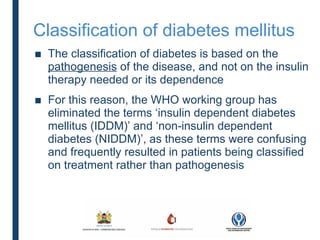
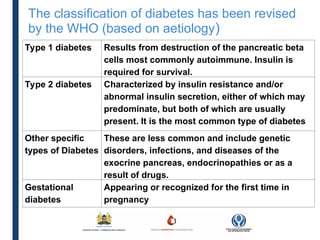
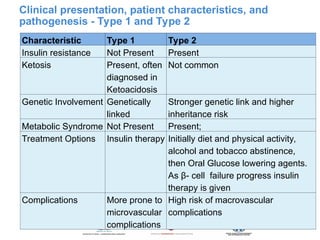
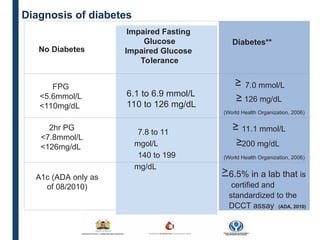
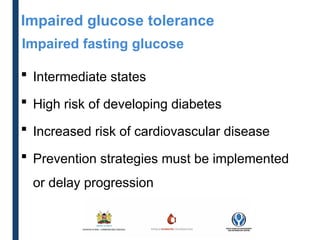
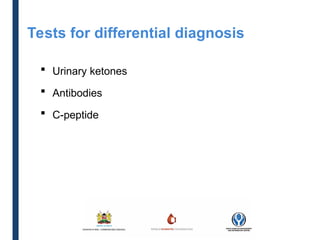
The document outlines the classification and diagnosis of diabetes, focusing on WHO criteria and the differences between type 1 and type 2 diabetes. It emphasizes that classification is based on disease pathogenesis rather than insulin dependence and details the clinical presentation, patient characteristics, and diagnostic criteria for different diabetes types. Additionally, it highlights the importance of capillary blood glucose monitoring and the management of impaired glucose tolerance and fasting glucose as risk factors for cardiovascular disease.