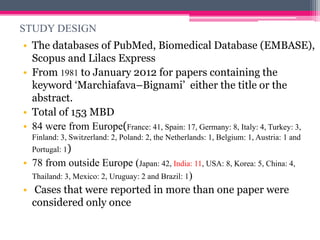
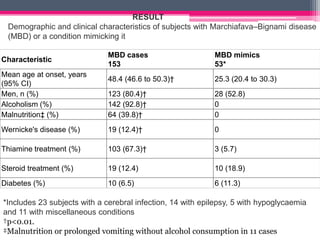
This study reviewed 153 cases of Marchiafava–Bignami disease (MBD) and 53 cases of conditions mimicking MBD that were diagnosed using MRI or CT. The key findings were:
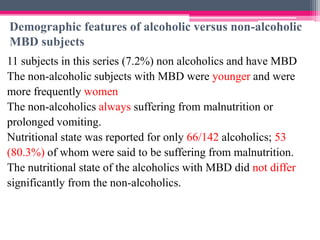
1) MBD patients were older, more often male alcoholics with malnutrition, while mimics were younger with various causes like infections or epilepsy.
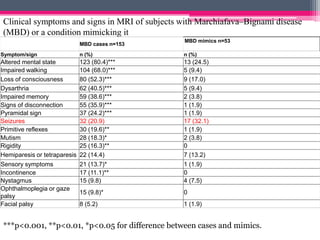
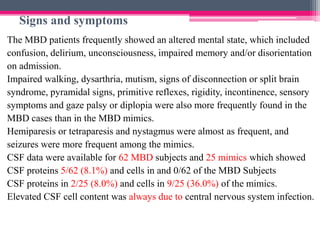
2) MBD patients presented with more severe neurological deficits like impaired walking and memory loss, while mimics had milder and shorter symptoms.
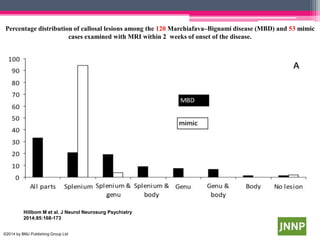
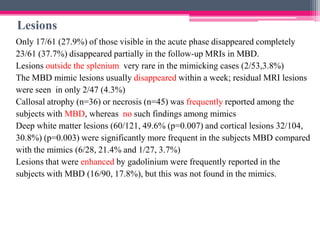
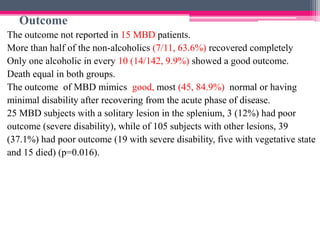
3) Lesions in MBD often involved multiple areas of the corpus callosum and were associated with poorer outcomes, while mimics typically had solitary splenium lesions.
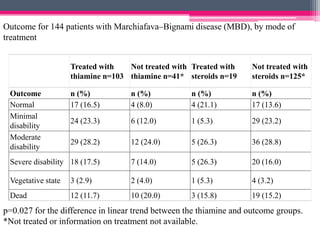
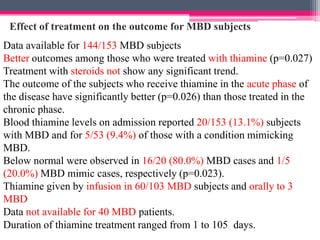
4) Treatment with parenteral