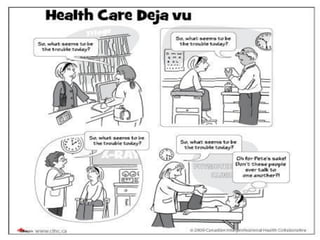
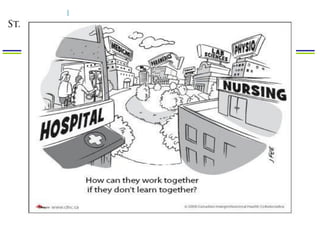
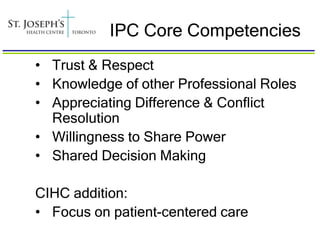
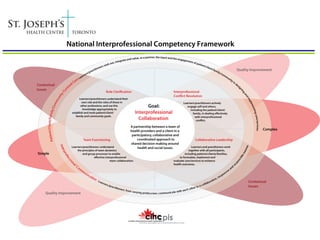
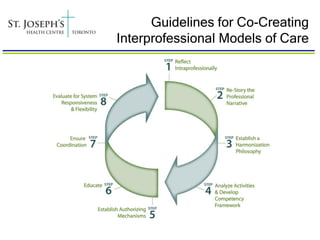
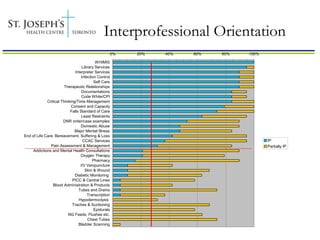
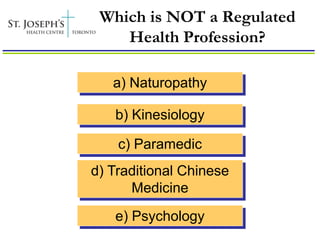
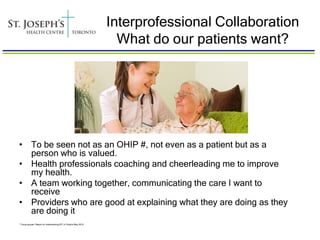
This document discusses interprofessional collaboration (IPC) and provides examples from St. Joseph's Health Centre of how IPC has been implemented. Some key points:
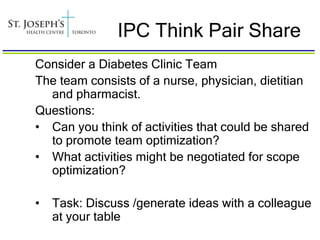
1) IPC involves intentional learning with, from, and about other professions to improve individual and team capacity and patient outcomes.
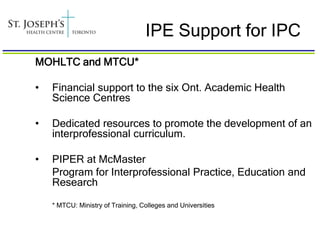
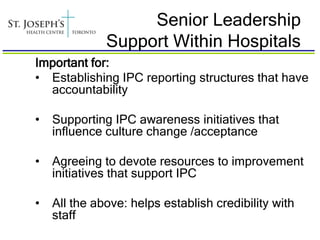
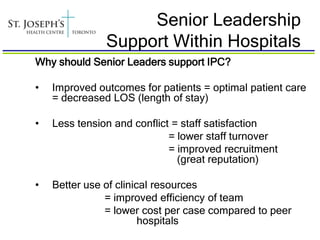
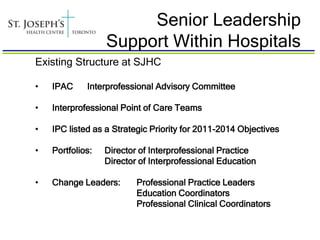
2) Government support through initiatives like funding academic health science centres has helped establish IPC. Hospitals also need senior leadership buy-in and dedicated roles to promote IPC.
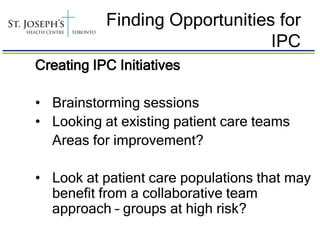
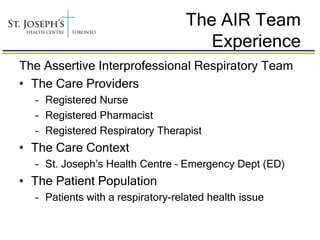
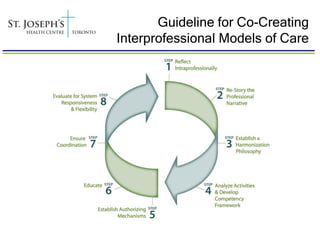
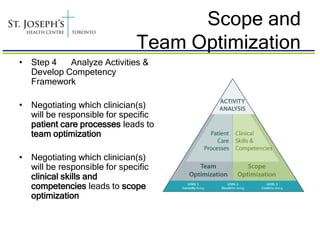
3) St. Joseph's has implemented structures like an interprofessional advisory committee and point of care teams to facilitate IPC. Change leaders and competency frameworks also support its adoption.
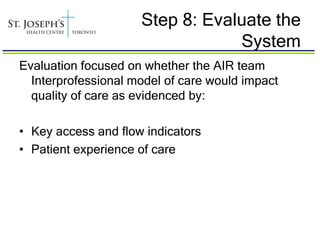
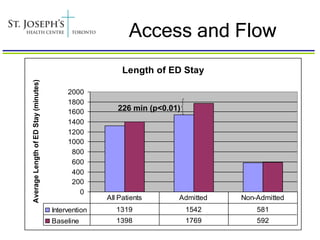
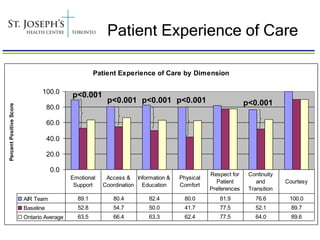
4) Evaluating initiatives like St. Joseph