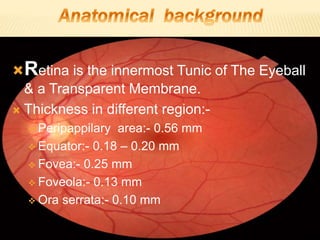
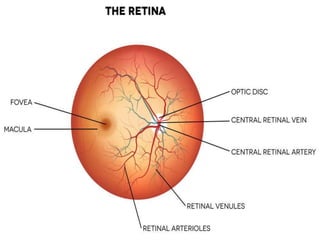
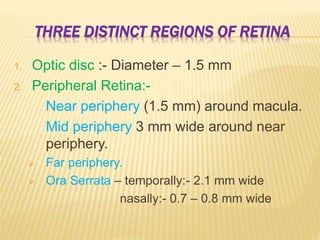
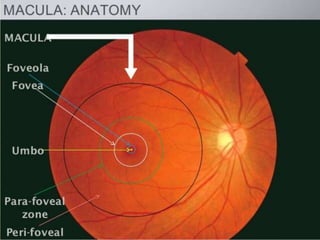
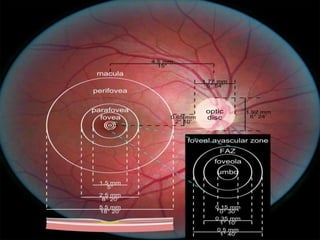
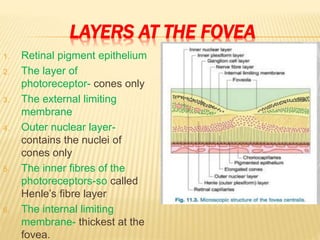
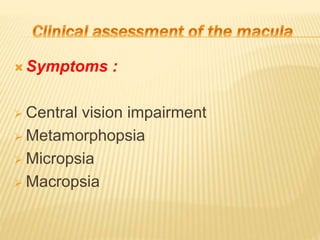
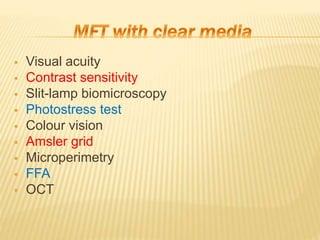
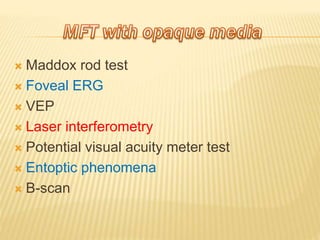
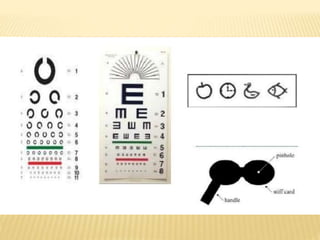
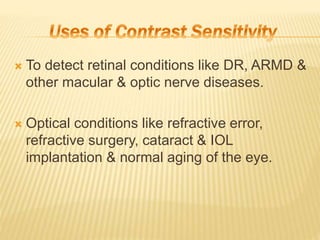
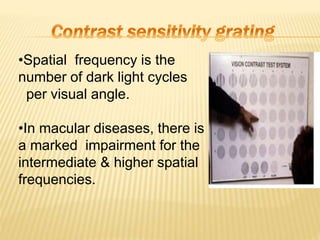
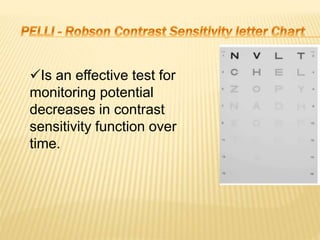
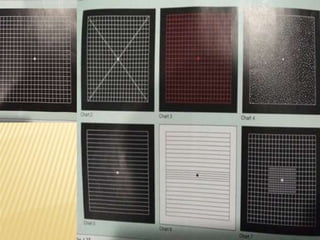
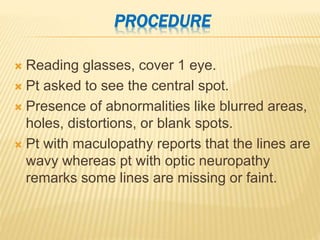
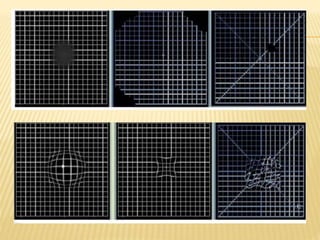
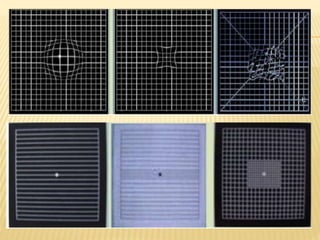
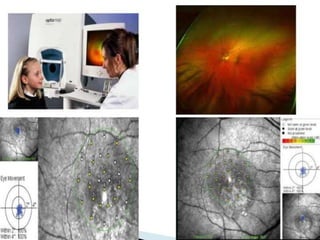
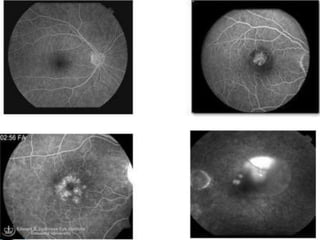
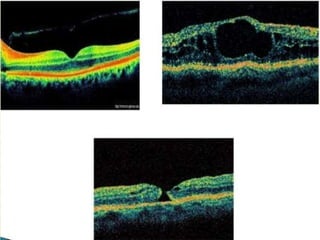
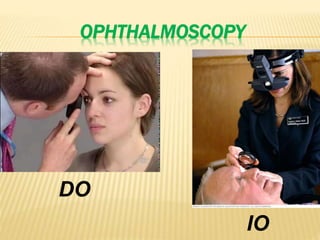
The document provides an extensive overview of the human retina, detailing its anatomy, thickness in various regions, and the structure and function of the macula and fovea. It covers symptoms of macular diseases, diagnostic tests to assess macular function and visual acuity, as well as various methodologies used in retinal imaging and evaluation. Additionally, it discusses the implications of different retinal conditions and the importance of testing for early detection and monitoring of visual impairments.