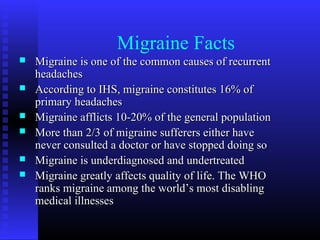
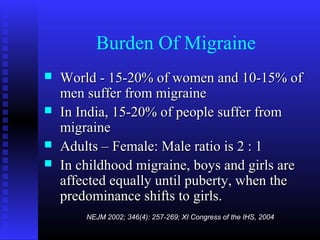
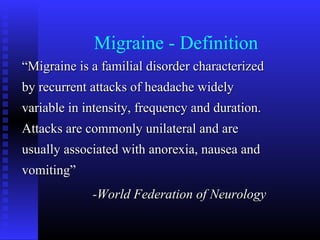
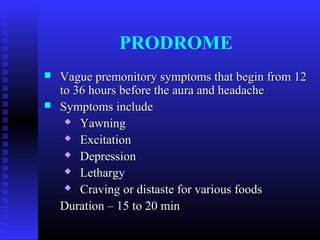
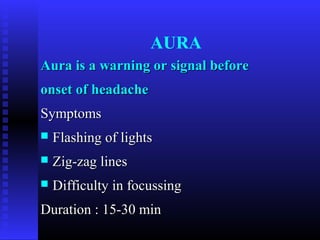
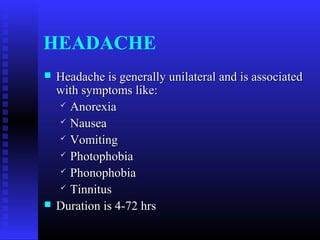
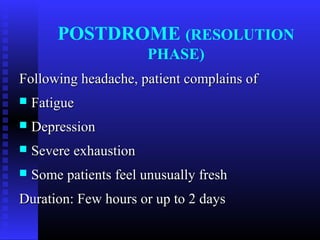
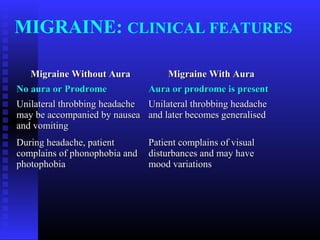
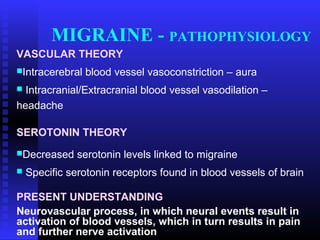
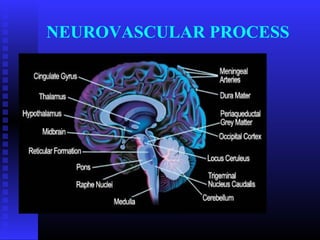
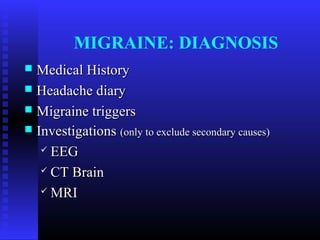
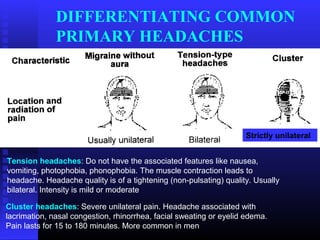
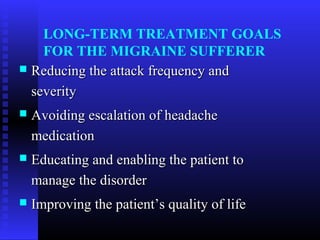
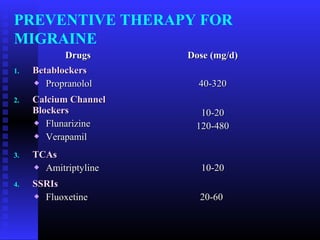
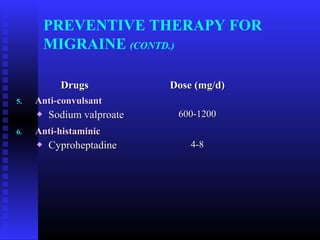
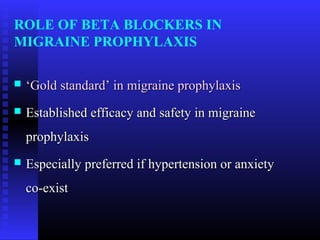
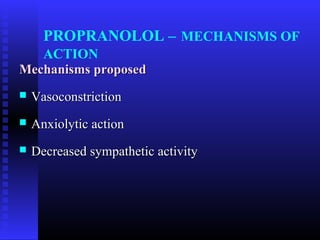
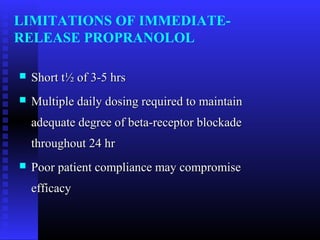
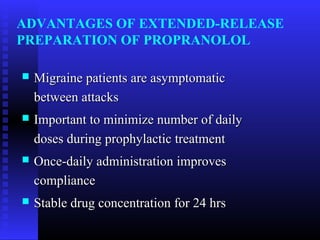
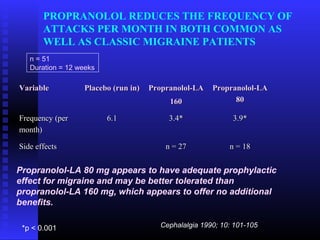
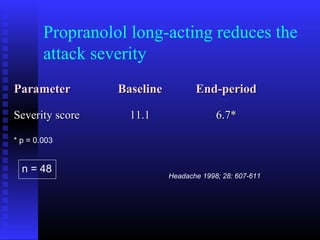
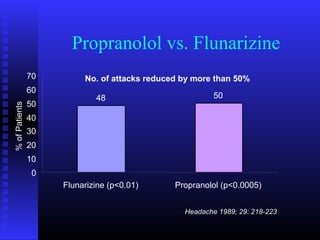
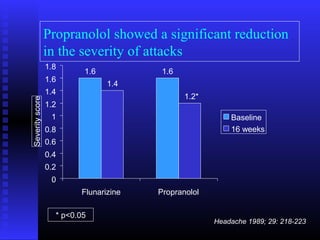
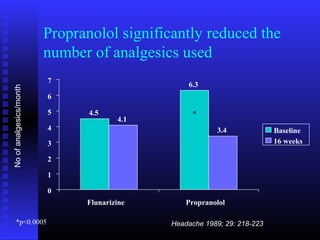
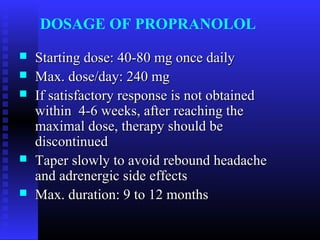
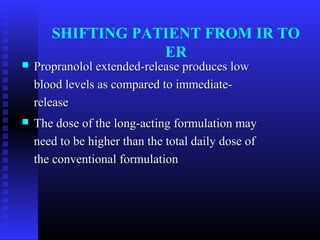
This document provides information on the management of migraines. It defines migraines and discusses their prevalence, burden, triggers, phases, and classification. It also covers the pathophysiology of migraines and outlines approaches to diagnosis, abortive treatment, and preventive treatment including medications like propranolol. Propranolol is positioned as the gold standard preventive treatment and its mechanisms of action, formulations, efficacy, dosage, and advantages over immediate-release versions are detailed.