This document provides information about a handbook titled "Taylor's Musculoskeletal Problems and Injuries" which was edited by Robert B. Taylor and includes contributions from various associate editors and authors. The handbook contains 12 chapters covering a range of musculoskeletal disorders, injuries, and related topics that are relevant for primary care clinicians. It is intended to address deficiencies in musculoskeletal training for physicians in family medicine, internal medicine, pediatrics, and other fields involved in primary care.














![Physical Examination
The initial examination is fairly detailed. With the patient standing
and appropriately gowned, the examining physician notes the stance
and gait, as well as the presence or absence of the normal curvature of
the spine (e.g., thoracic kyphosis, lumbar lordosis, splinting to one
side, scoliosis). The range of motion of the back is documented,
including flexion, lateral bending, and rotation. Intact dorsiflexion
and plantar flexion of the foot is determined by observing heel-walk
and toe-walk. Intact knee extension is determined by observing the
patient squat and rise, while keeping the back straight.
With the patient seated, a distracted straight-leg raising test is
applied. With the hip flexed at 90 degrees, the flexed knee is brought
to full extension. A positive straight-leg raising test reproduces the
patient’s paresthesias in the distribution of a nerve root at ⬍60
degrees of knee extension. Sensation to light touch and pinprick are
examined and motor strength of hip and knee flexors is tested. The
deep tendon reflexes are tested [knee jerk (L4), ankle jerk (S1)]
and long tract signs are elicited by applying Babinski’s maneuver
(Table 1.1).
With the patient in the supine position, the straight-leg raising test
is repeated. With the hip and knee extended, the leg is raised (i.e., the
1. Disorders of the Back and Neck 5
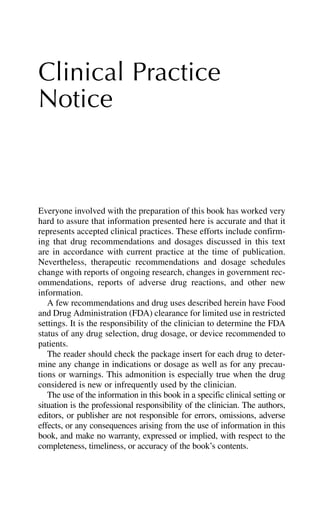
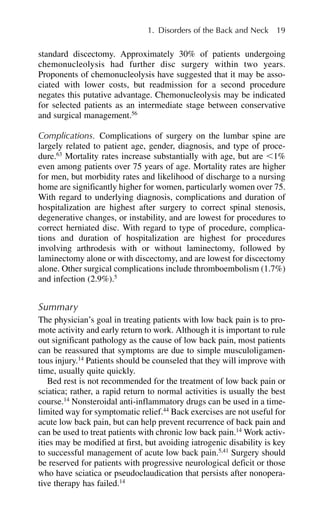
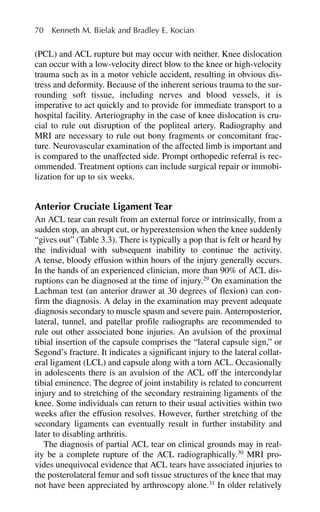
Table 1.1. Motor, Sensory, and Deep Tendon Reflex Patterns
Associated with Commonly Affected Nerve Roots
Deep tendon
Nerve root Motor reflexes Sensory reflexes reflexes
C5 Deltoid Lateral arm Biceps jerk (C5,C6)
C6 Biceps, Lateral forearm Brachioradialis
brachioradialis,
wrist extensors
C7 Triceps, wrist Middle of hand, Triceps jerk
flexors, MCP middle finger
extensors
C8 MCP flexors Medial forearm —
T1 Abductors and Medial arm —
adductors of
fingers
L4 Quadriceps Anterior thigh Knee jerk
L5 Dorsiflex foot Dorsum of foot Hamstring reflex
and great toe (L5, S1)
S1 Plantarflex foot Lateral foot, Ankle jerk
posterior calf
MCP ⫽ metacarpophalangeal.](https://image.slidesharecdn.com/musculoskeletalpocketbook-230104013636-e7f180fd/85/musculoskeletal-pocketbook-pdf-19-320.jpg)





























![Examination of the patient with a rotator cuff injury reveals painful or
limited active abduction (between 60 and 120 degrees), where the cuff
comes in greatest contact with the overlying acromial arch.9
With a
significant cuff tear, the patient is frequently unable to hold the arm in
90 degrees of abduction. Atrophy may develop in the supraspinatus or
infraspinatus muscles of the scapula. If a cuff tear is suspected, ortho-
pedic referral with arthroscopy or magnetic resonance imaging (MRI)
is indicated to delineate potential surgical cases. With any cuff injury
an extensive rehabilitation program of three to six months is needed
to gain full motion and strength.
Subacromial Bursitis
The subacromial bursa separates the deltoid muscle from the underly-
ing rotator cuff. Irritation of adjacent structures, most commonly
impingement of the rotator cuff, results in inflammatory bursitis.
Often there is a history of overuse or trauma followed by pain and
limited active motion. Aspiration of excessive bursal fluid followed
by corticosteroid injection using a subacromial lateral or posterior
approach can provide dramatic relief of this problem.3
Adequate vol-
ume of injection [5 to 10 cc lidocaine (Xylocaine) plus corticosteroid]
should be used to optimize injection results.
Calcific tendonitis, usually within the supraspinatus insertion, may
cause an acute inflammatory reaction of the overlying subacromial
bursa. Roentgenograms demonstrate a calcific deposit superior and
lateral to the humerus. The severe pain can be relieved by needle aspi-
ration of the calcific mass along with a lidocaine and corticosteroid
injection of the bursa. Occasionally surgical excision of the calcific
deposition is required.10
Bicipital Tendonitis and Rupture
The long head of the biceps tendon, which is palpable in the bicipital
groove, may be irritated as it courses through the glenohumeral joint
and below the supraspinatus tendon to its attachment at the superior
sulcus of the glenoid. Isolated pain over the long head of the biceps
tendon suggests this problem, although usually there is more diffuse
tenderness involving the entire subacromial region. The short head of
the biceps tendon attaches to the coracoid process and is rarely
involved in inflammatory problems of the shoulder. In most cases rup-
ture of the long head of the biceps tendon occurs as a result of
advanced impingement in middle-aged or elderly patients. There is a
sudden pop associated with a heavy isometric flexion of the arm such
as lifting a heavy object with that arm. The patient experiences mild
40 Ted C. Schaffer](https://image.slidesharecdn.com/musculoskeletalpocketbook-230104013636-e7f180fd/85/musculoskeletal-pocketbook-pdf-54-320.jpg)
















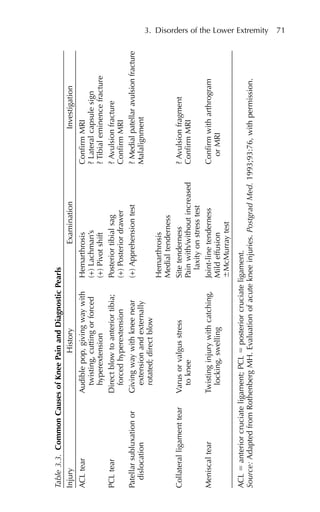
![tensile trabeculae, and wider trochanteric region) on plain radiographs
were as predictive of risk for hip fracture as bone mineral density
determinations.4
Dexa scanning has become an important tool in
screening for osteoporosis.
The best treatment for osteoporosis is prevention. Preventive meas-
ures include hormone replacement therapy, exercise, alendronate,
increased calcium intake, and calcitonins (see Reference 56, Chapter
122). Recently, combination therapies of estrogen and alendronate
have yielded even greater increases in bone mineral density and are
tolerated quite well.5
Certain facts are important to remember when
considering the prescription of preventive measures: short-term inter-
vention late in the natural course of osteoporosis may have significant
effects on the incidence of hip fractures;6
hip fracture may be associ-
ated with reduced muscle strength rather than reduced body mass or
fat;7,8
long-term heavy activity reduces the risk of hip fracture in post-
menopausal women;9
and height appears to be an important inde-
pendent risk factor for hip fracture among American women and
men.10
Factors that are protective [relative risk (RR) ⬍1] against hip
fracture in the elderly are an increase in weight after age 25 and rou-
tine walking for exercise.
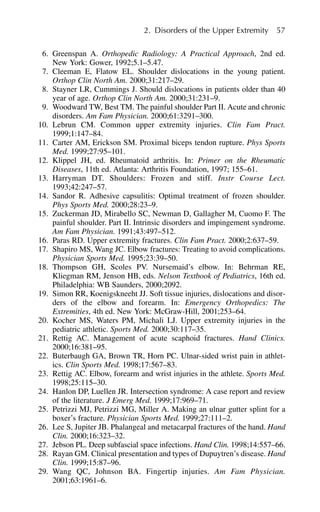
Fractures of the proximal femur can be classified as femoral neck,
intertrochanteric, or subtrochanteric based on anatomic site. Fractures
of the femoral neck (cervical or intracapsular) result from an indirect
shear force on the angulated femoral neck (Fig. 3.1). They are found
more commonly in the elderly and have a high risk for complications,
such as avascular necrosis. Fractures of the neck of the femur are
painful and can be associated with little bruising or swelling. It is
important to note that a nondisplaced fracture can be ambulated upon,
albeit with some degree of pain. A displaced fracture of the hip causes
shortening and external rotation. Extracapsular (intertrochanteric and
subtrochanteric) fractures occur with direct trauma to the hip, result-
ing in immediate pain, inability to ambulate, and generally significant
loss of blood. In the elderly, trochanteric fractures have been associ-
ated with up to twice the short-term mortality of cervical fractures. In
terms of measured bone mineral density (BMD), a relatively low
trochanteric BMD or a high femoral neck BMD is associated with
trochanteric hip fracture.11
Immediate referral for orthopedic surgery
is necessary. Treatment options take into account the type and extent
of fracture: cervical fractures in the elderly and significant displace-
ments require hip replacement, and extracapsular fractures respond
well with repair and internal fixation.
With suspected hip fracture and negative plain radiographs, mag-
netic resonance imaging (MRI) demonstrated occult femoral and
3. Disorders of the Lower Extremity 61](https://image.slidesharecdn.com/musculoskeletalpocketbook-230104013636-e7f180fd/85/musculoskeletal-pocketbook-pdf-75-320.jpg)
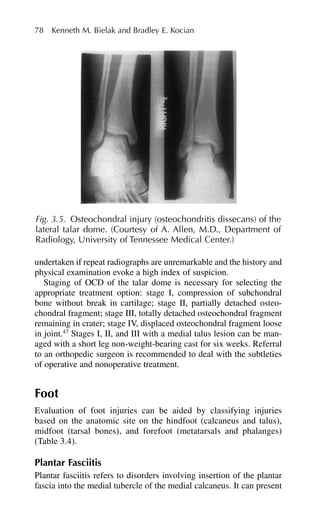
![ment plan.16
In the absence of penetrating trauma, intracapsular gas
bubbles on CT are reliable indicators of recent hip dislocation and
may be the only objective finding of this injury.17
MRI can be used for
the early detection of osteonecrosis of the femoral head after trau-
matic hip dislocation or fracture dislocation.18
Traumatic anterior dislocation of the hip represents 11% of all hip
dislocations and is classified into superior and inferior types.
Associated femoral head fractures are common, but acetabular frac-
tures are relatively rare. Whereas inferoanterior hip dislocation is eas-
ily recognized on an anteroposterior radiograph of the pelvis, the
radiographic appearance of superoanterior hip dislocation is less
straightforward. Misinterpretation of a superoanterior hip dislocation
can lead to an initial misdiagnosis of posterior hip dislocation, which
has implications for the surgical approach and may result in failed
closed reduction.19
The superoanterior dislocation of the femoral head
can be distinguished from the posterior dislocation by noting a more
lateral orientation to the acetabulum and an externally rotated femur
that is not adducted. The lesser trochanter becomes more prominent
medially.20
Central hip dislocations usually occur with resulting fracture to the
iliopubic portion of the acetabulum as a severe lateral blow to the hip
drives the femoral head medially. There are usually other skeletal and
soft tissue injuries associated with this type of injury.14
After closed reduction of a hip dislocation, it is necessary to con-
firm concentric reduction (the joint space is equidistant on plain radi-
ograph or CT scan). The absence of concentric reduction suggests an
interposition of soft tissue in the joint. Early diagnosis and treatment
of this serious complication can avoid the poor results of open and
deferred treatments.21
Pelvic Avulsion Injuries
The bony attachments of the sartorius [anterior superior iliac spine
(ASIS)], rectus femoris (anterior inferior iliac spine), and the ham-
strings (ischial tuberosity) can be individually avulsed by sudden
overloading of the respective muscles (acute muscular contraction
against a fixed resistance). The history is typically a sudden onset of
extreme pain following sudden, forceful acceleration or deceleration.
Localized pain and swelling at the site of injury and increased dis-
comfort with passive stretching and muscle contraction against resist-
ance suggest the diagnosis. Plain radiographs confirm the injury (Fig.
3.3). Subtleties may make the diagnosis obscure, and MRI may be a
more sensitive and accurate way to establish the diagnosis. The ham-
64 Kenneth M. Bielak and Bradley E. Kocian](https://image.slidesharecdn.com/musculoskeletalpocketbook-230104013636-e7f180fd/85/musculoskeletal-pocketbook-pdf-78-320.jpg)
















![management strategies for OA include periods of rest (one to two
hours) when symptoms are at their worst, avoidance of repetitive
movements or static body positions that aggravate symptoms, heat
(or cold) for the control of pain, weight loss if the patient is over-
weight, adaptive mobility aids to diminish the mechanical load on
joints, adaptive equipment to assist in activities of daily living
(ADL), range of motion exercises, strengthening exercises, and
endurance exercises.11,12
Immobilization should be avoided. The use
of adaptive mobility aids (e.g., canes, walkers) is an important strat-
egy, but care must be taken to ensure that the mobility aid is the cor-
rect device, properly used, appropriately sized, and in good repair.
Medial knee taping to realign the patella in patients with
patellofemoral OA, and the use of wedged insoles for patients with
medial compartment OA and shock-absorbing footwear may help
reduce joint symptoms.10,13
Pharmacological approaches to the treatment of OA include aceta-
minophen, salicylates, nonselective nonsteroidal anti-inflammatory
drugs (NSAIDs), cyclooxygenase-2 (COX-2) specific inhibitors, top-
ical analgesics, and intra-articular steroids.14,15
Acetaminophen is
advocated for use as first-line therapy for relief of mild to moderate
pain, but it should be used cautiously in patients with liver disease or
chronic alcohol abuse. Salicylates and NSAIDs are commonly used as
first-line medications for the relief of pain related to OA. Compliance
with salicylates can be a major problem given their short duration of
action and the need for frequent dosing; thus NSAIDs are preferable to
salicylates. There is no justification for choosing one nonselective
NSAID over another based on efficacy, but it is clear that a patient who
does not respond to an NSAID from one class may well respond to an
NSAID from another. The choice of a nonselective NSAID versus a
COX-2 specific inhibitor should be made after assessment of risk for
GI toxicity (e.g., age 65 or older, history of peptic ulcer disease, previ-
ous GI bleeding, use of oral corticosteroids or anticoagulants). For
patients at increased risk for upper GI bleeding, the use of a nonselec-
tive NSAID and gastroprotective therapy or a COX-2 specific inhibitor
is indicated. NSAIDs should be avoided or used with extreme caution
in patients at risk for renal toxicity [e.g., intrinsic renal disease, age 65
or over, hypertension, congestive heart failure, and concomitant use of
diuretics or angiotensin-converting enzyme (ACE) inhibitors].10
COX-
2 inhibitors increase the risk of heart attack and stroke.
Topical capsaicin may improve hand or knee OA symptoms when
added to the usual treatment; however, its use may be limited by
cost and the delayed onset of effect requiring multiple applications
daily and sustained use for up to four weeks. Intra-articular steroids
92 Alicia D. Monroe and John B. Murphy](https://image.slidesharecdn.com/musculoskeletalpocketbook-230104013636-e7f180fd/85/musculoskeletal-pocketbook-pdf-106-320.jpg)

























![with a platelet count as low as 20,000 cells/mm.3,23
Furthermore, SLE
patients have higher incidences of both arterial and venous thromboem-
bolic events. Some studies have shown up to a fiftyfold increase in risk
of myocardial infarction among reproductive-aged women with SLE,
compared to age-matched controls.18
Some investigators have recom-
mended prophylactic aspirin or other anticoagulation treatment for all
SLE patients, regardless of antiphospholipid status,24
and aggressive
anticoagulation with warfarin [with a goal international normalized ratio
(INR) of 2.5–3.5] for patients with known antiphospholipid antibodies.18
Treatment
Treatment of SLE is best tailored to individual patients and their specific
symptoms. Current treatment regimens have in general been successful
in decreasing the morbidity and mortality associated with SLE. Current
data indicate that more than 90% of patients survive at least 15 years.
All SLE patients are encouraged to minimize sun exposure and to use
sunscreen. The most common complaint, arthralgias, can often be ade-
quately treated with NSAIDs. Patients being treated long term with
NSAIDs should be monitored periodically for renal and hepatic side
effects. Glucocorticoids have also been used to treat severe symptoms,
but they increase the risk of side effects. Cutaneous manifestations of
SLE generally respond well to treatment with antimalarials (i.e.,
hydroxychloroquine or quinacrine). For treatment of skin disease resist-
ant to either of these agents, small studies have used dapsone, azathio-
prine, gold, intralesional interferon, and retinoids. Methotrexate is more
effective than placebo for moderate SLE without renal involvement.18
The foundation of treatment of SLE patients with renal disease has
long been glucocorticoid therapy; however, this practice is being chal-
lenged. Patients with mild disease can often be managed with low-
dose prednisone; patients with diffuse proliferative or severe focal
proliferative glomerulonephritis may require a two-month course of
high-dose prednisone (1 mg/kg) followed by a prolonged taper.
However, studies using cyclophosphamide have shown this drug to be
effective as either a single agent or in combination with glucocorti-
coids, and more effective than glucocorticoids alone.18,23
Like treatment of renal disease, the mainstay for treating thrombocy-
topenia has long been glucocorticoids. Patients with disease resistant to
glucocorticoid treatment may respond to splenectomy, but prior to con-
sideration of splenectomy providers must weigh the benefits against the
risks posed by decreased immune function. Cyclophosphamide and
chemotherapeutic agents such as vincristine and procarbazine have also
been used in patients with severe disease.23
118 Joseph W. Gravel Jr., Patricia A. Sereno, Katherine E. Miller](https://image.slidesharecdn.com/musculoskeletalpocketbook-230104013636-e7f180fd/85/musculoskeletal-pocketbook-pdf-132-320.jpg)
























![bone resorption mediated by osteoclasts and are effective in Paget’s
disease. These treatments have significant potential side effects and
complications. The alkaline phosphatase level can be used to monitor
disease activity.
Prognosis. The later in life that Paget’s disease begins, the better is
the prognosis. The progression is usually slow, over years. Renal
complications and malignant degeneration of lesions are associated
with a poor prognosis.
References
1. Clauw DJ. Fibromyalgia: More than just a musculoskeletal disease. Am
Fam Physician. 1995;52:843–51.
2. Goldenberg DL. Fibromyalgia syndrome: An emerging but controversial
condition. JAMA. 1987;257:2782–7.
3. Stormorken H, Brosstad F. Fibromyalgia: Family clustering and sensory
urgency with early onset indicate genetic predisposition and thus a “true”
disease [letter]. Scand J Rheumatol. 1992;21:207–11.
4. Silman A, Schollum J, Croft P. The epidemiology of tender point counts
in the general population [abstract]. Arthritis Rheum. 1993;36(suppl):48.
5. Granges G, Littlejohn GO. A comparative study of clinical signs in
fibromyalgia/fibrositis syndrome, healthy and exercising subjects. J
Rheumatol. 1993;20:344–51.
6. Reynolds WJ, Moldofsky H, Saskin P, et al. The effects of cyclobenza-
prine on sleep physiology and symptoms in patients with fibromyalgia. J
Rheumatol. 1991;18:452–4.
7. Simms RW, Goldenberg DL. Symptoms mimicking neurologic disorders
in fibromyalgia syndrome. J Rheumatol. 1988;15:1271–3.
8. Pellegrino MJ, Van Fossen D, Gordon C, et al. Prevalence of mitral valve
prolapse in primary fibromyalgia: A pilot investigation. Arch Phys Med
Rehabil. 1989;70:541–3.
9. Goldenberg DL. Management of fibromyalgia syndrome. Rheum Dis
Clin North Am. 1989;15:499–512.
10. Felson DT, Goldenberg DL. The natural history of fibromyalgia. Arthritis
Rheum. 1986;29:1522–6.
11. Yunus MB, Kalyan-Raman UP, Kalyan-Raman K. Primary fibromyalgia
syndrome and myofascial pain syndrome: Clinical features and muscle
pathology. Arch Phys Med Rehabil. 1988;69:451–4.
12. Thompson JM. Tension myalgia as a diagnosis at the Mayo Clinic and its
relationship to fibrositis, fibromyalgia, and myofascial pain syndrome.
Mayo Clin Proc. 1990;65:1237–48.
13. Harden RN, Bruehl SP, Gass S, Niemiec C, Barbick B. Signs and symp-
toms of the myofascial pain syndrome: A national survey of pain man-
agement providers. Clin J Pain. 2000;16(1):64–72.
14. Lederhaas G. Complex regional pain syndrome: New emphasis. Emerg
Med. 2000;32:18–22.
6. Selected Disorders of the Musculoskeletal System 145](https://image.slidesharecdn.com/musculoskeletalpocketbook-230104013636-e7f180fd/85/musculoskeletal-pocketbook-pdf-159-320.jpg)


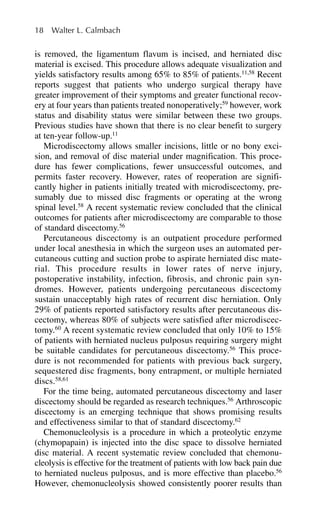
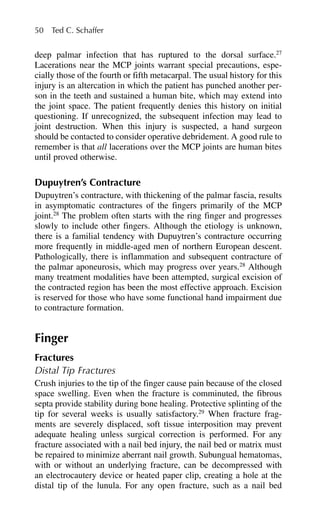
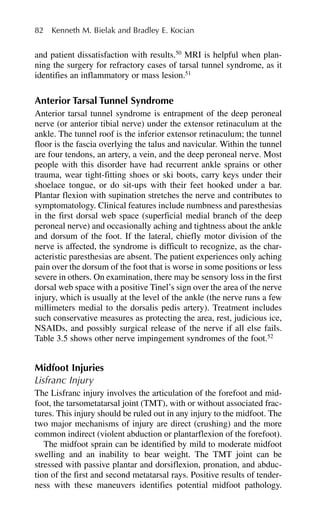
![Terminology
Definitions of the terms used in this chapter are as follows.
Angle of gait (foot progression angle): Angle of the intersection
between the foot axis and the line progression. It is the result of
static and dynamic influences from the foot to the hip. This angle
remains relatively stable at 8 to 12 degrees of out-toeing through
growth. There is a wide range of normal values varying from 3
degrees in-toeing to 20 degrees out-toeing; in one study of 130 chil-
dren, 4.5% had an in-toeing gait.2
Abnormalities anywhere along
this kinetic chain (including hip, leg, and foot) can change the angle
of gait.
Femoral antetorsion: Anteversion beyond the normal range [2 stan-
dard deviations (SD)].
Femoral anteversion: Angular difference between the forward
inclination of the femoral neck and the transcondylar femoral axis
(Fig. 7.2).
148 Mark D. Bracker et al.
A
C D E
c
B
b
a
Fig. 7.1. Tests for torsional deformities (see text for full discus-
sion). (A) Foot progression angle (a) is formed by the foot axis (B)
and the line of progression (b). (B) Foot axis. (C) Measurement of
internal femoral rotation. (D) Measurement of external femoral
rotation. (E) Thigh-foot angle (c) is formed by the longitudinal axis
of the femur and the foot axis. (From Lillegard and Kruse,50
with
permission.)](https://image.slidesharecdn.com/musculoskeletalpocketbook-230104013636-e7f180fd/85/musculoskeletal-pocketbook-pdf-162-320.jpg)







































































![Management
Modification of shoulder activity and antiinflammatory measures [the
RICE protocol, nonsteroidal antiinflammatory drugs (NSAIDs)] are
instituted early. Swimmers will need to alter the strokes during their
training periods and reduce the distance that they swim to the point
that the pain is decreasing daily. Rehabilitation exercises should con-
sist of both aggressive shoulder stretching to lengthen the cora-
coacromial ligament and improve range of motion. The use of an
upper arm counterforce brace will alter the fulcrum of the biceps in
such a way as to depress the humeral head further. Strength training
of the supraspinatus and biceps internal and external rotator muscles
should be performed to aid in depressing the humeral head when
stressed, thus increasing the subacromial space. In advanced calcific
tendonitis, steroid injection into the subacromial bursa or surgical
removal of the calcific tendon may be required.18
Tennis Elbow (Lateral Epicondylitis)
Lateral epicondylitis is characterized by point tenderness of the lateral
epicondyle at the attachment of the extensor carpi radialis brevis. The
most common sports that cause this syndrome are tennis, racquetball,
and cross-country skiing.19
The mechanism of injury in all of the sports
is the repetitive extension of the wrist against resistance. Adolescent or
preadolescent athletes are at highest risk of significant injury if the
growth plate that underlies the lateral epicondyle is not yet closed. If
the inflammation of the epicondyle is not arrested, the soft growth car-
tilage can fracture and rotate the bony attachment of the extensor liga-
ments, requiring surgical reimplantation of the epicondyle. Without
surgery, a permanent deformity of the elbow will result.
Diagnosis
Patients will complain of pain with active extension of the wrist local-
ized to the upper forearm and lateral epicondyle. There is usually
marked tenderness of the epicondyle itself. Pain with grasping a
weighted cup (Canard’s test) or with resisted dorsiflexion is also diag-
nostic. X-ray studies are not necessary but may show calcific changes
to the extensor aponeurosis in chronic cases. Comparison views of the
unaffected elbow may be helpful in the adolescent in whom a stress
fracture is suspected and the growth plate is not yet closed. Stress
fractures of the lateral epicondyle are best diagnosed with a tech-
netium-99 (Te-99) bone scan.
10. Athletic Injuries 223](https://image.slidesharecdn.com/musculoskeletalpocketbook-230104013636-e7f180fd/85/musculoskeletal-pocketbook-pdf-237-320.jpg)