This document discusses methodology for lipid profile analysis, including cholesterol, lipoproteins, triglycerides, and apolipoproteins. It covers pre-analytical considerations for specimen collection and storage, as well as analytical methods such as enzymatic, chemical, and electrophoretic techniques. Cholesterol is measured using enzymatic cholesterol oxidase or chemical Liebermann-Burchardt reactions. Lipoproteins are separated by polyanion precipitation, electrophoresis, or ultracentrifugation. Triglycerides are analyzed chemically or enzymatically using glycerol kinase. Quality control is also important in lipid analysis.









![LDL–C Estimation
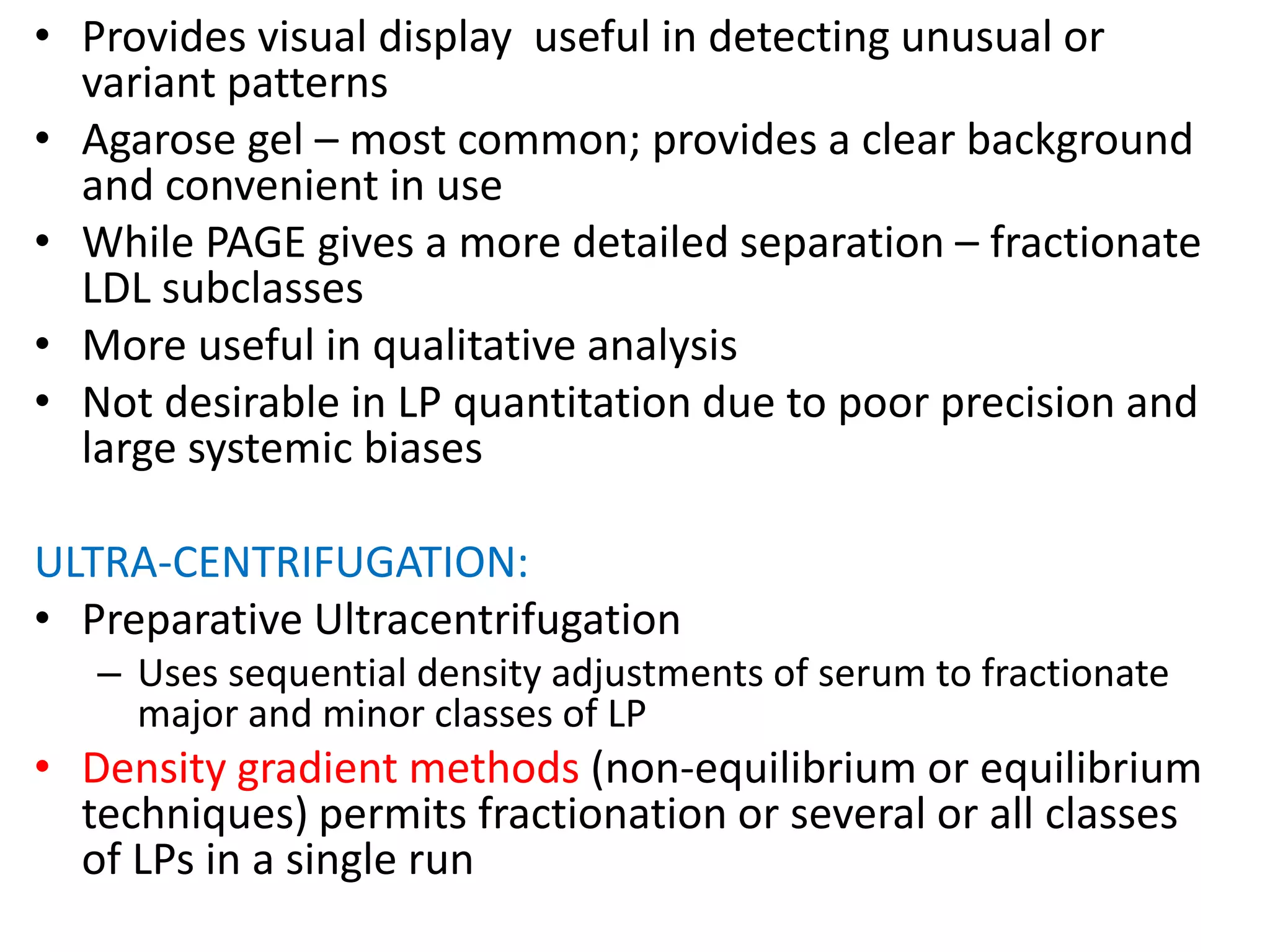
INDIRECT METHODS:
• Fridewald Equation(Calculation Method) – Routine.
– LDL–Chol(mmol/L) = [TC – HDL-Chol] – Plasma TG/2.175;
or, LDL-Chol(mg/dL) = [TC – HDL-Chol] – Plasma TG/5
• VLDL (mg/dL) = [TAG]/5 or VLDL (mmol/L) = [TAG]/2.175
• The factor [TAG]/5 is an estimate of the VLDL cholesterol and is
based on the average ratio of triglyceride to cholesterol in VLDL
• Equation assumes patient fasted and plasma [TAG] does not
exceed 5.0mmol/L
– Limitations: not appropriate in
• Samples with TG > 400mg/dL
• Patients with suspected Dysbetalipoproteinaemia
– Other limitations:
• Does not account for cholesterol assosciated with IDL and Lp(a)
• Underestimate LDL-C in chronic alcoholics
• Unsuitable for monitoring
• Mis-classifies 15 – 40 % of patients when TG levels are between
200 to 400 mg/dL](https://image.slidesharecdn.com/lipidsmethodology-160228131059/75/Lipids-methodology-18-2048.jpg)