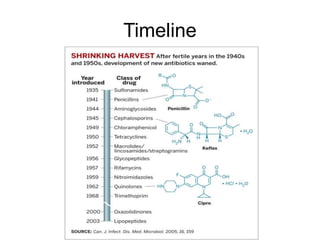
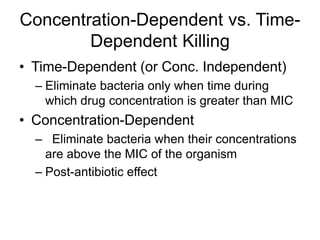
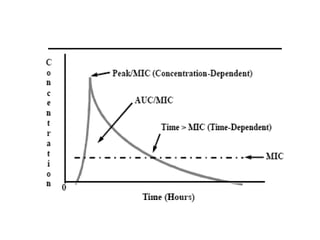
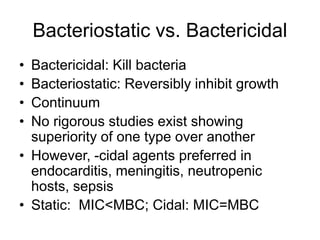
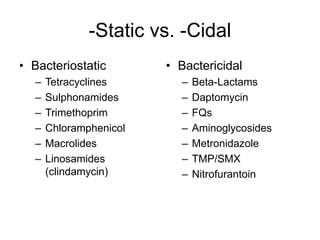
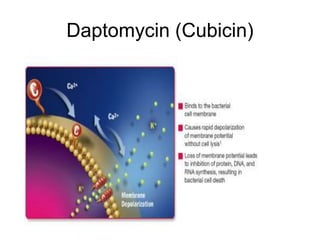
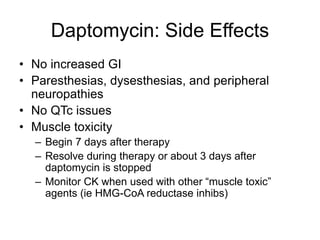
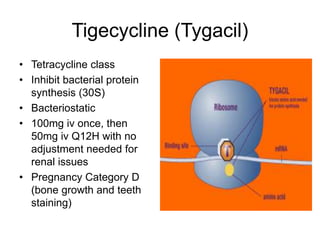
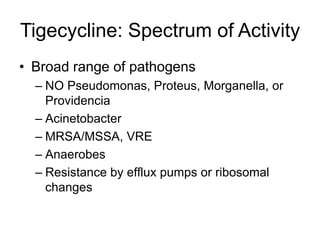
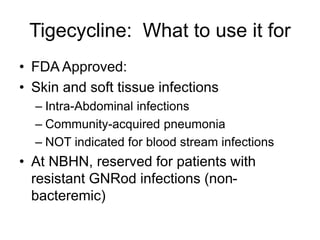
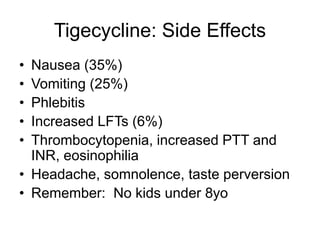
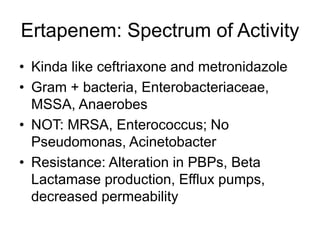
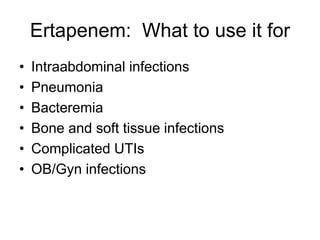
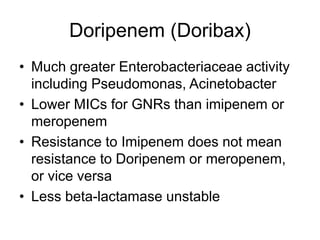
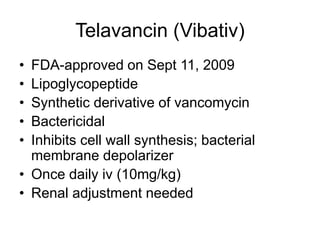
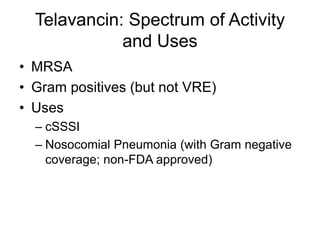
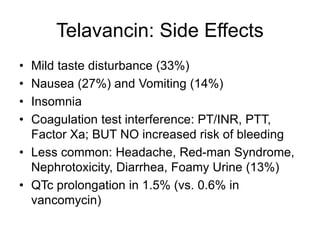
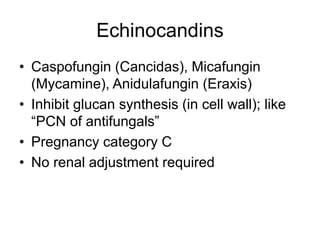
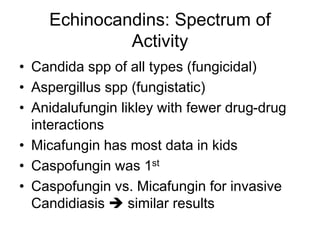
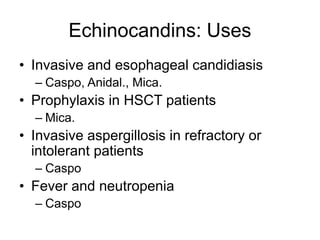
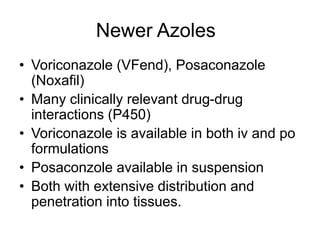
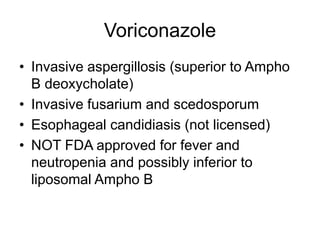
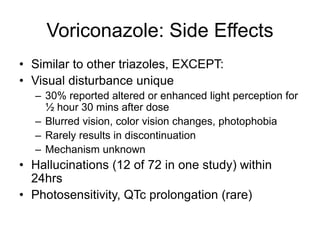
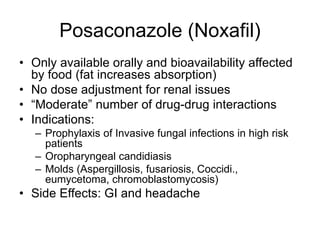
The document provides an overview of various newer antibiotics, their mechanisms of action, spectrum of activity, and appropriate uses for specific infections. It discusses the differences between bactericidal and bacteriostatic agents, along with specific antibiotics such as linezolid, daptomycin, tigecycline, and others, highlighting their side effects and resistance issues. Additionally, it covers antifungals like echinocandins and newer azoles, detailing their applications and potential side effects.