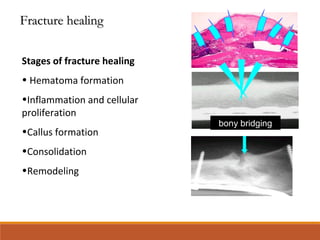
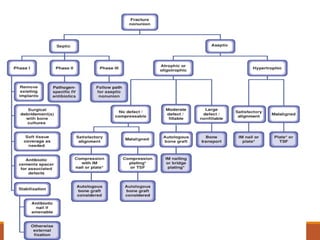
This document discusses nonunion fractures, including definitions, causes, classification, evaluation, and management. Some key points:
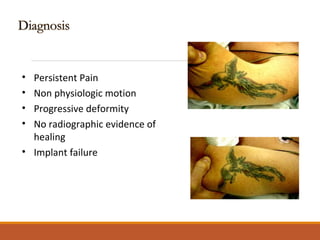
- Nonunion occurs when a fracture fails to heal in the expected time and is unlikely to heal without further intervention. Delayed union is when healing is delayed but still possible with treatment.
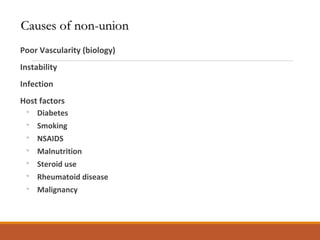
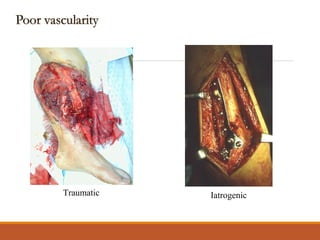
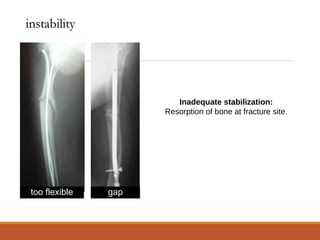
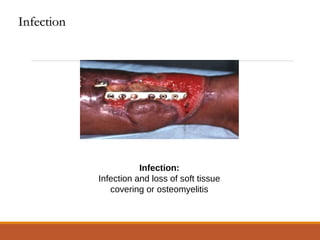
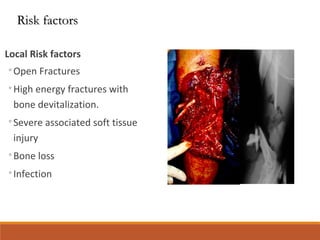
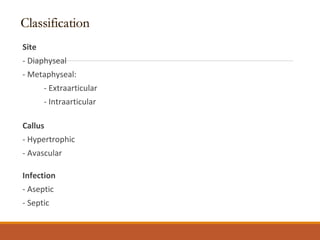
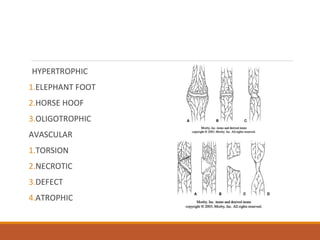
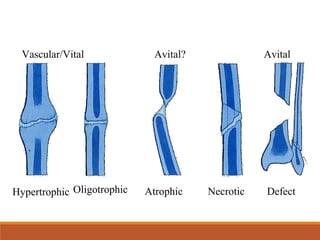
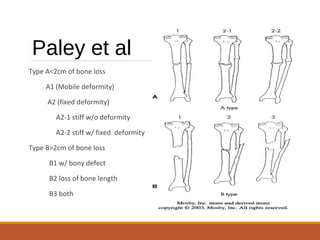
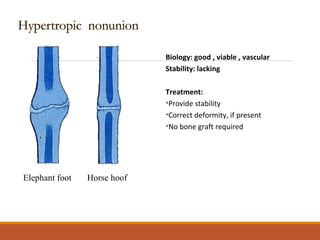
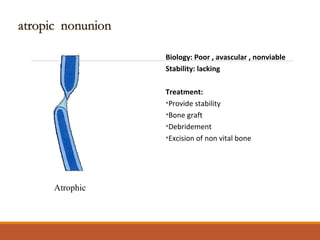
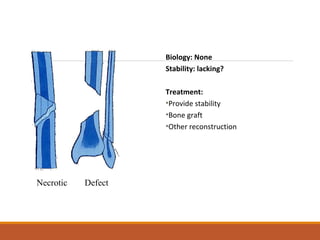
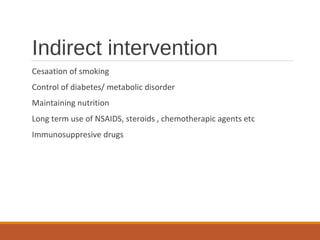
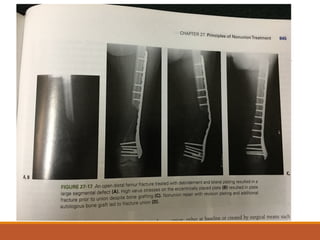
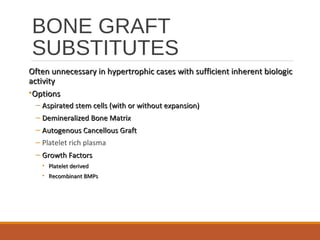
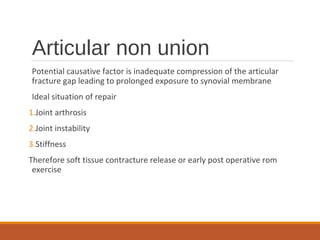
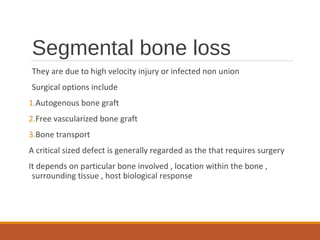
- Causes of nonunion include poor vascularity, instability, infection, and patient factors like smoking or diabetes. Types of nonunion include hypertrophic, atrophic, necrotic, and defect.
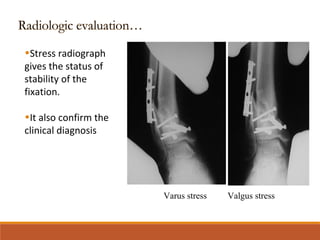
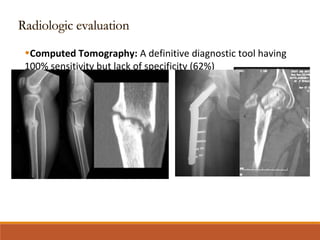
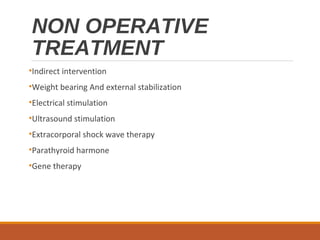
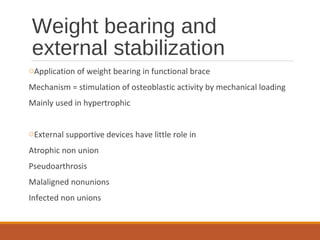
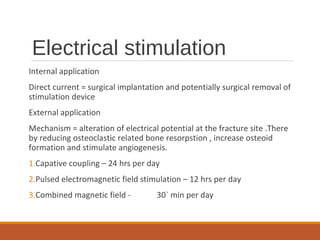
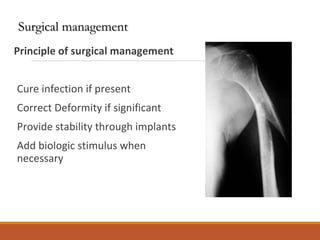
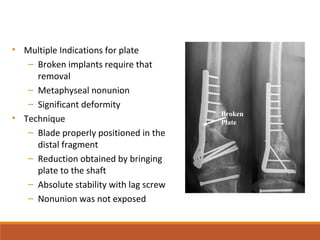
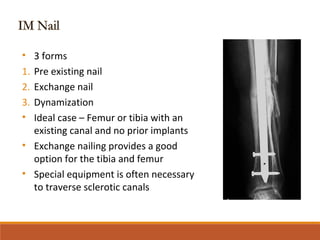
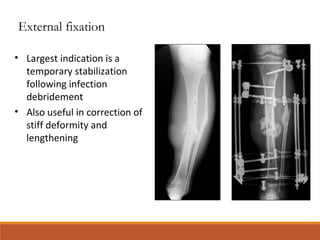
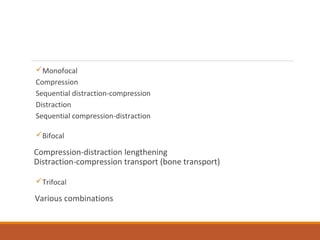
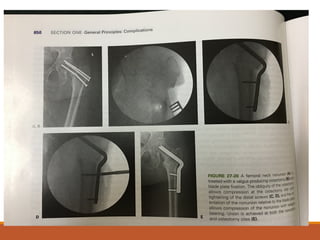
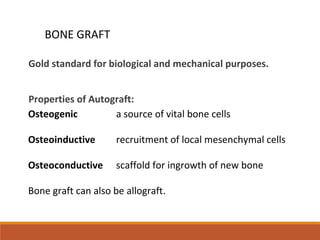
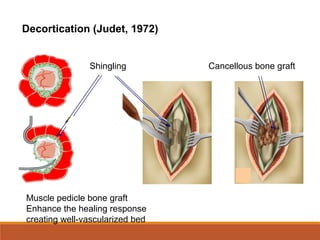
- Evaluation involves standard radiographs and stress views. Treatment includes non-operative options like bracing or stimulation, or operative options like plating, nailing, bone grafting, and correction