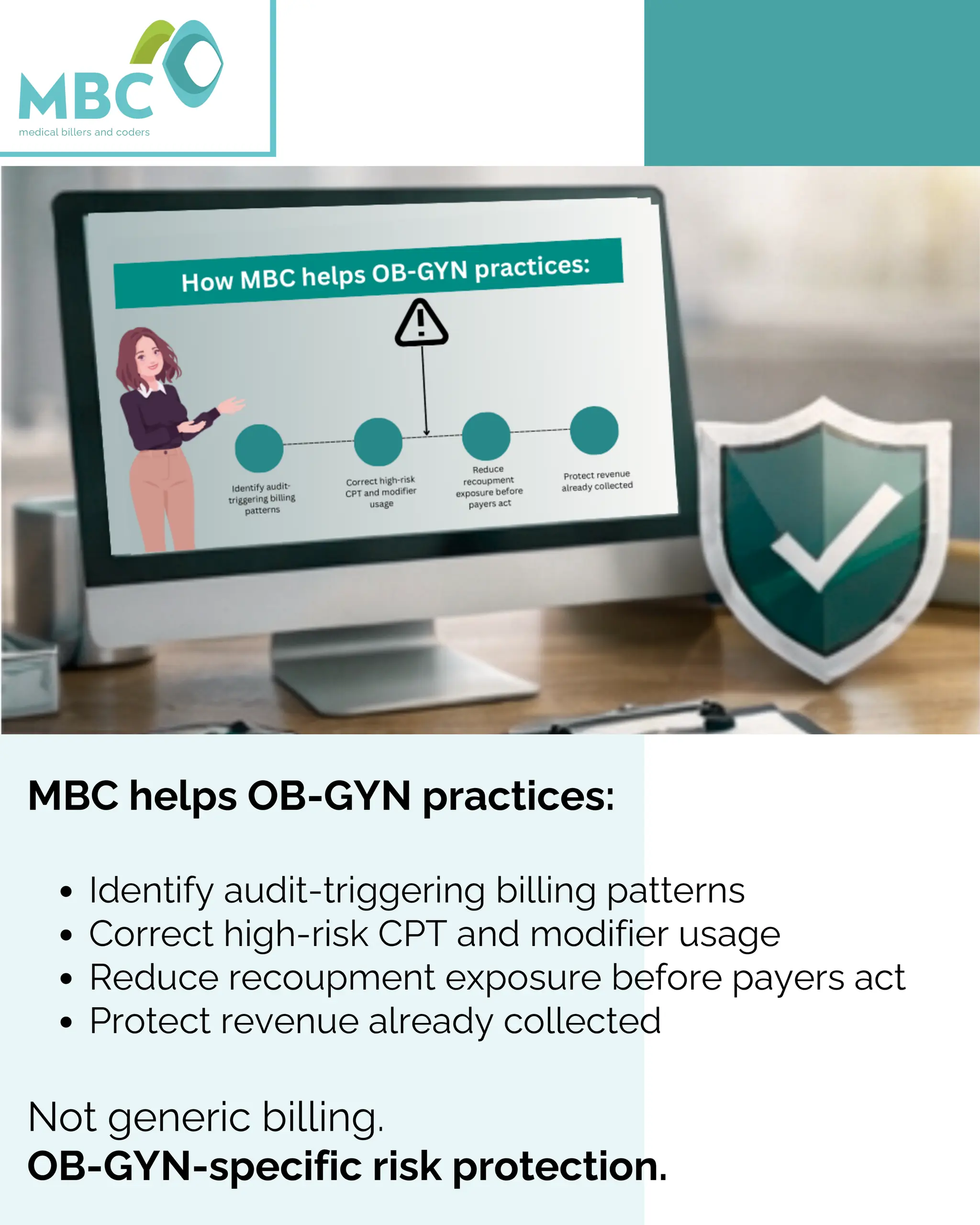
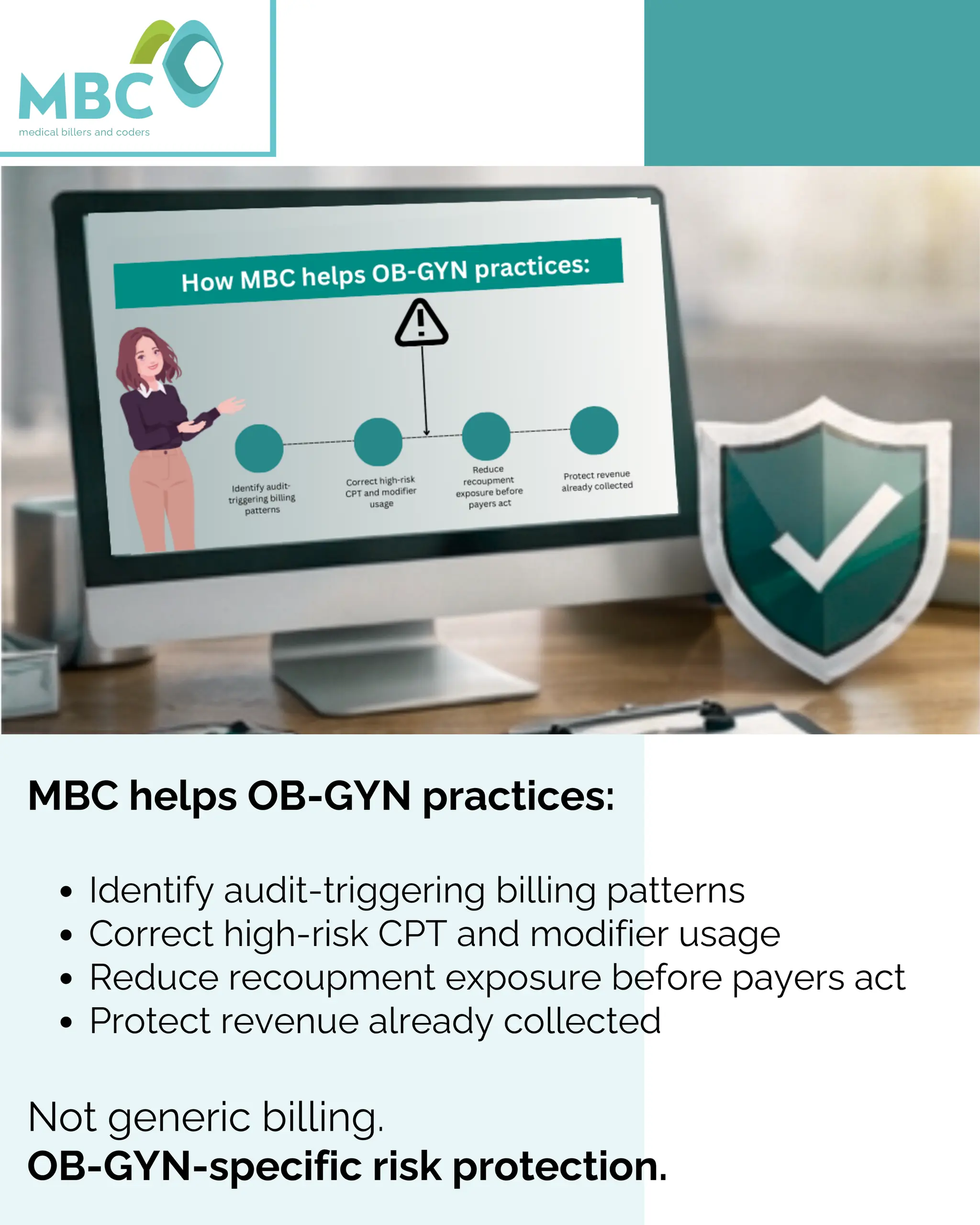
Download to read offline

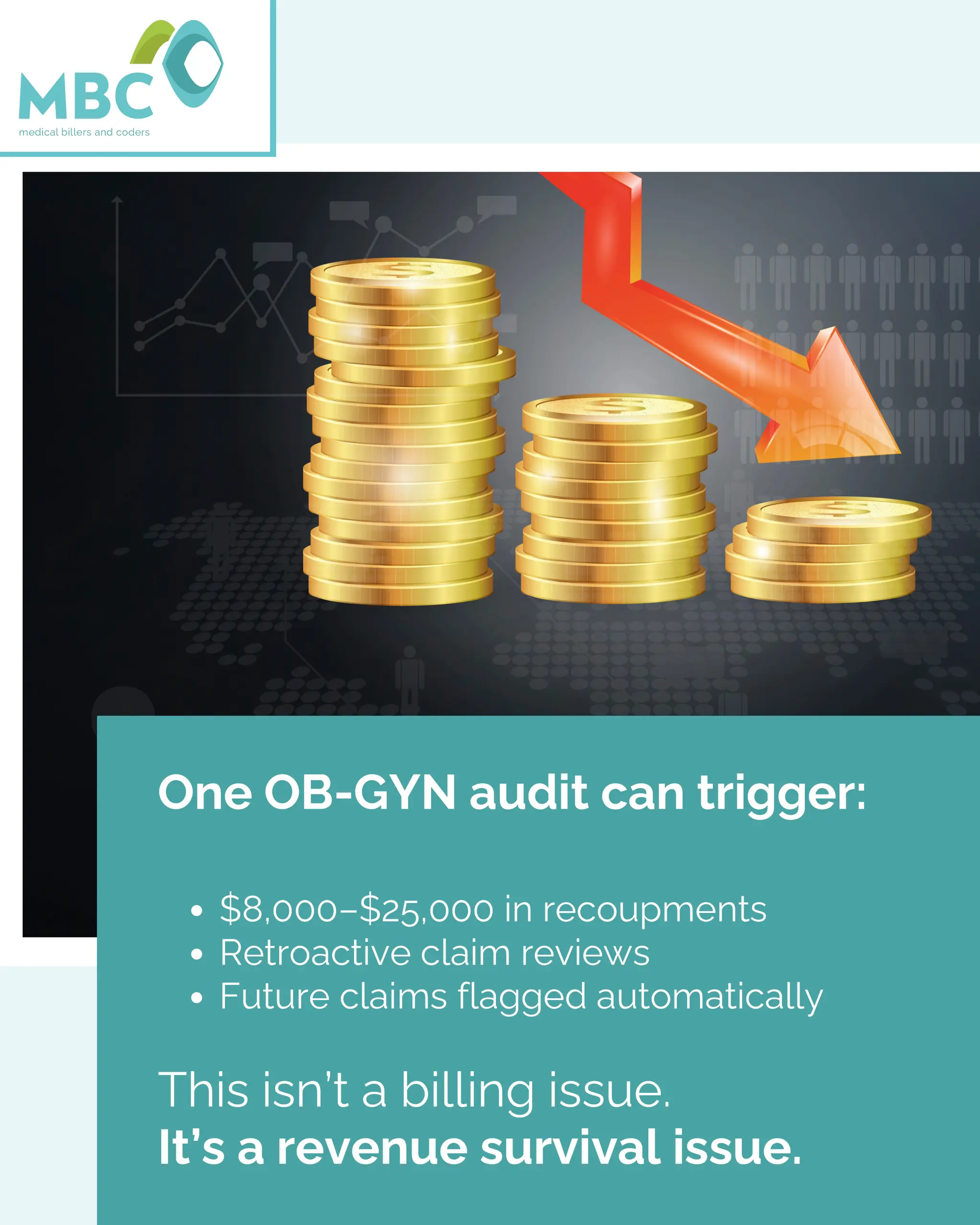
Many OB-GYN practices assume that paid claims mean compliance. In reality, payers audit after payment—often 6 to 18 months later—when the money has already been used. Incorrect global OB package billing, modifier misuse, weak E/M documentation, and lack of post-payment monitoring quietly expose practices to costly recoupments. When an audit hits, cash flow slows, staff scrambles, and revenue already earned is taken back. The biggest losses don’t happen because of audits—they happen because practices were unprepared. Medical Billers and Coders (MBC) helps OB-GYN practices identify audit-triggering patterns early, correct high-risk CPT and modifier usage, and reduce recoupment exposure before payers act. This is OB-GYN–specific risk protection, not generic billing. Before payers review your claims, you should. Contact Medical Billers and Coders Phone: 888-357-3226 Website: medicalbillersandcoders.com OB-GYN billing audits, audit risk review, OB-GYN billing compliance, recoupment prevention, medical billing services, revenue protection, post-payment audit review