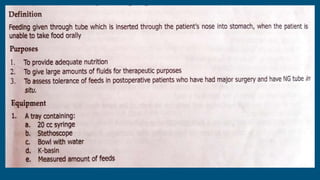
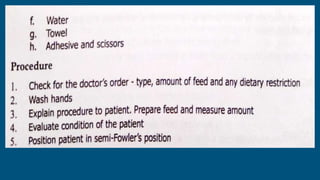
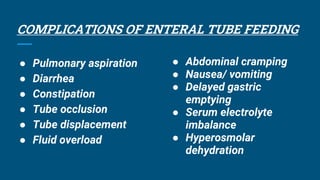
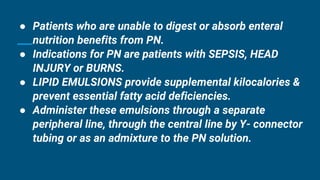
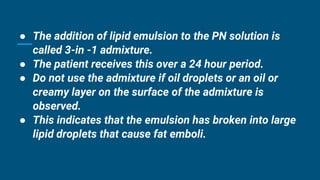
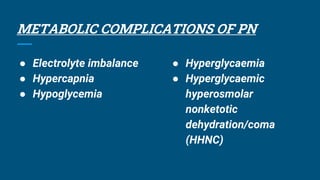
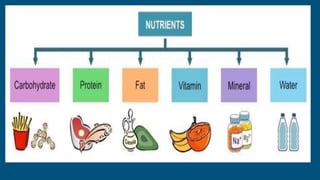
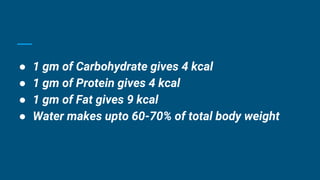
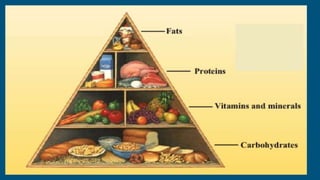
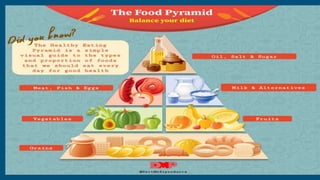
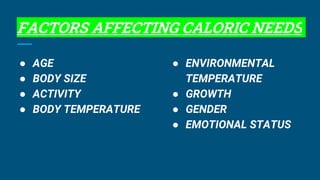
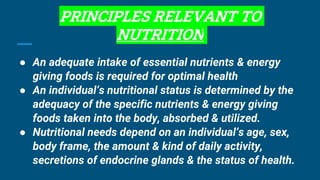
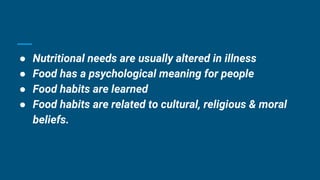
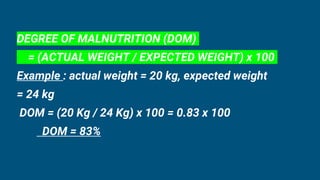
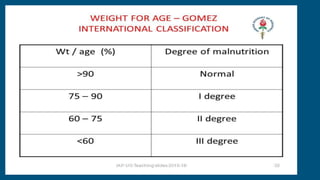
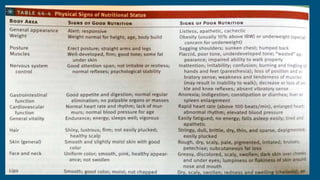
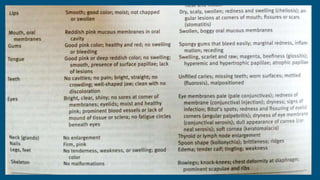
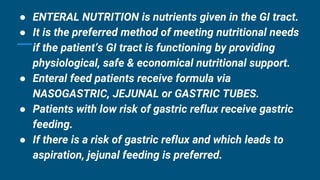
The document outlines the importance of nutrition for health, including the energy requirements for maintaining bodily functions and the factors influencing dietary intake. It discusses methods for assessing nutritional status and managing nutrition through diet and enteral or parenteral feeding, especially in patients with specific health conditions. Additionally, it covers the principles of medical nutrition therapy and the various complications associated with nutritional support methods.









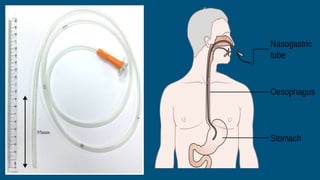
![● Feeding tubes are inserted through the nose
(NASOGASTRIC or NASO INTESTINAL), surgically
(GASTROSTOMY or JEJUNOSTOMY) or endoscopically
(PERCUTANEOUS ENDOSCOPIC GASTROSTOMY[PEG]
or JEJUNOSTOMY [PEJ]).
● If enteral nutrition therapy is less than 4 weeks total,
NG or NJ feeding tubes may be used.](https://image.slidesharecdn.com/nutritionalneeds-230212180909-5851a29f/85/NUTRITIONAL-NEEDS-pptx-57-320.jpg)