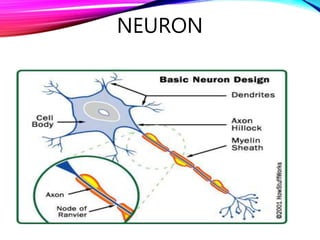
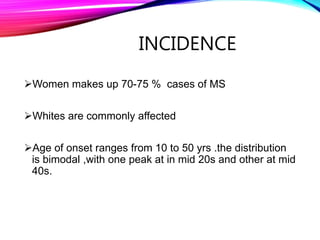
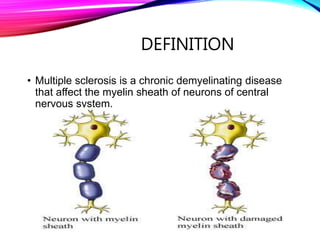
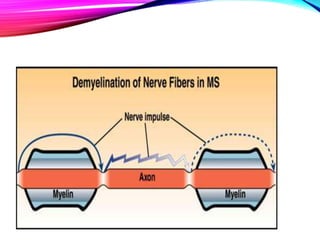
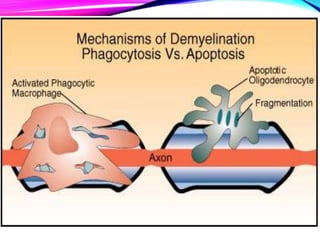
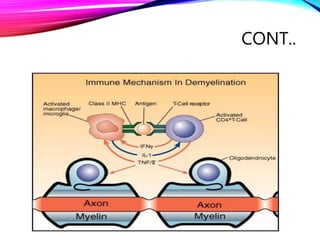
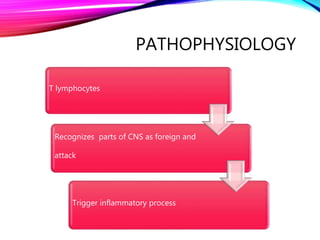
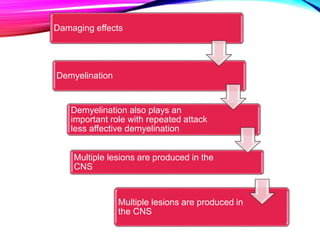
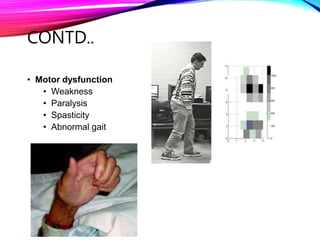
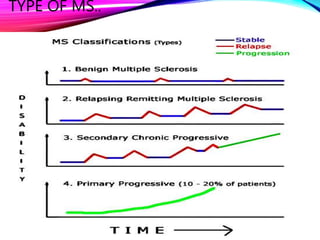
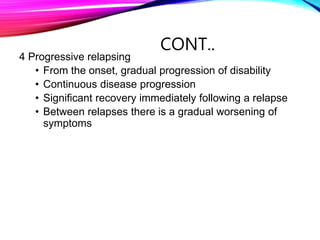
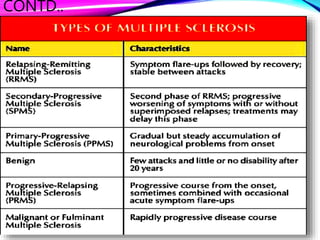
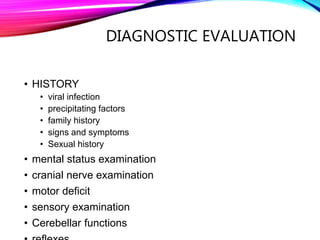
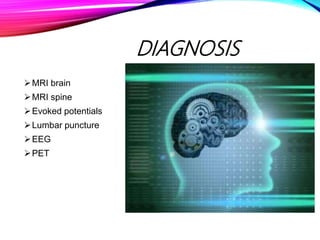
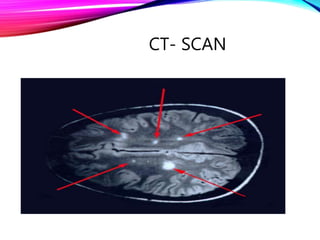
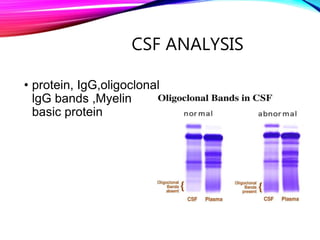
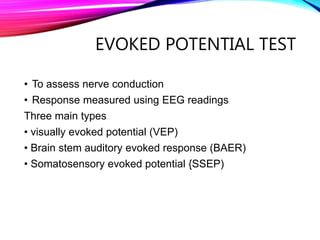
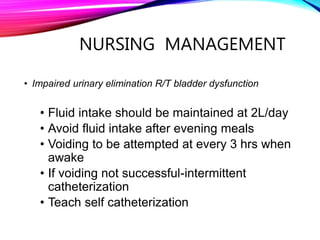
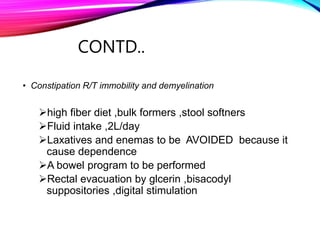
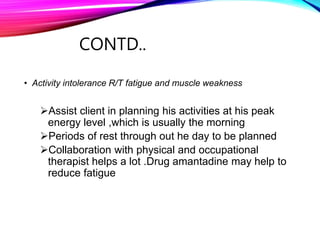
Multiple sclerosis is a chronic autoimmune disease that affects the central nervous system by destroying myelin sheaths surrounding neurons. It is the most common disabling neurological disease in young adults. The exact cause is unknown but is thought to involve genetic and environmental factors. There are several types but most common is relapsing-remitting MS where periods of relapse with new or worsening symptoms are followed by periods of remission. Diagnosis involves MRI, lumbar puncture, and evoked potential tests. While there is no cure, treatments aim to reduce frequency and severity of relapses and manage symptoms. Nursing care focuses on managing symptoms like bladder dysfunction, fatigue, mobility issues, and providing emotional support.