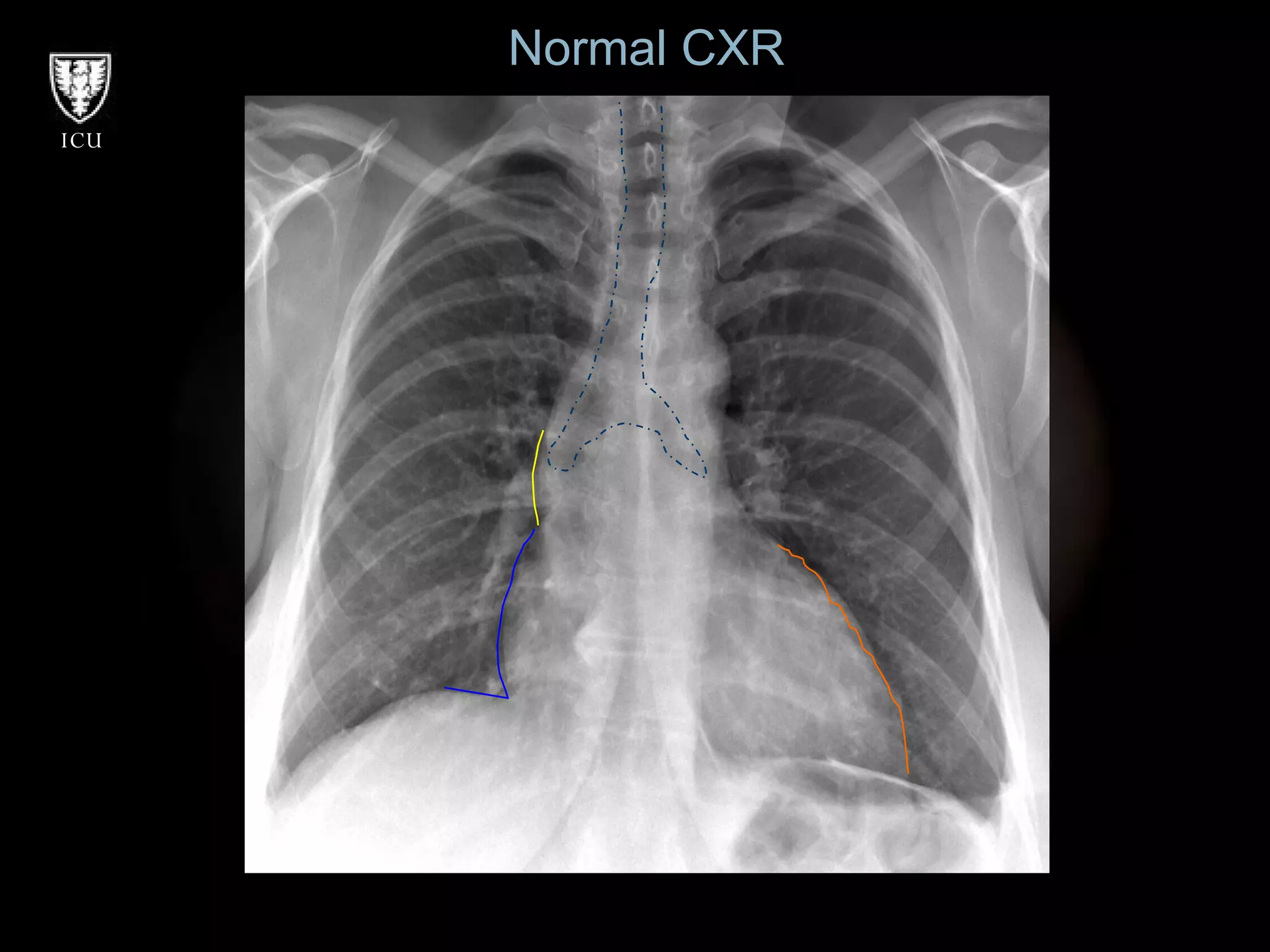
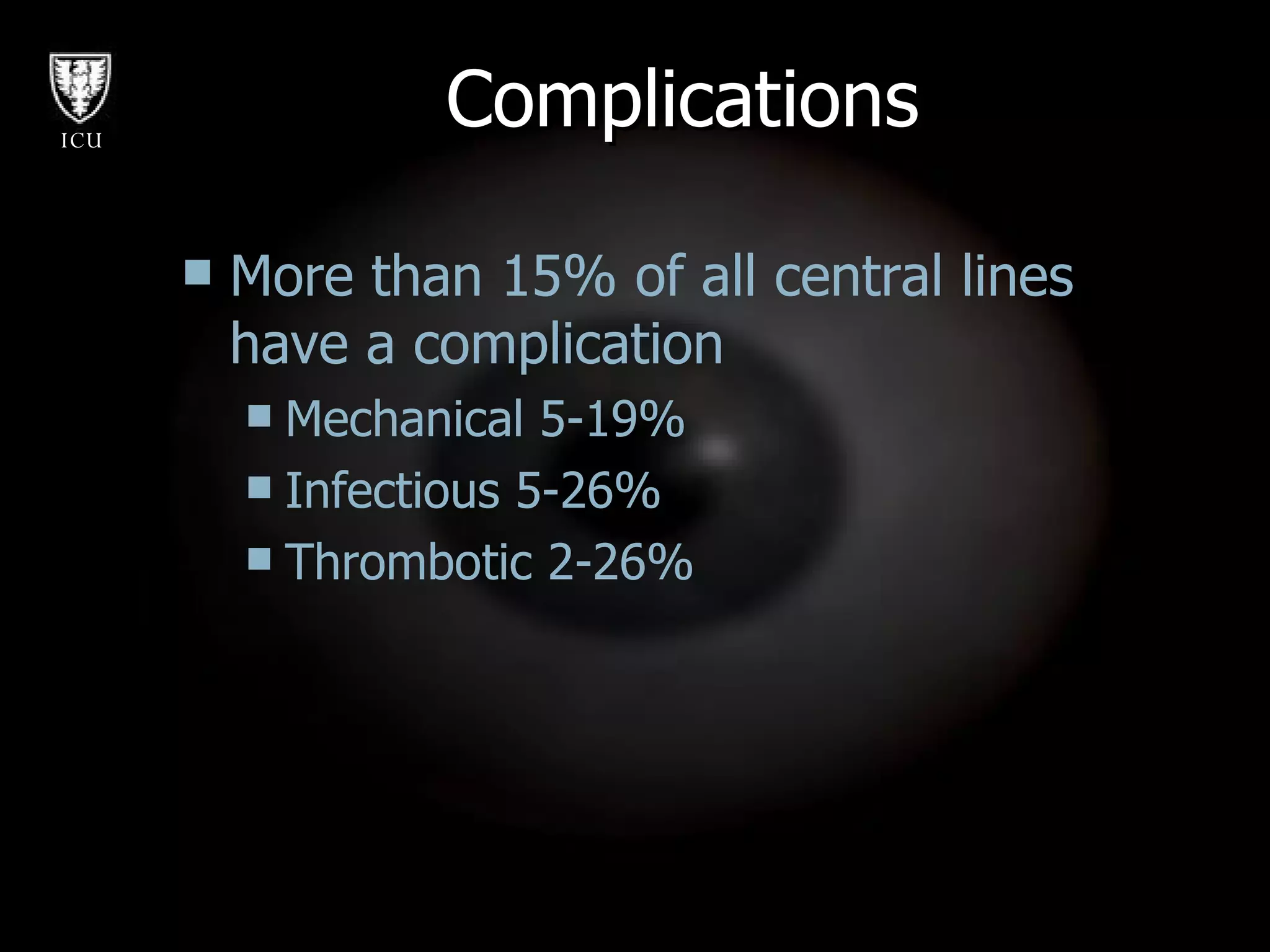
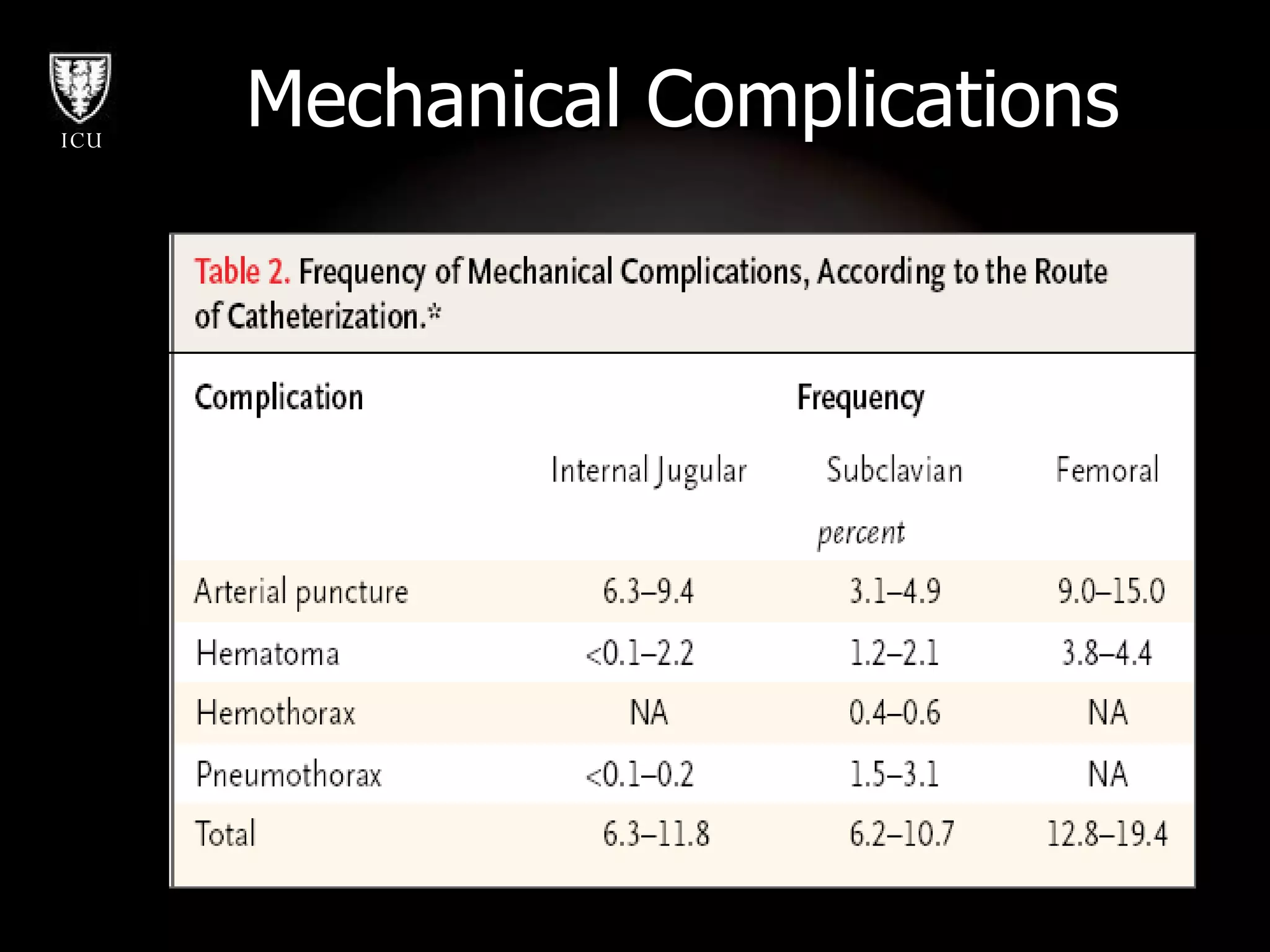
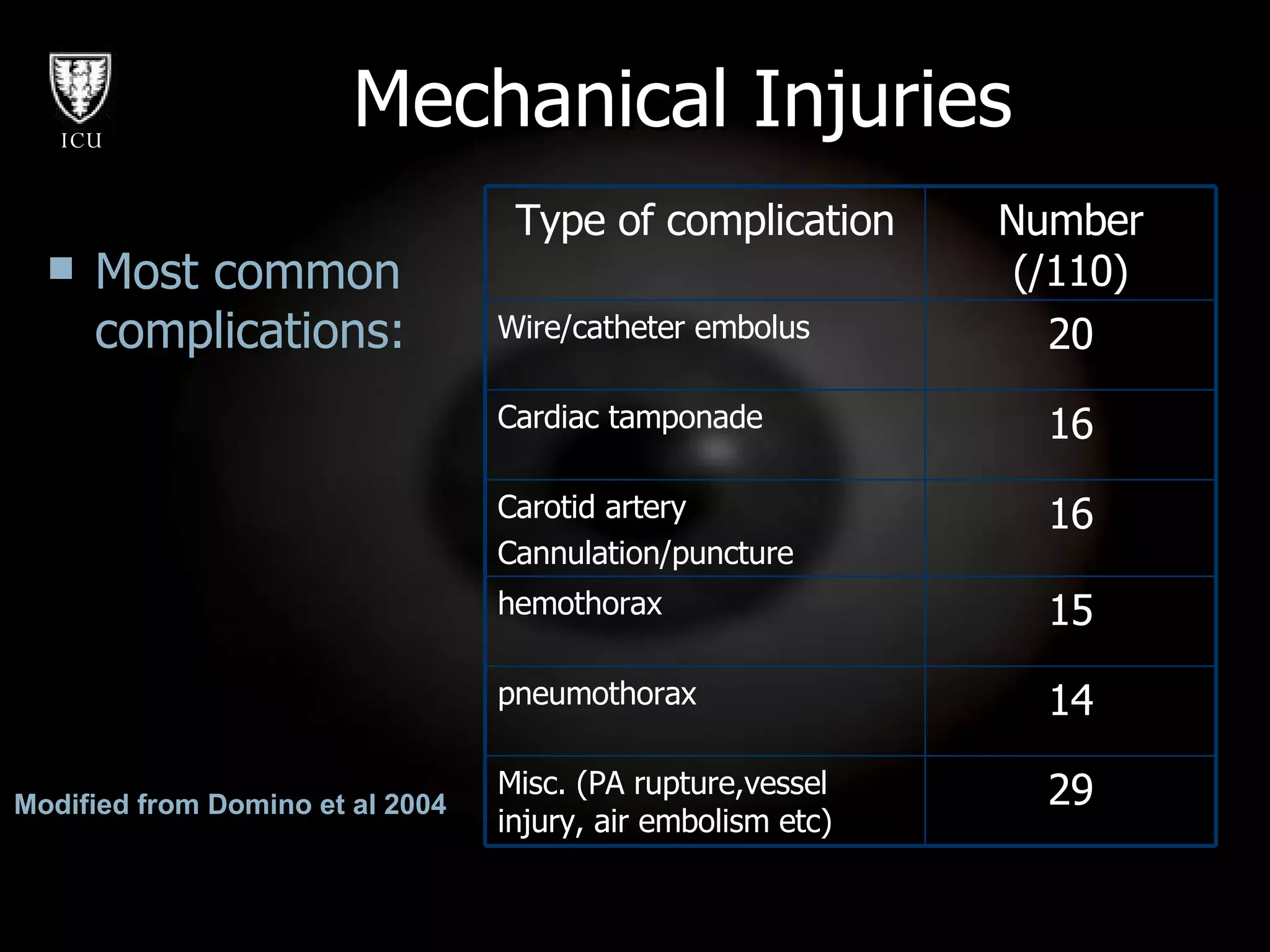
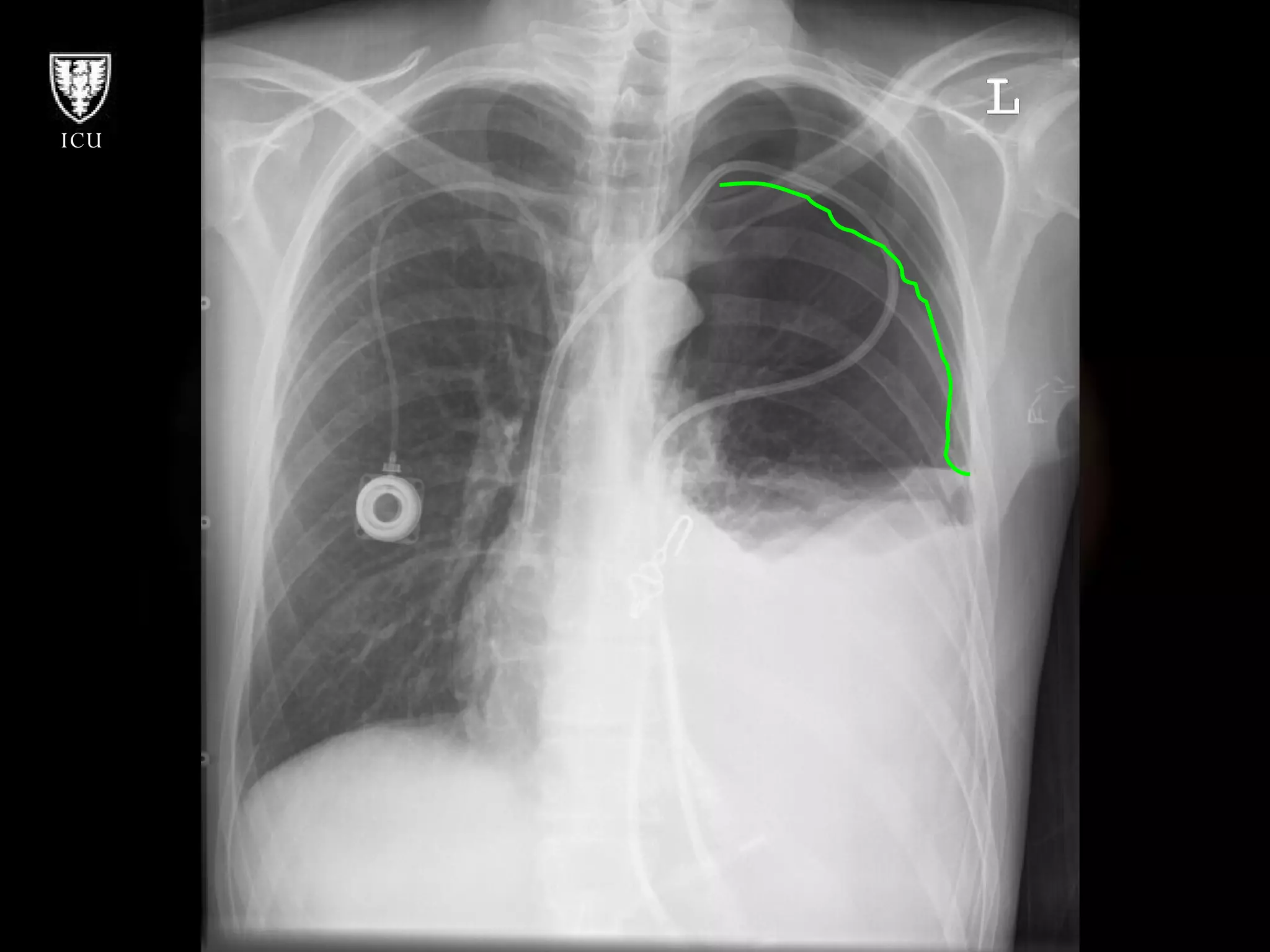
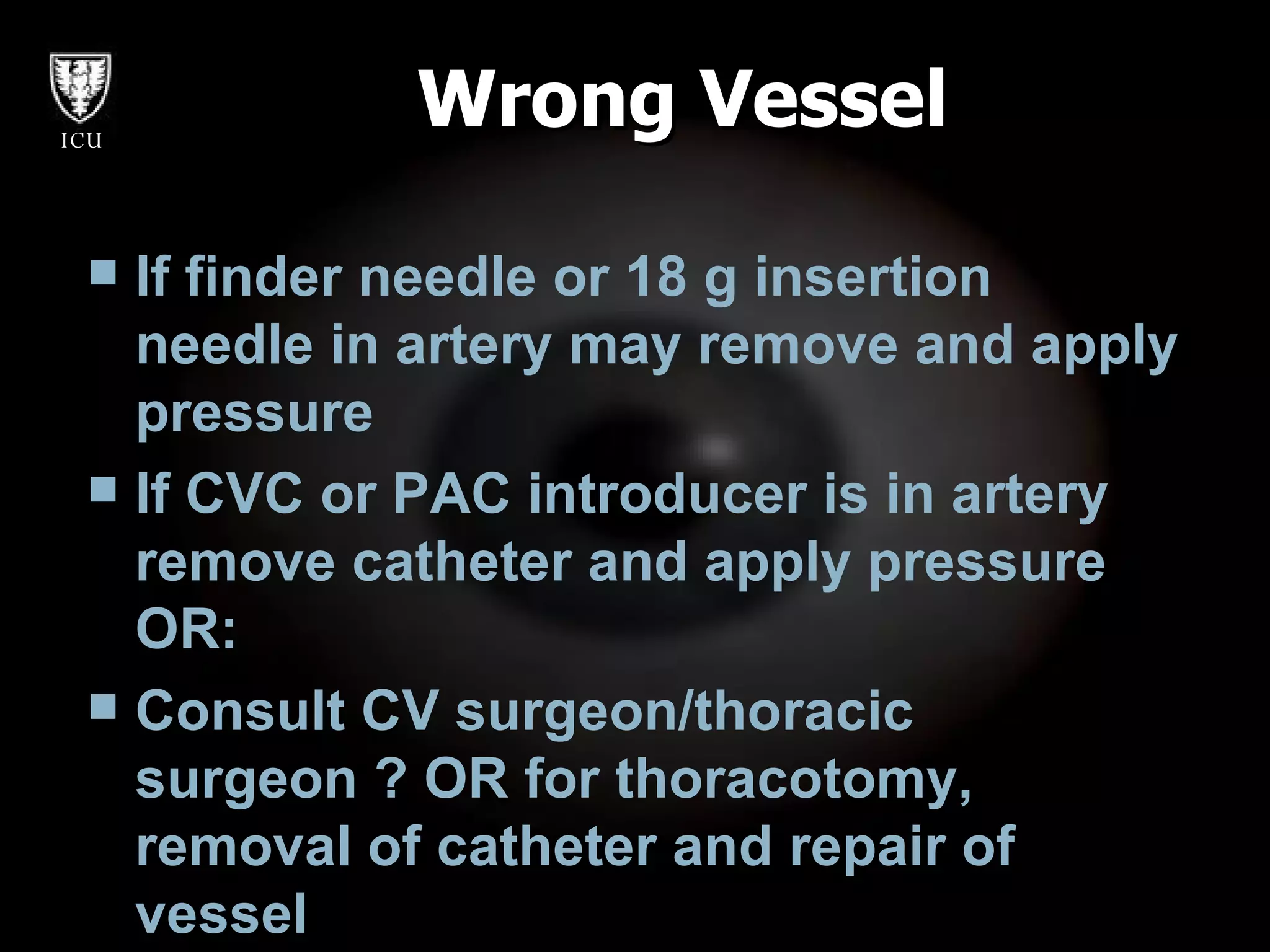
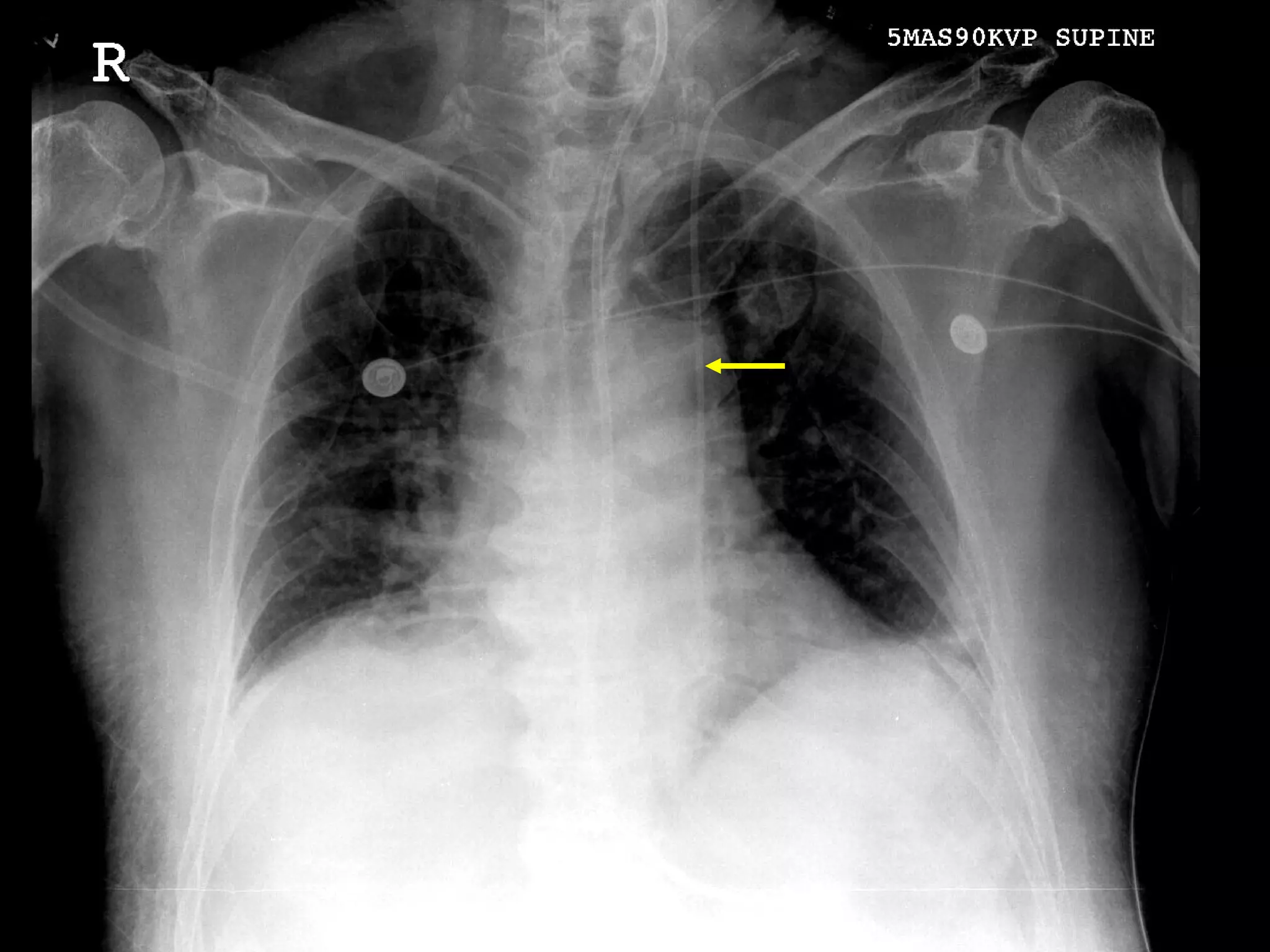
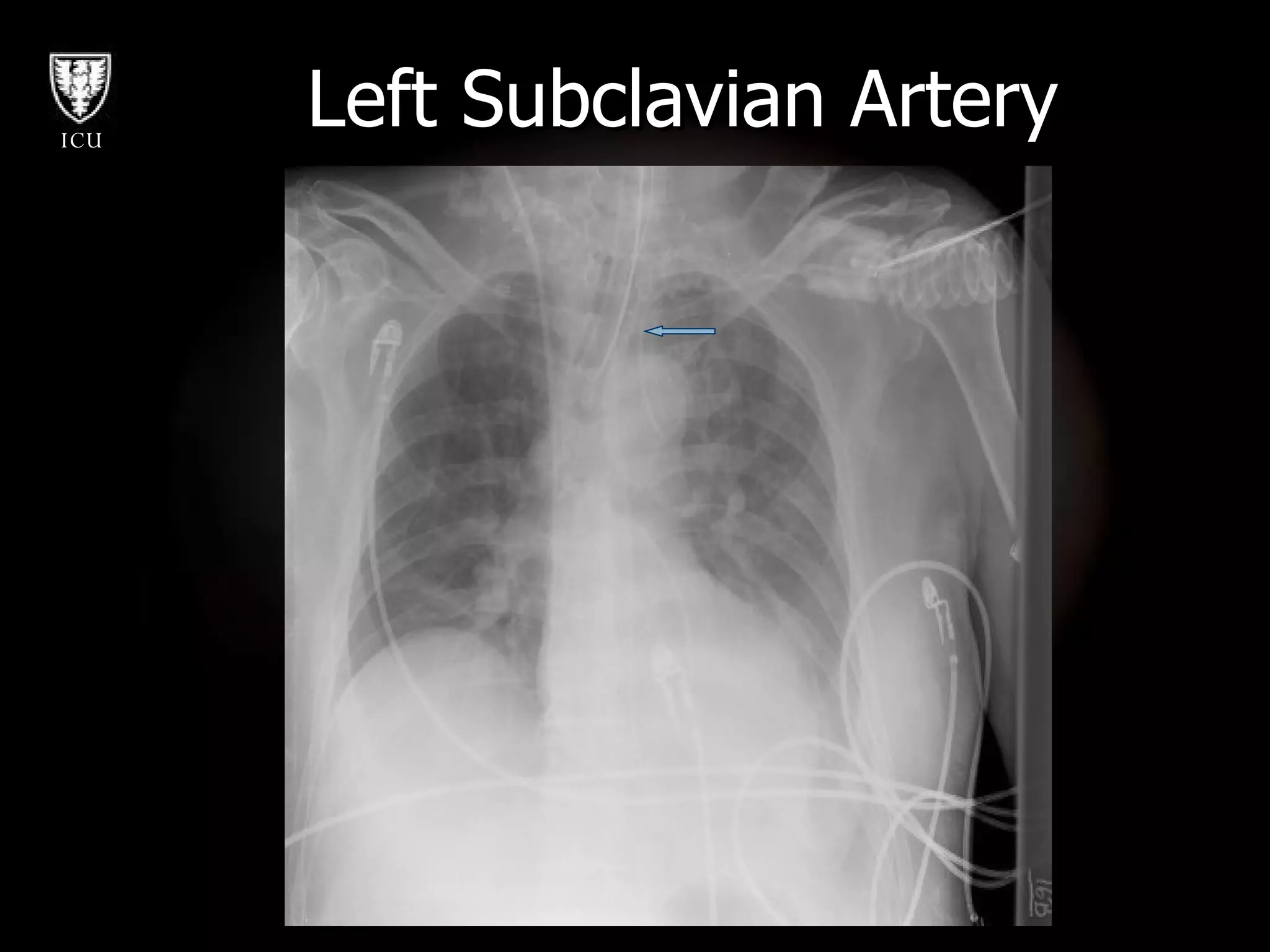
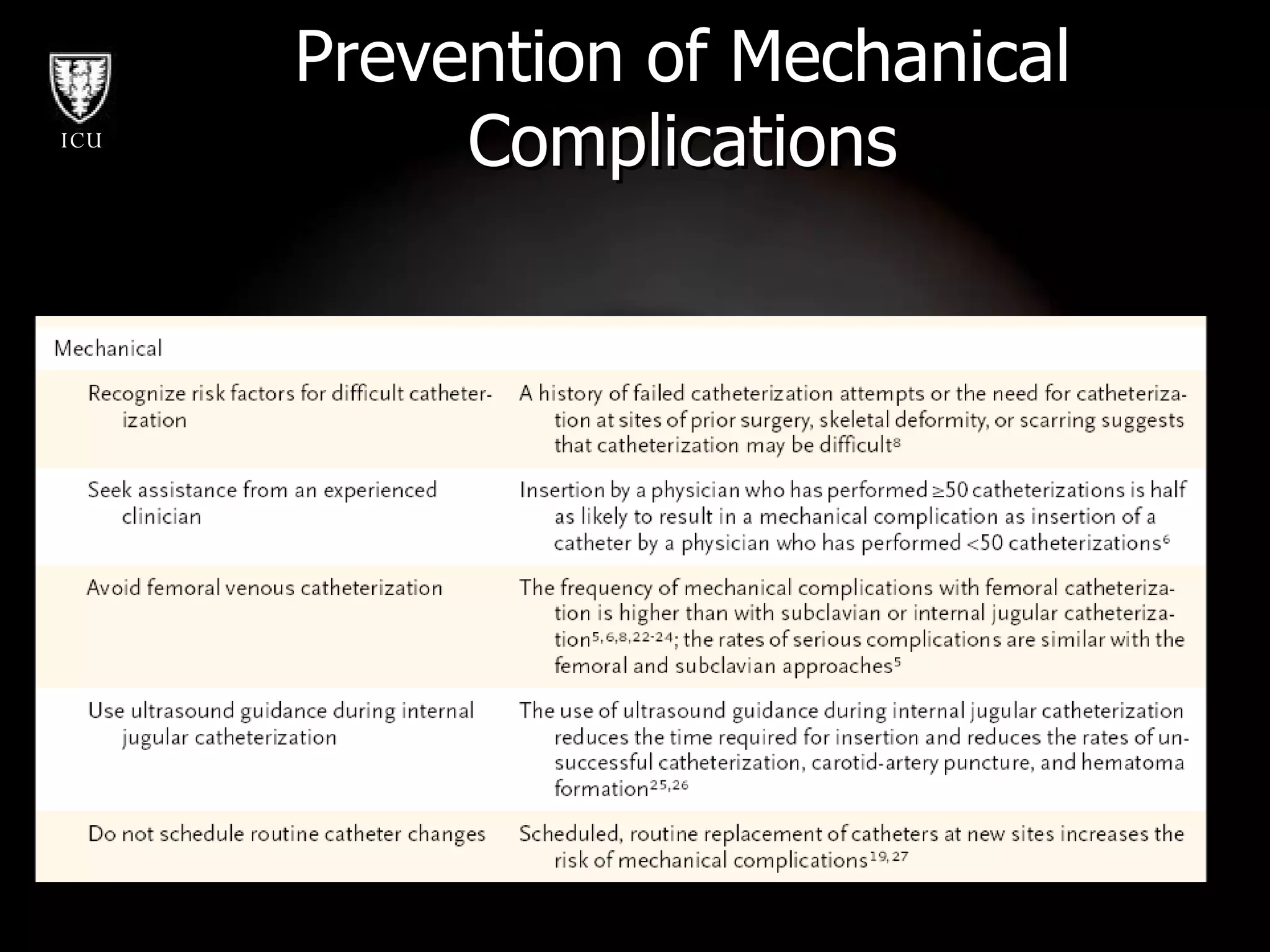
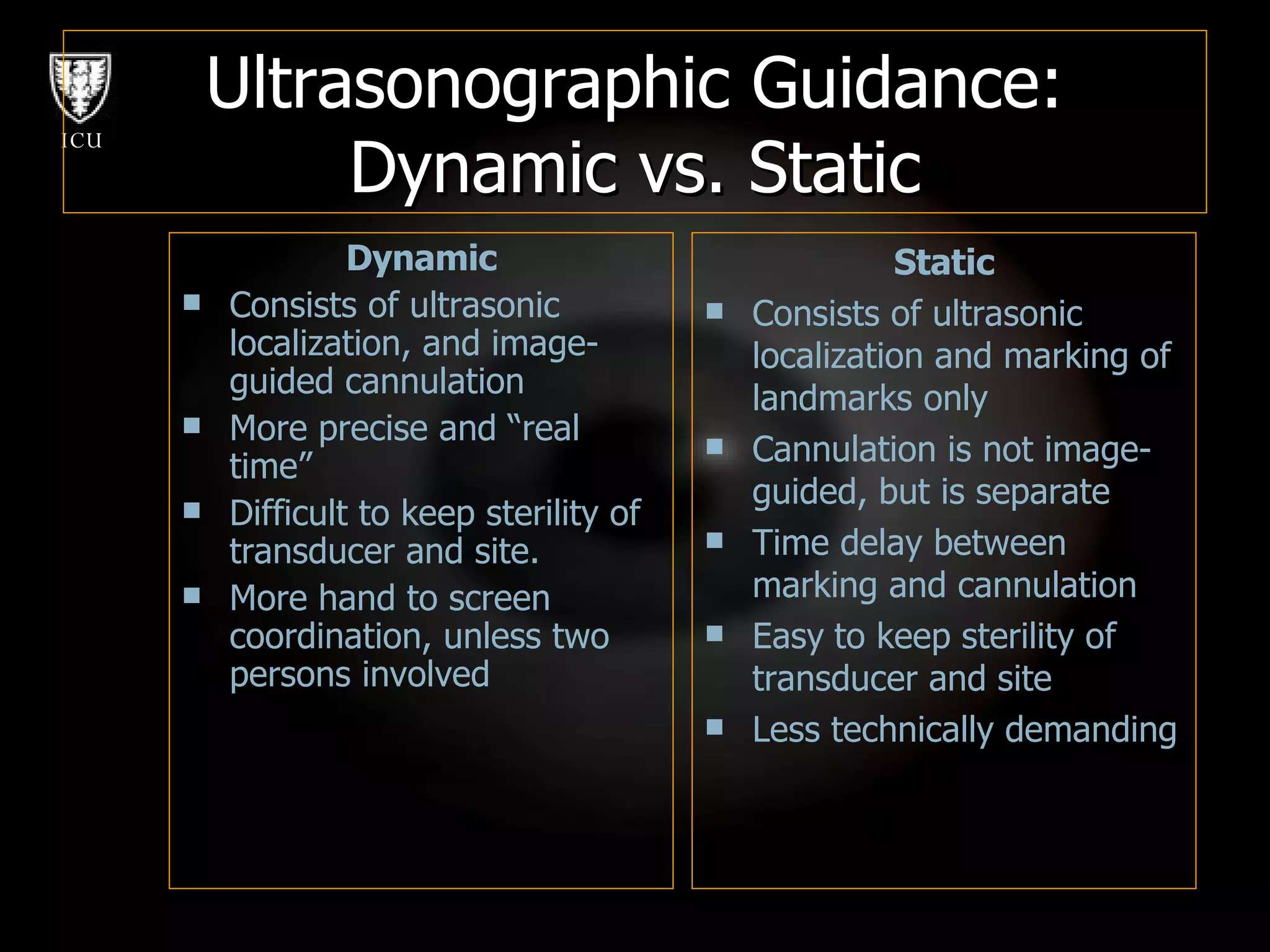
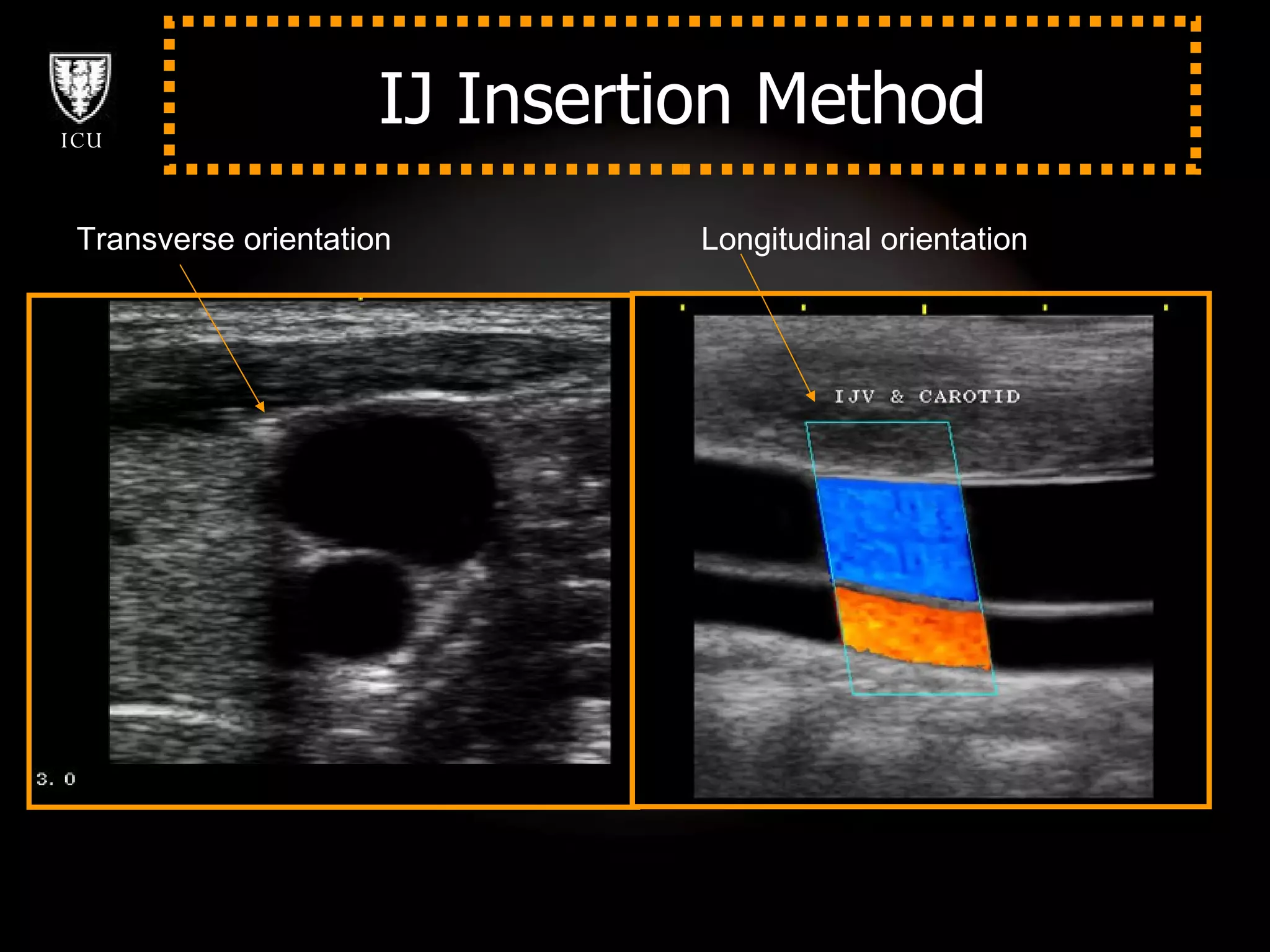
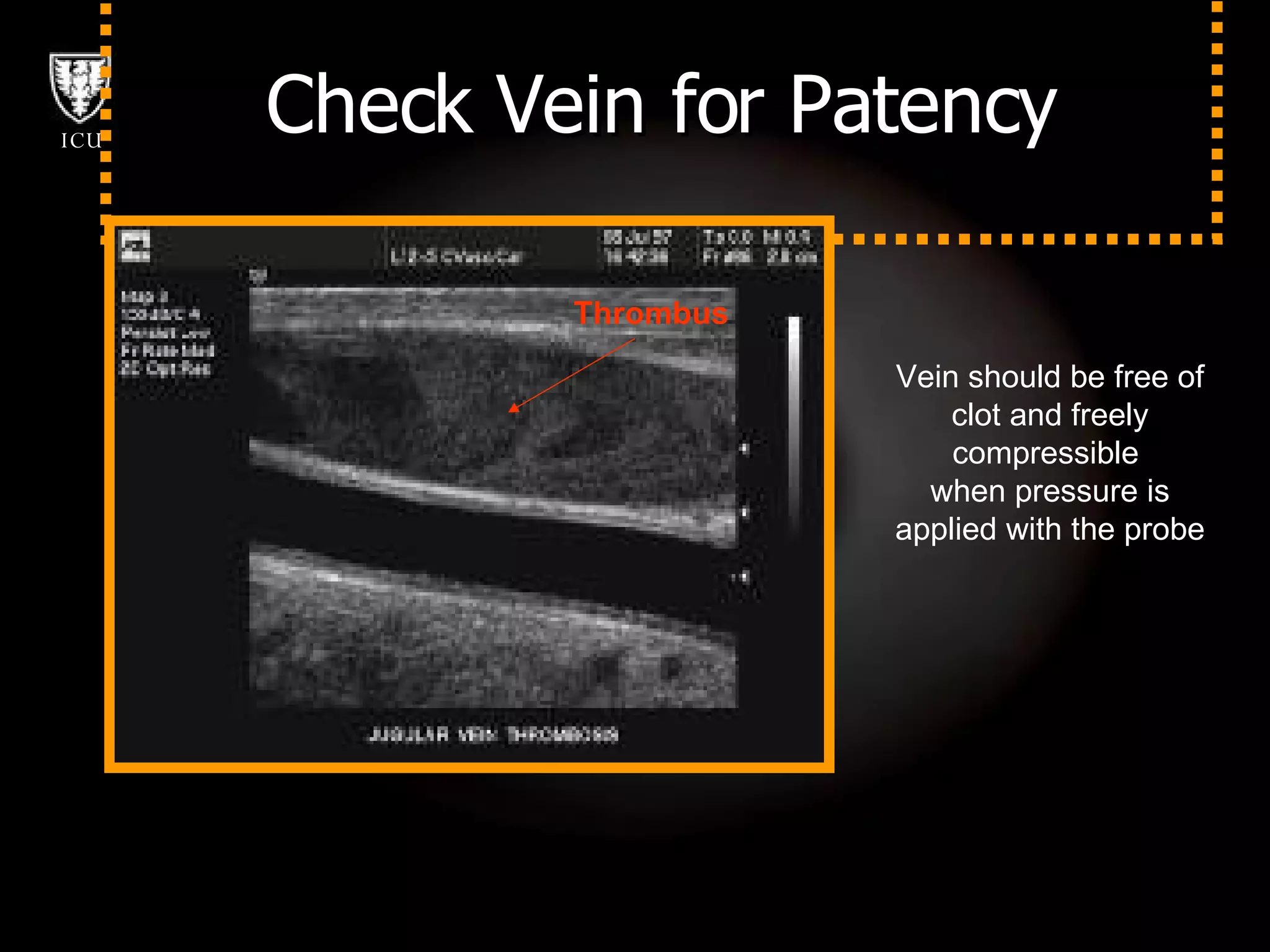
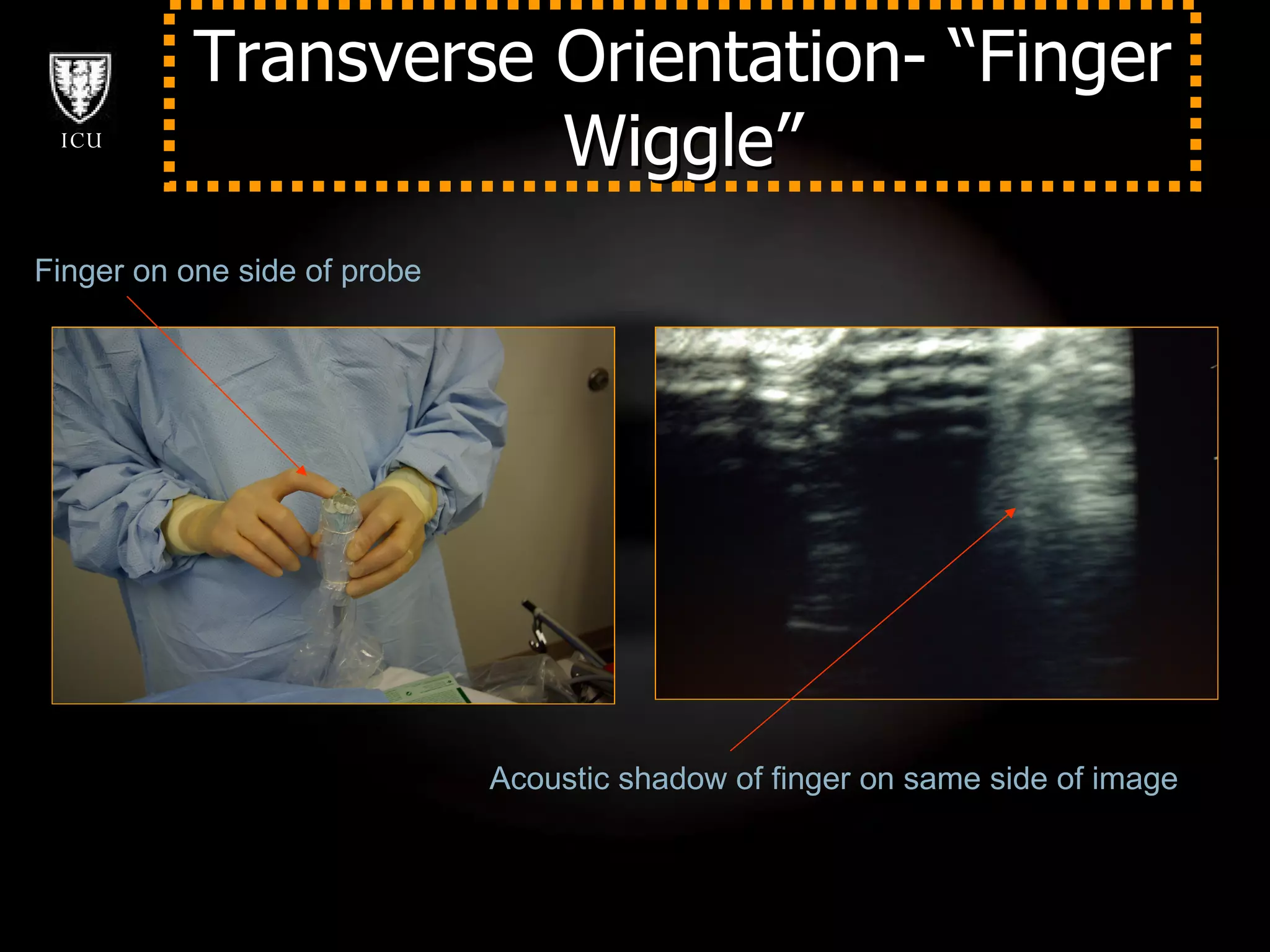
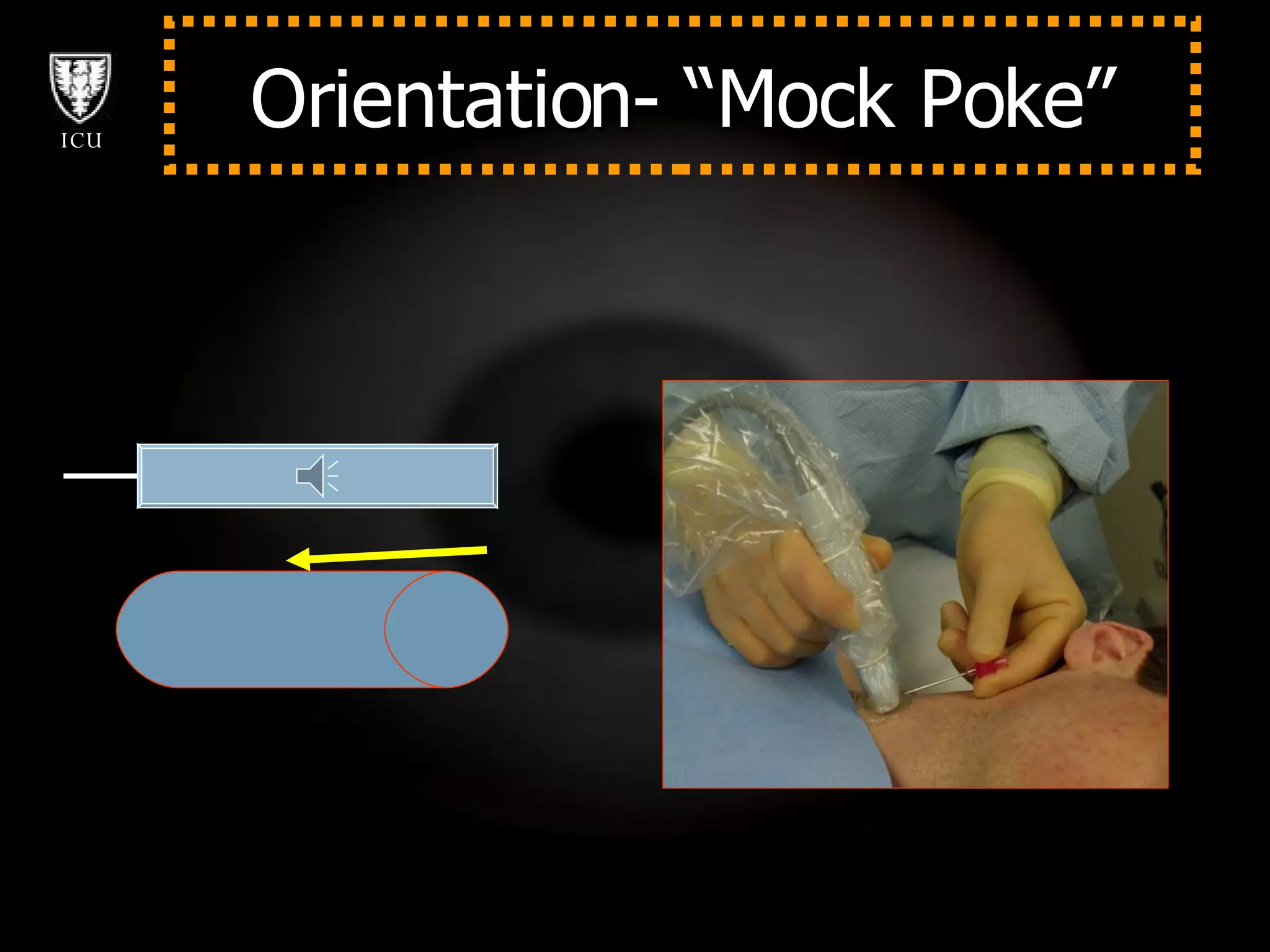
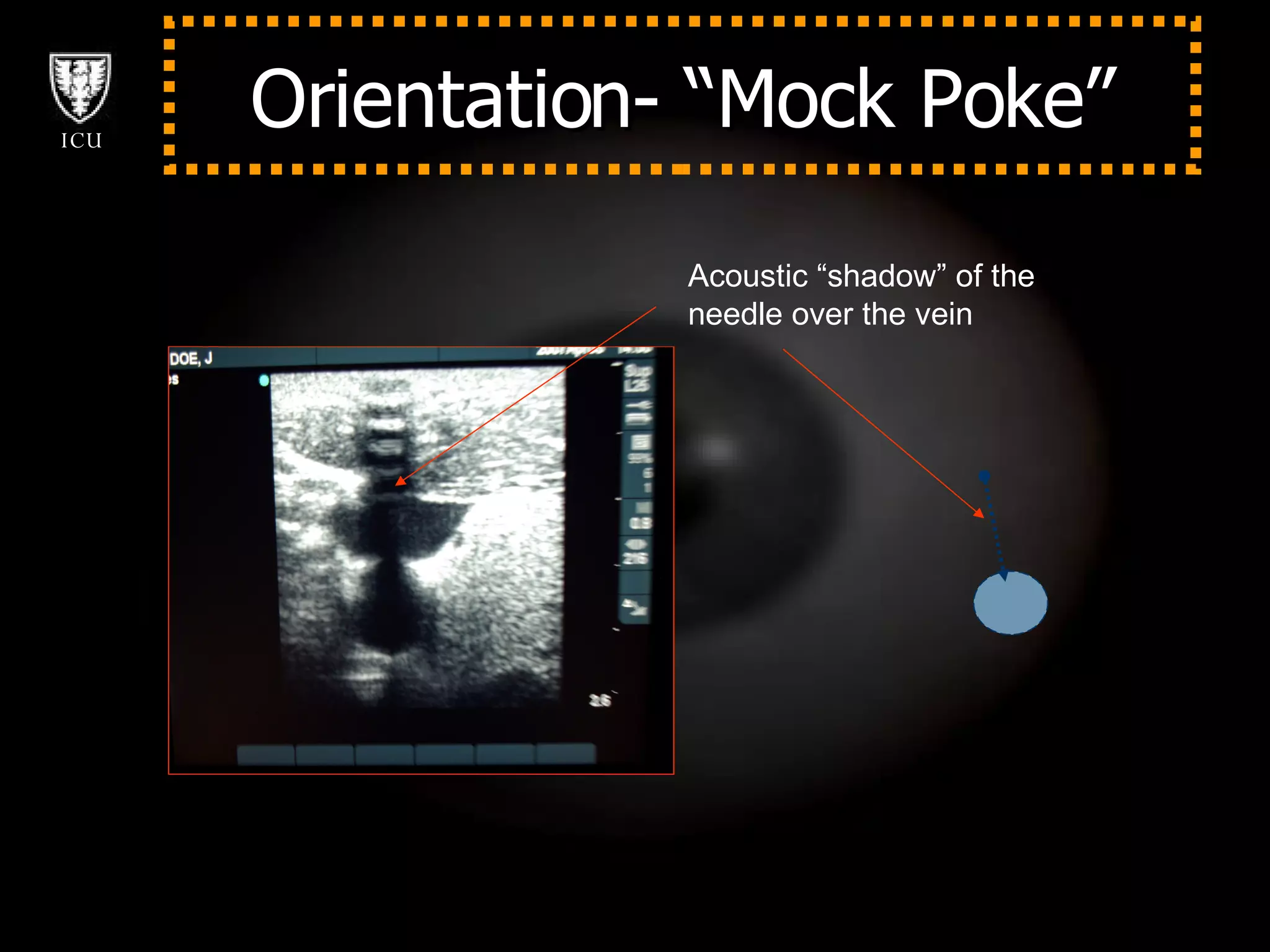
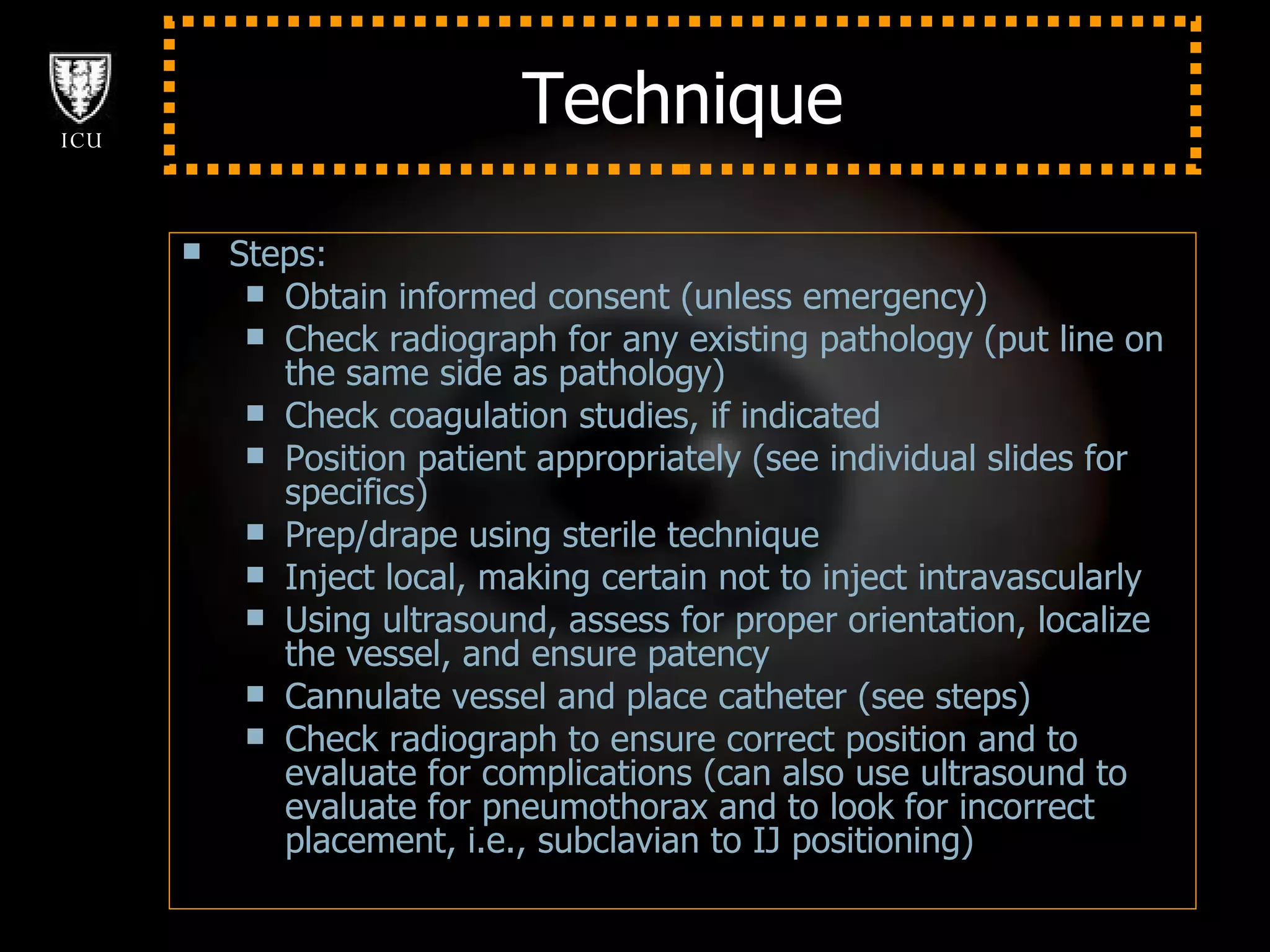
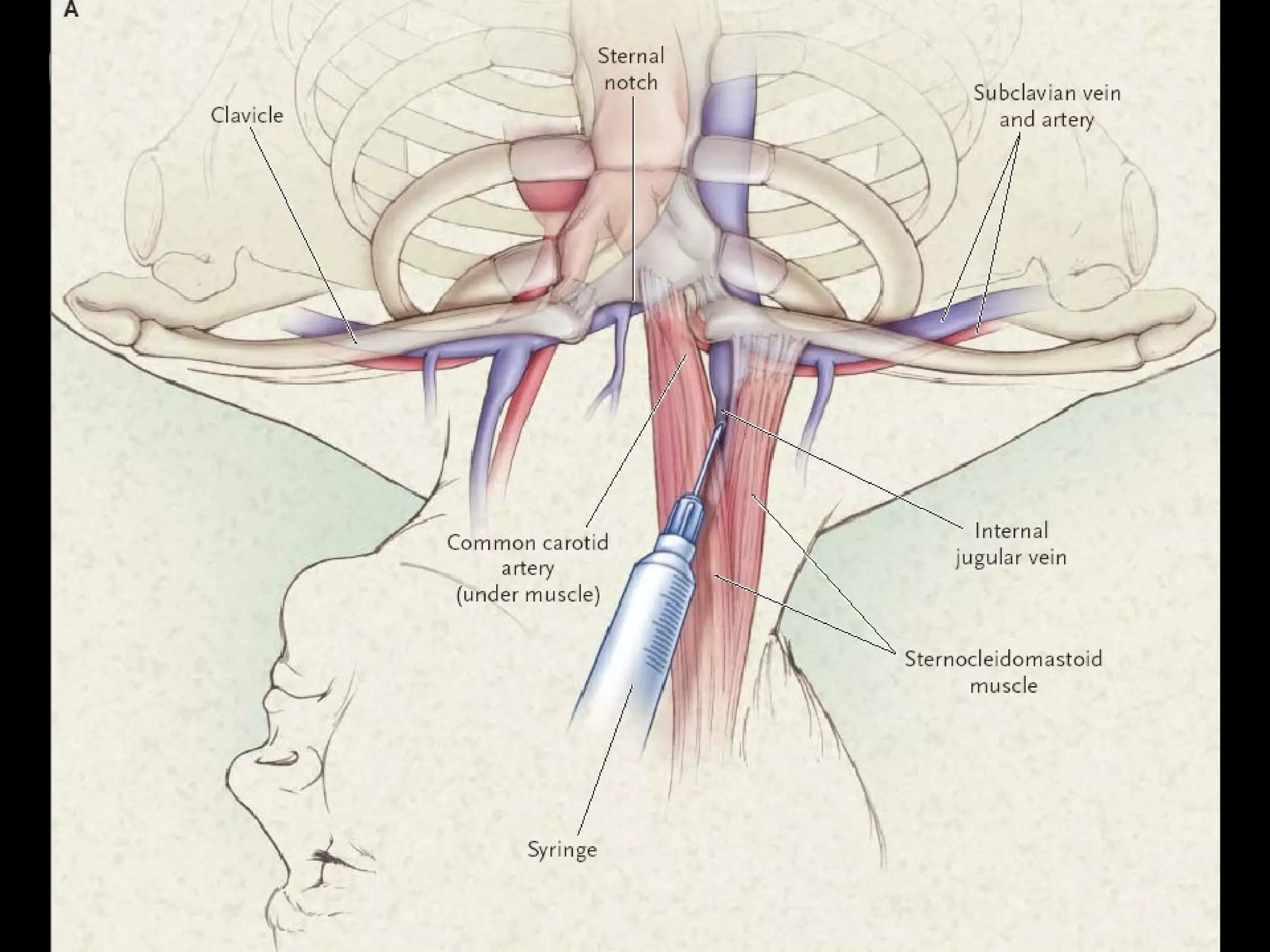
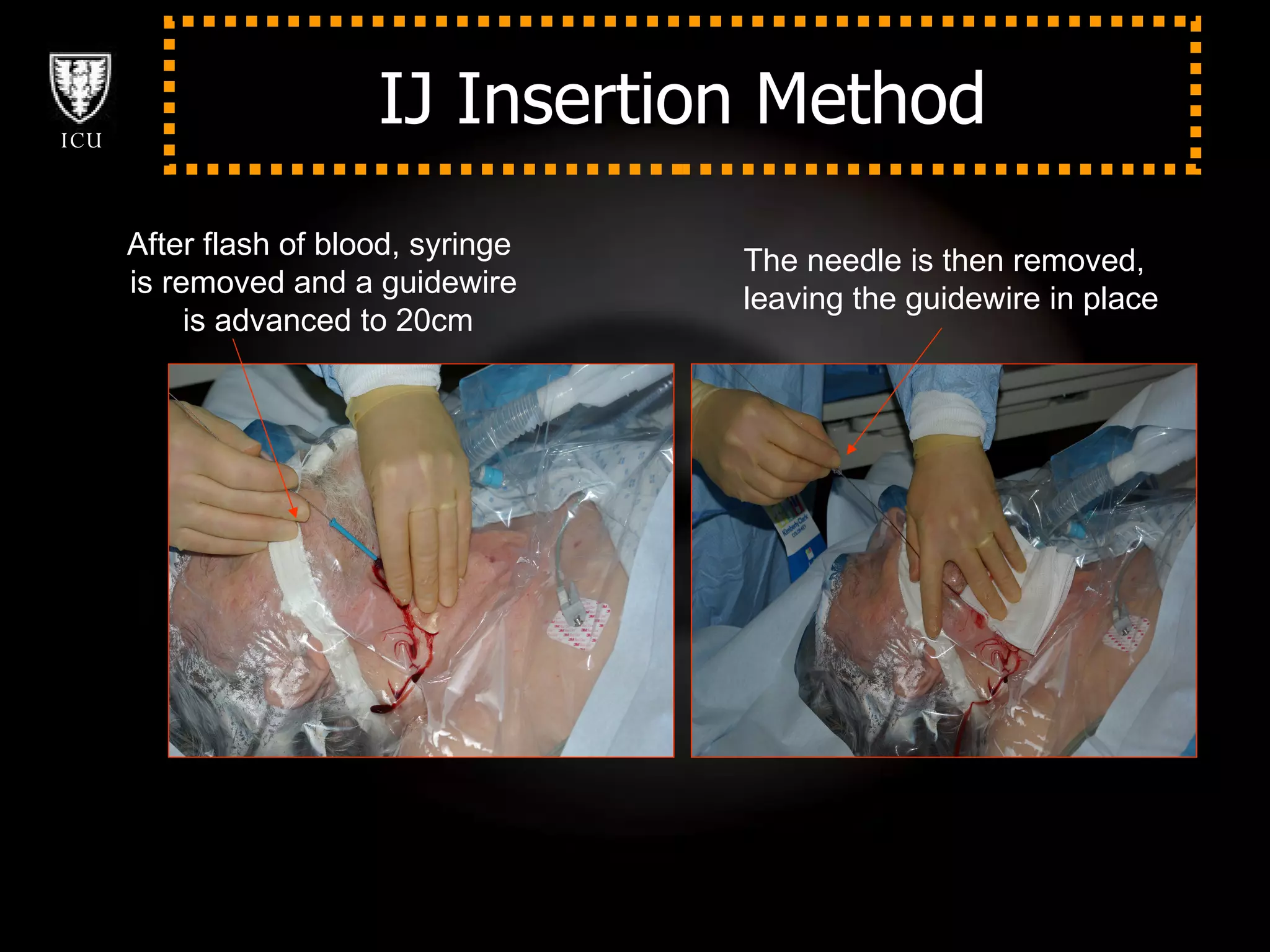
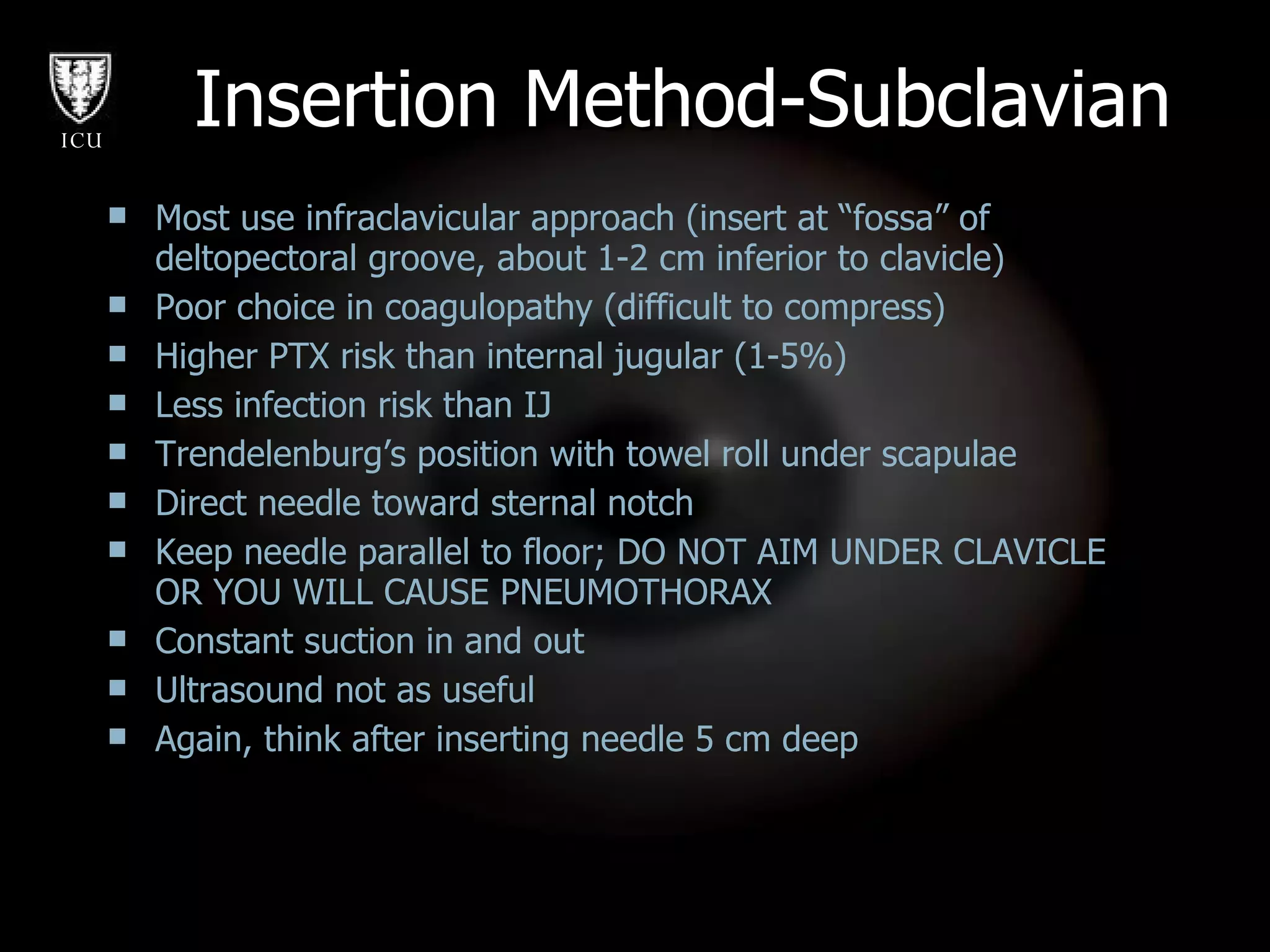
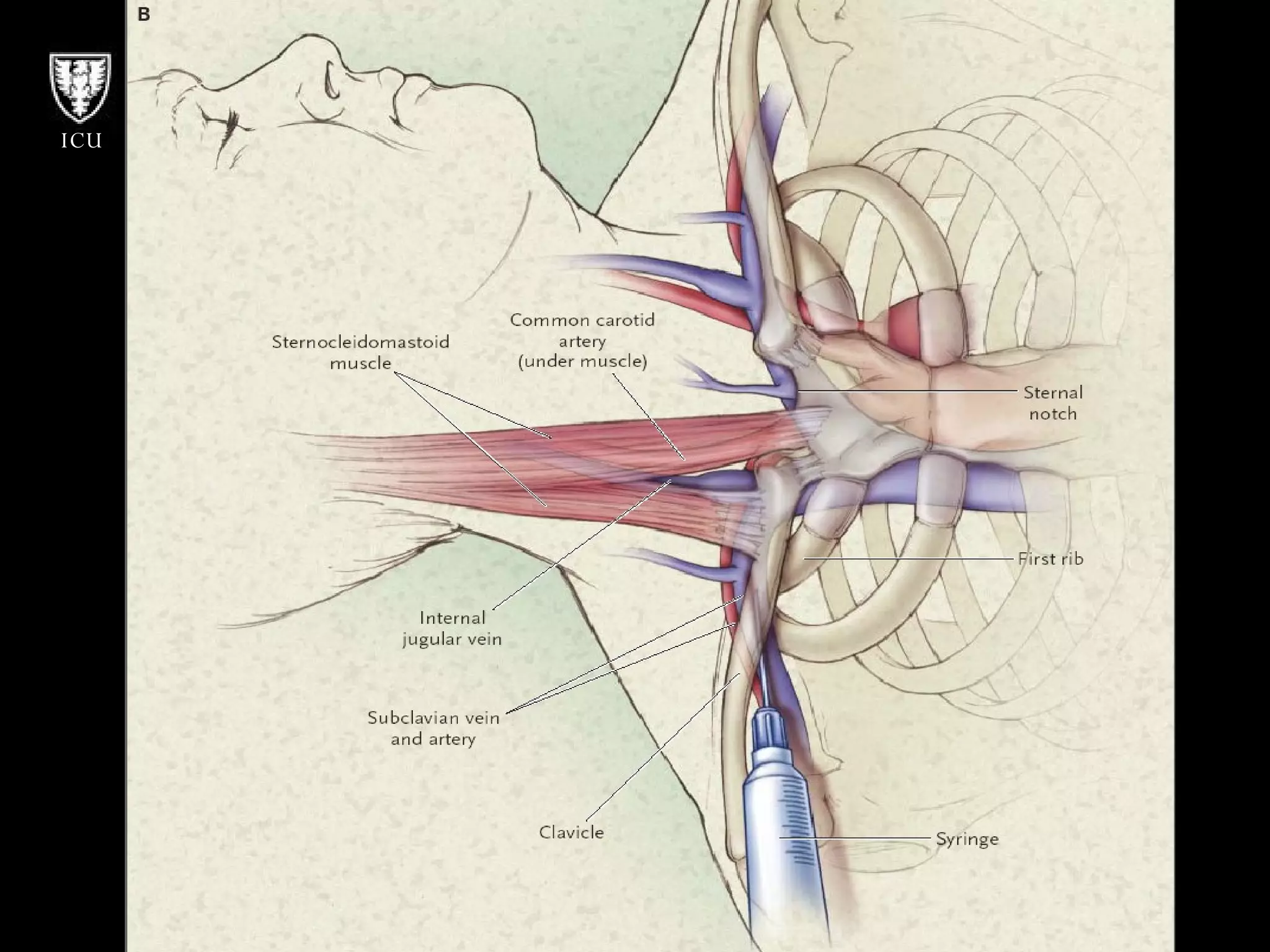
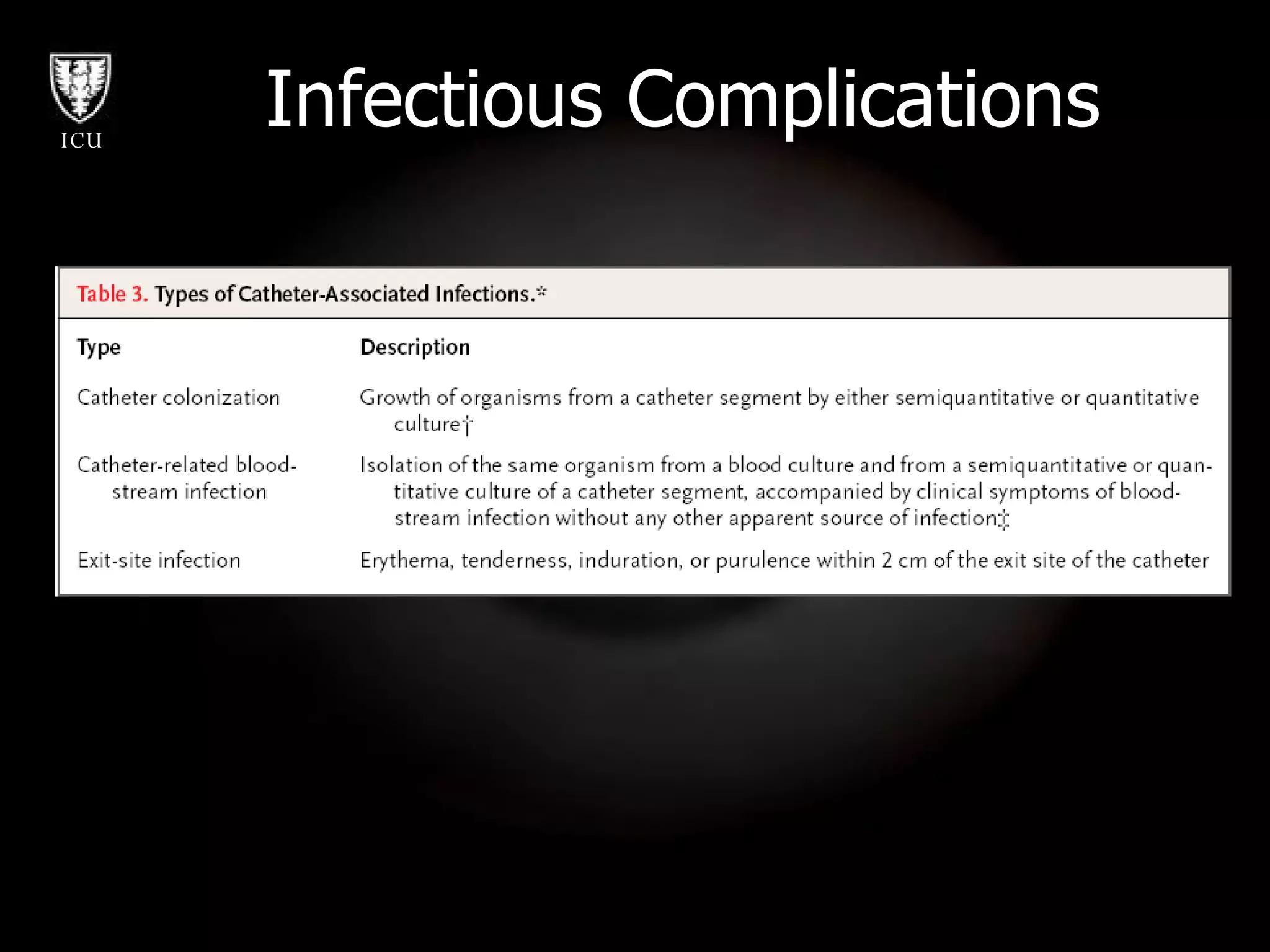
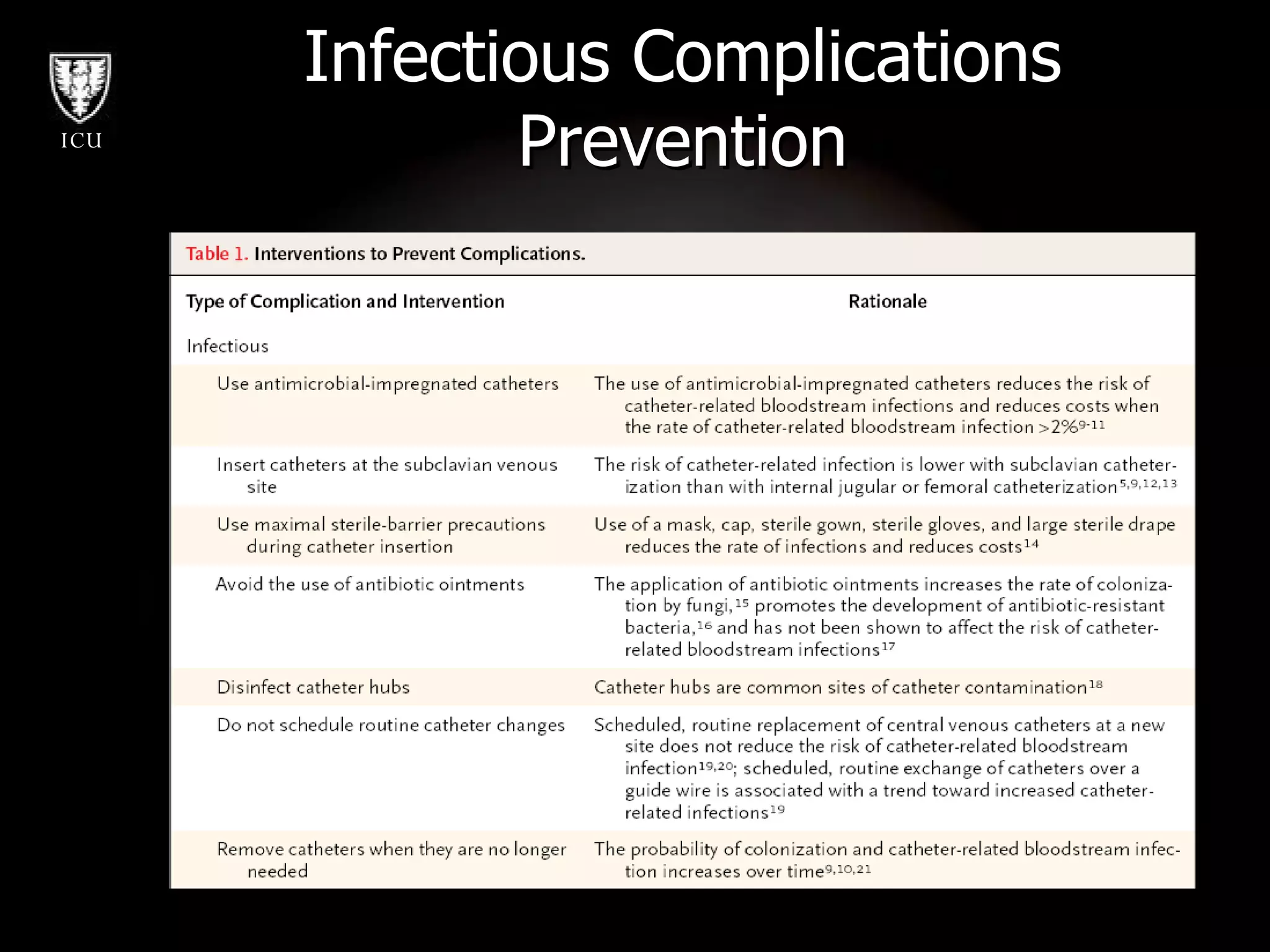
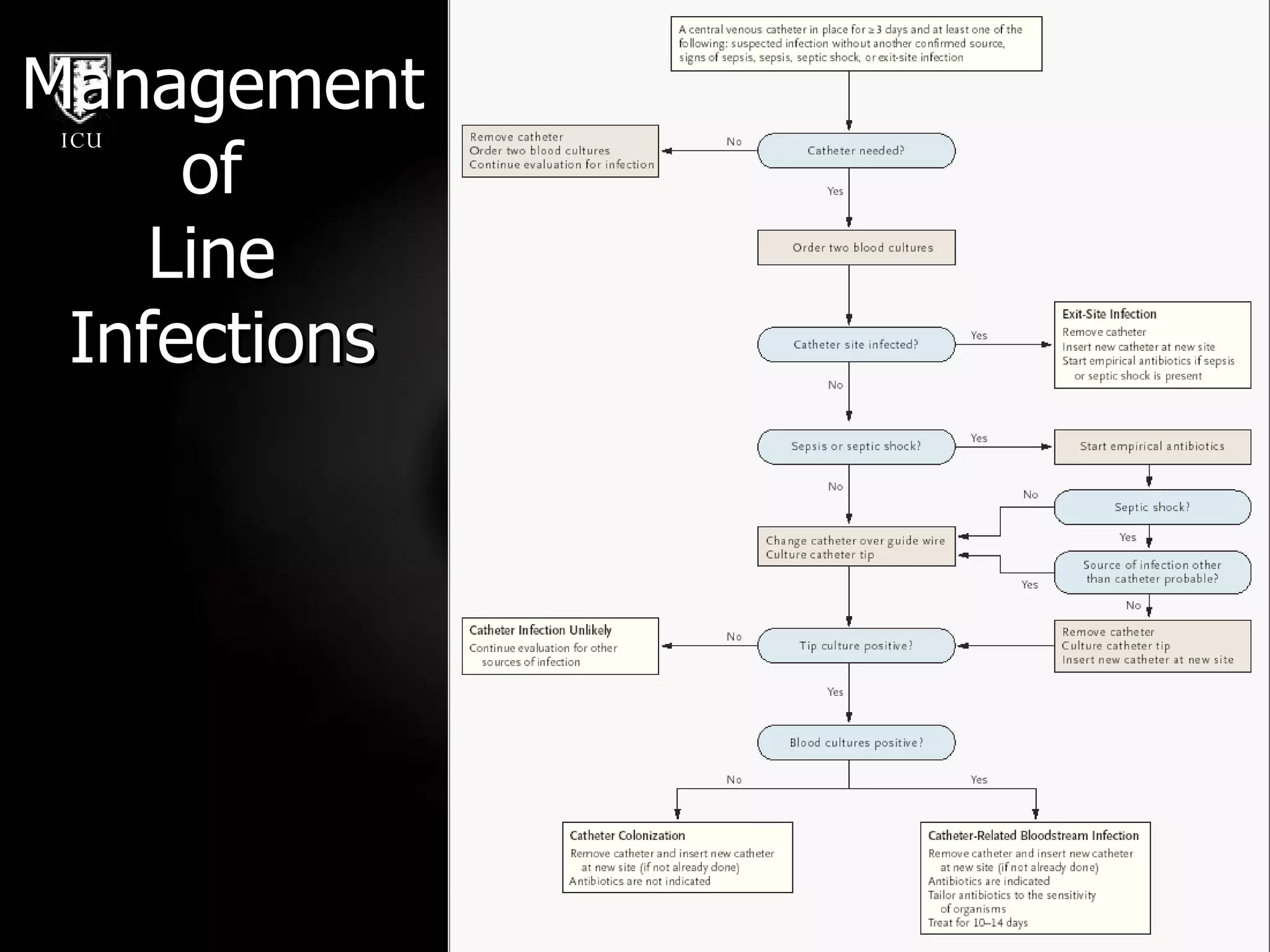
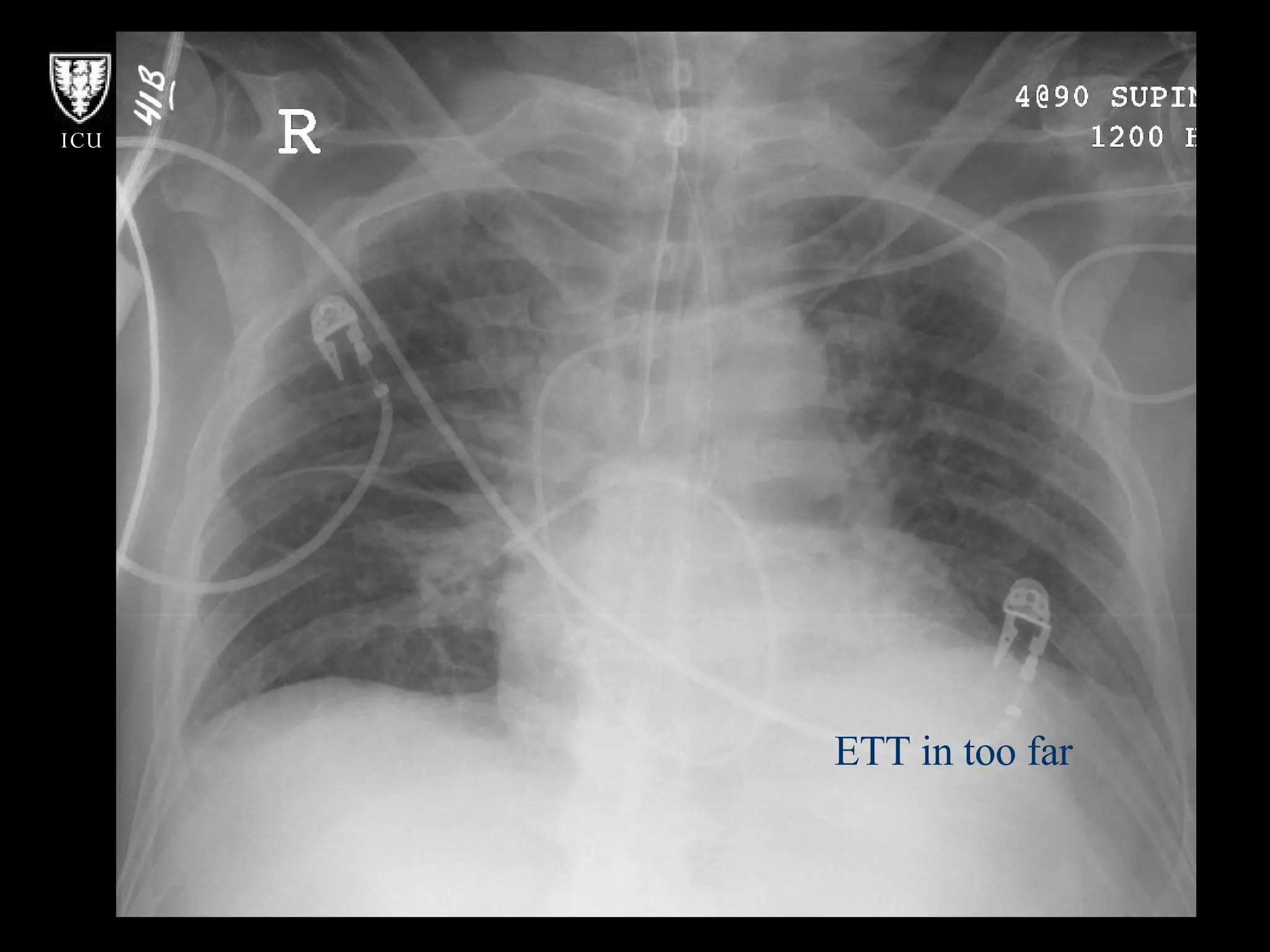
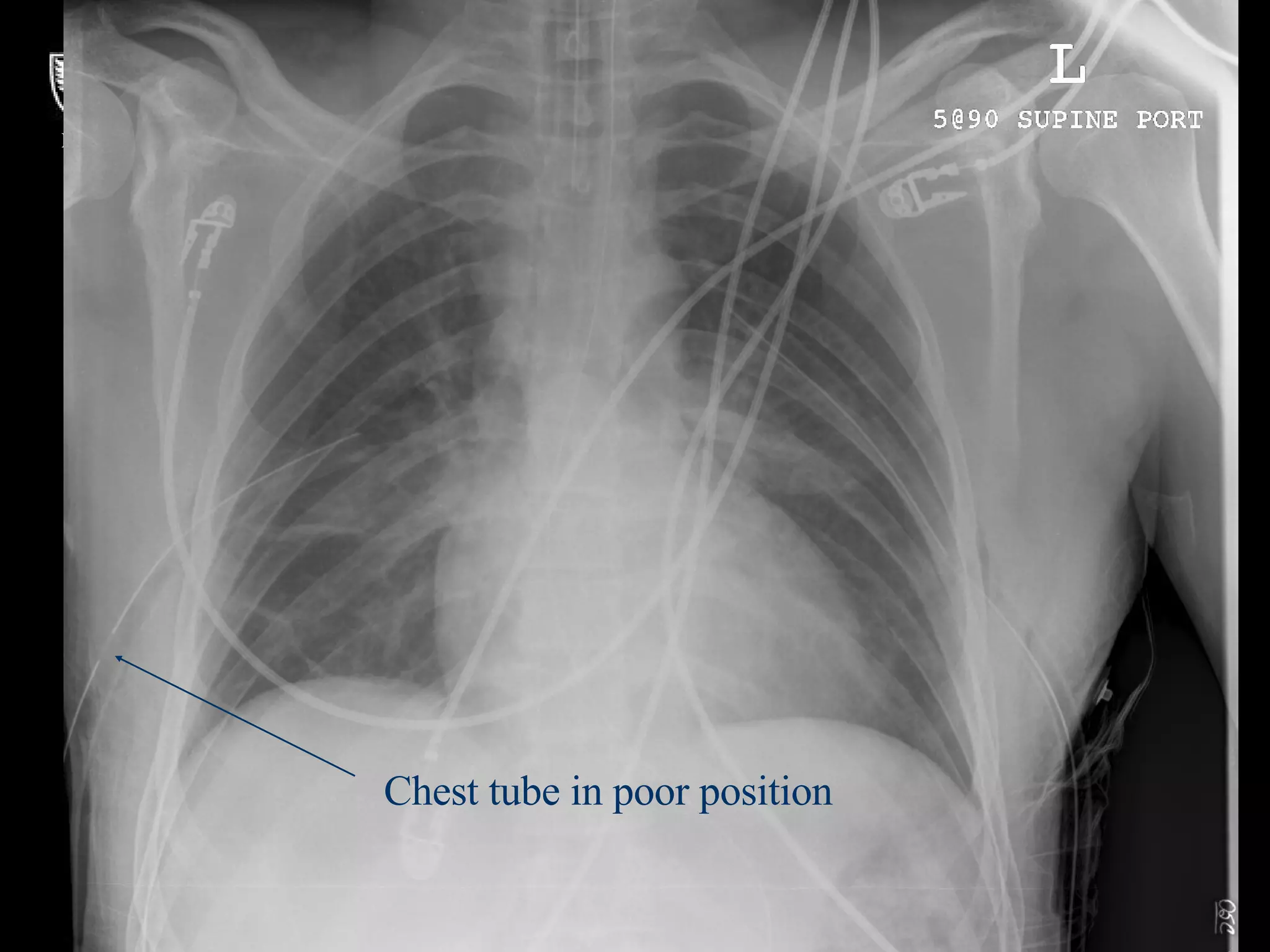
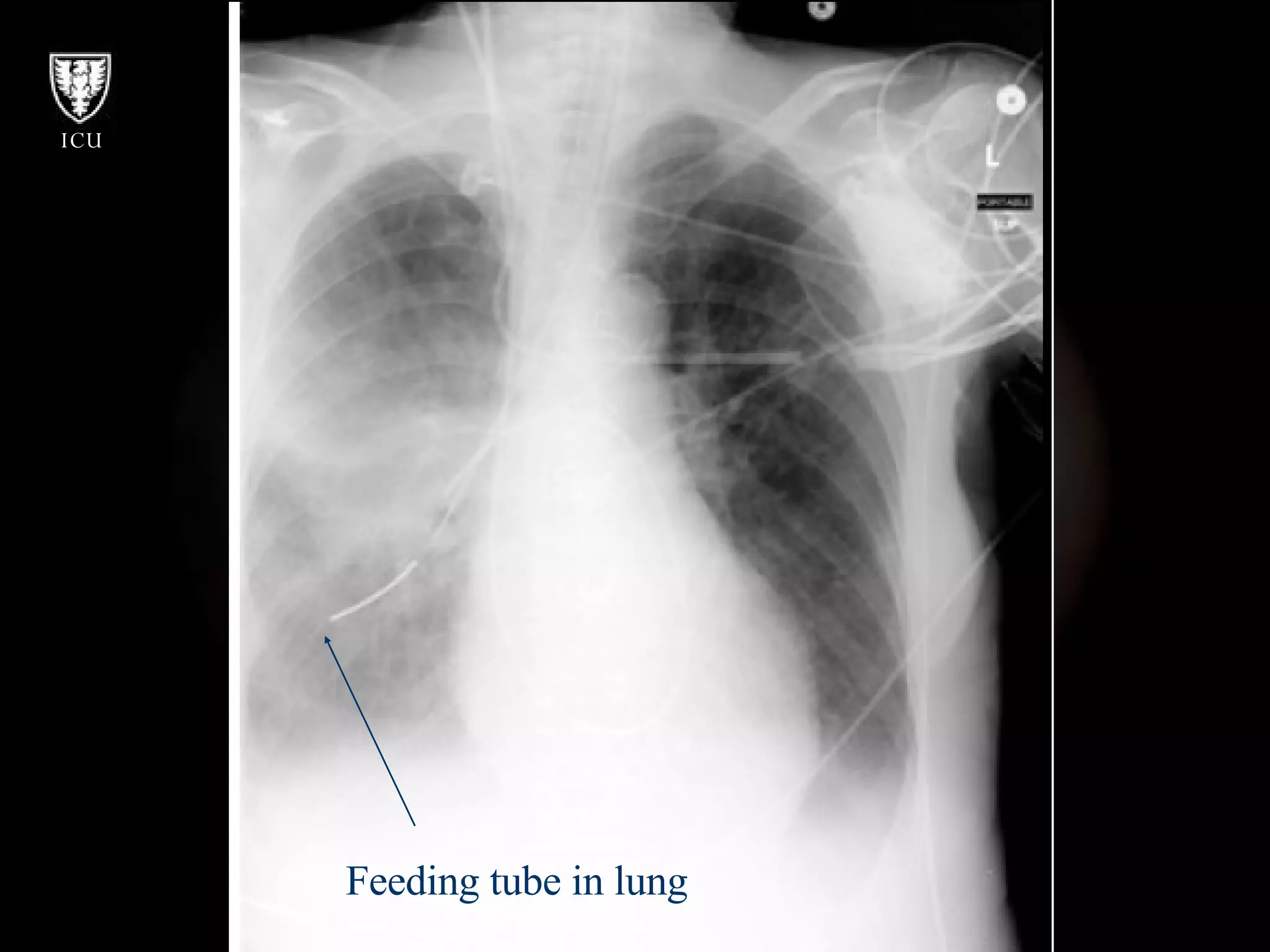
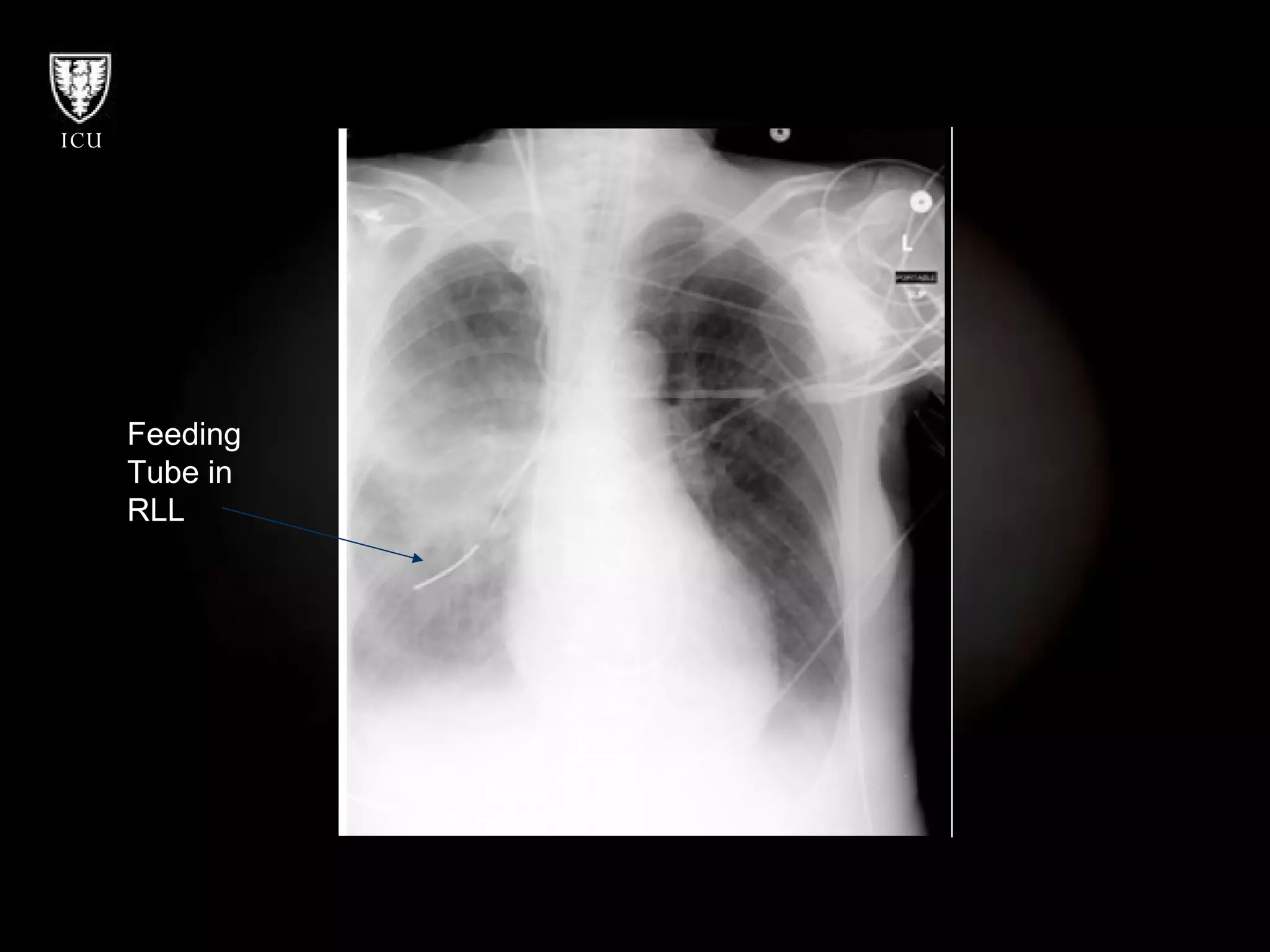
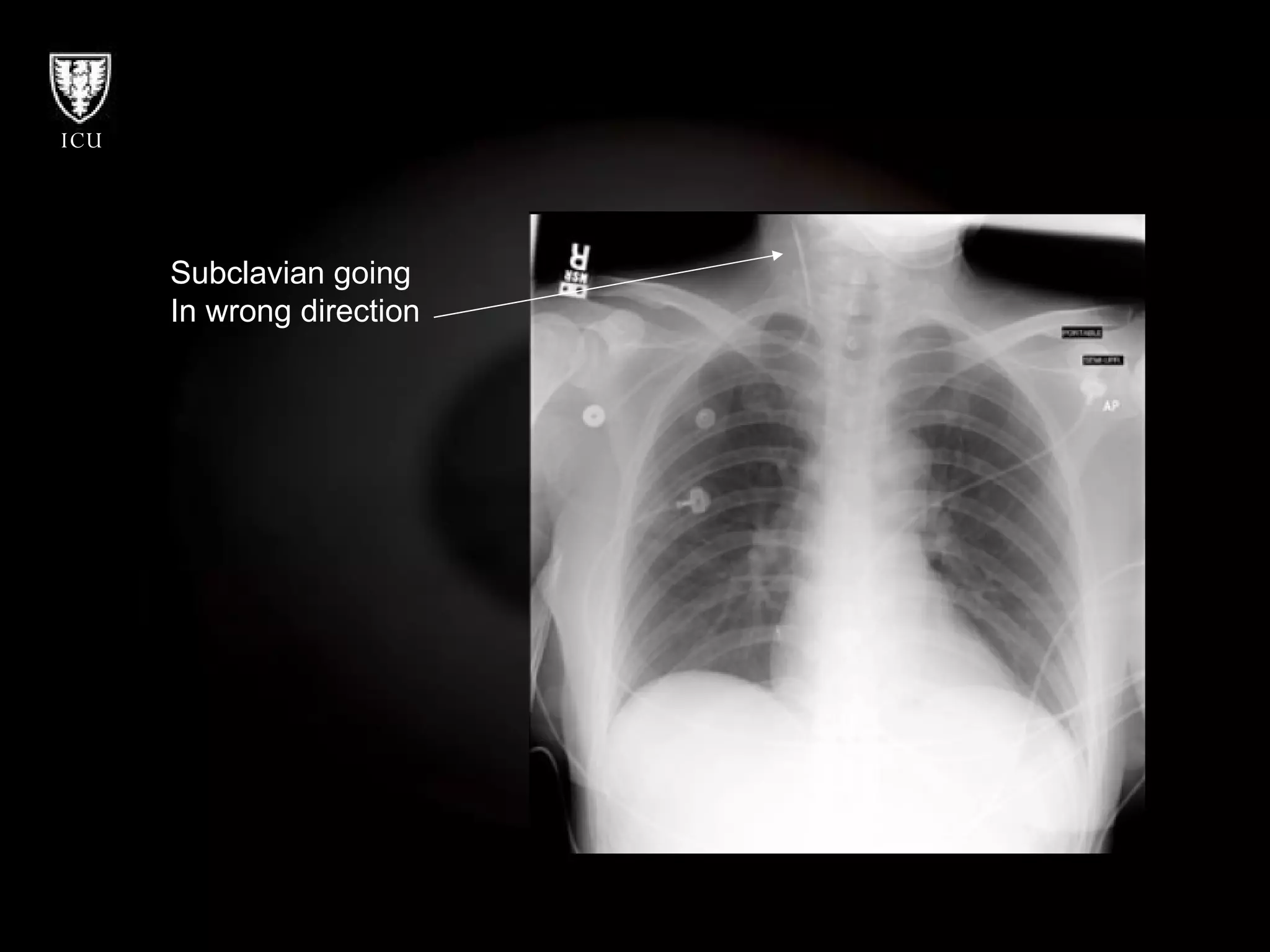
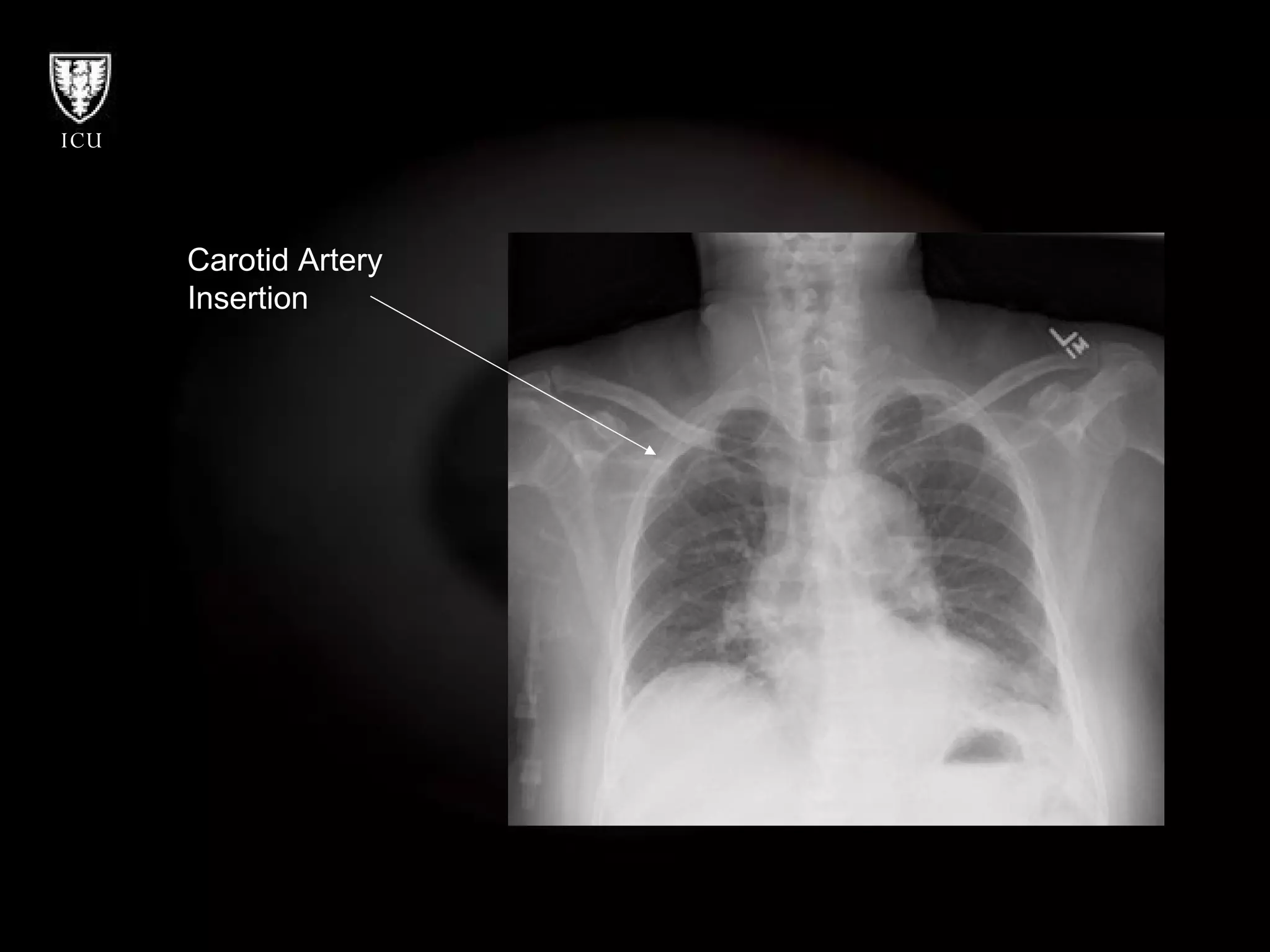
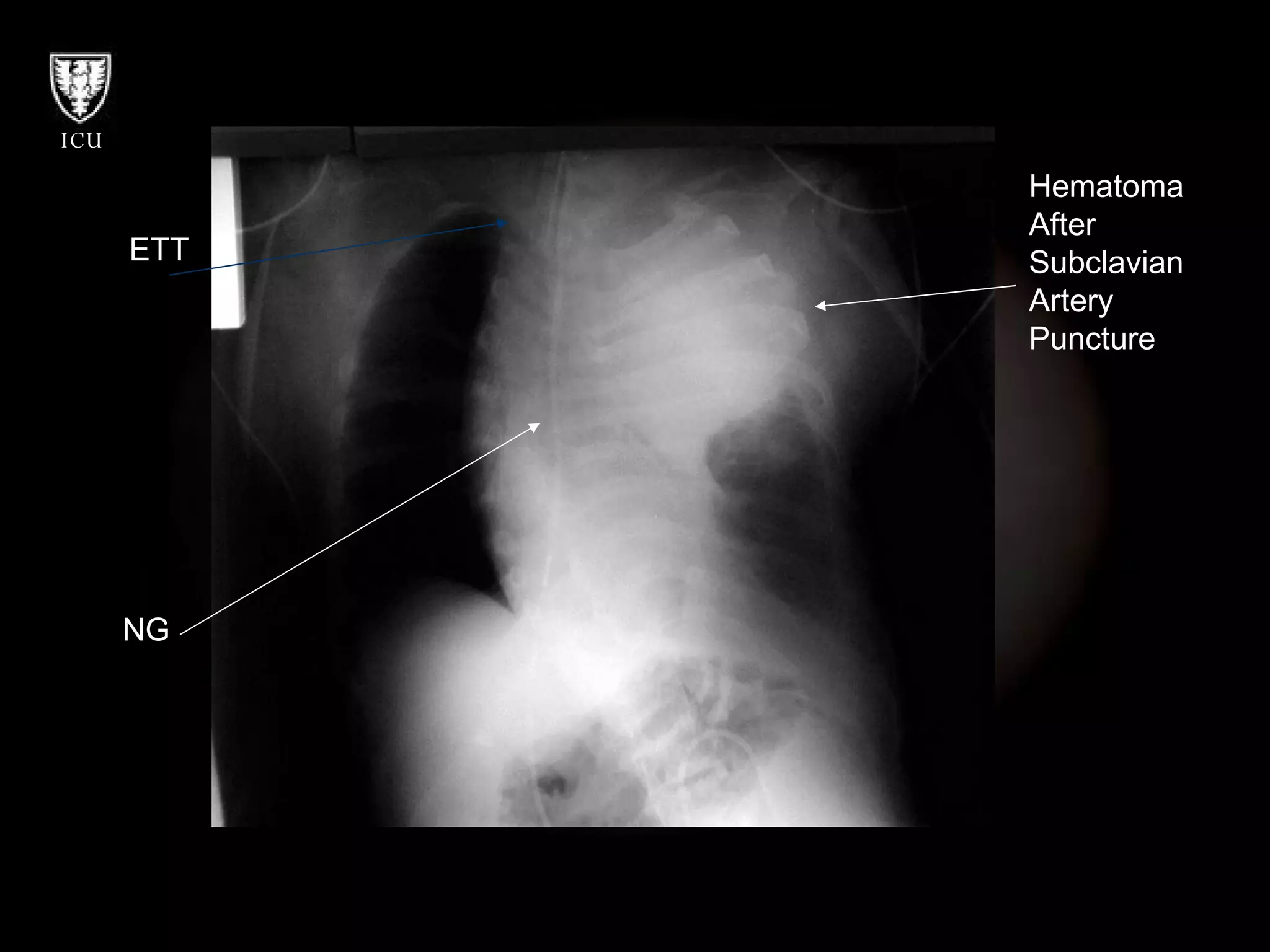
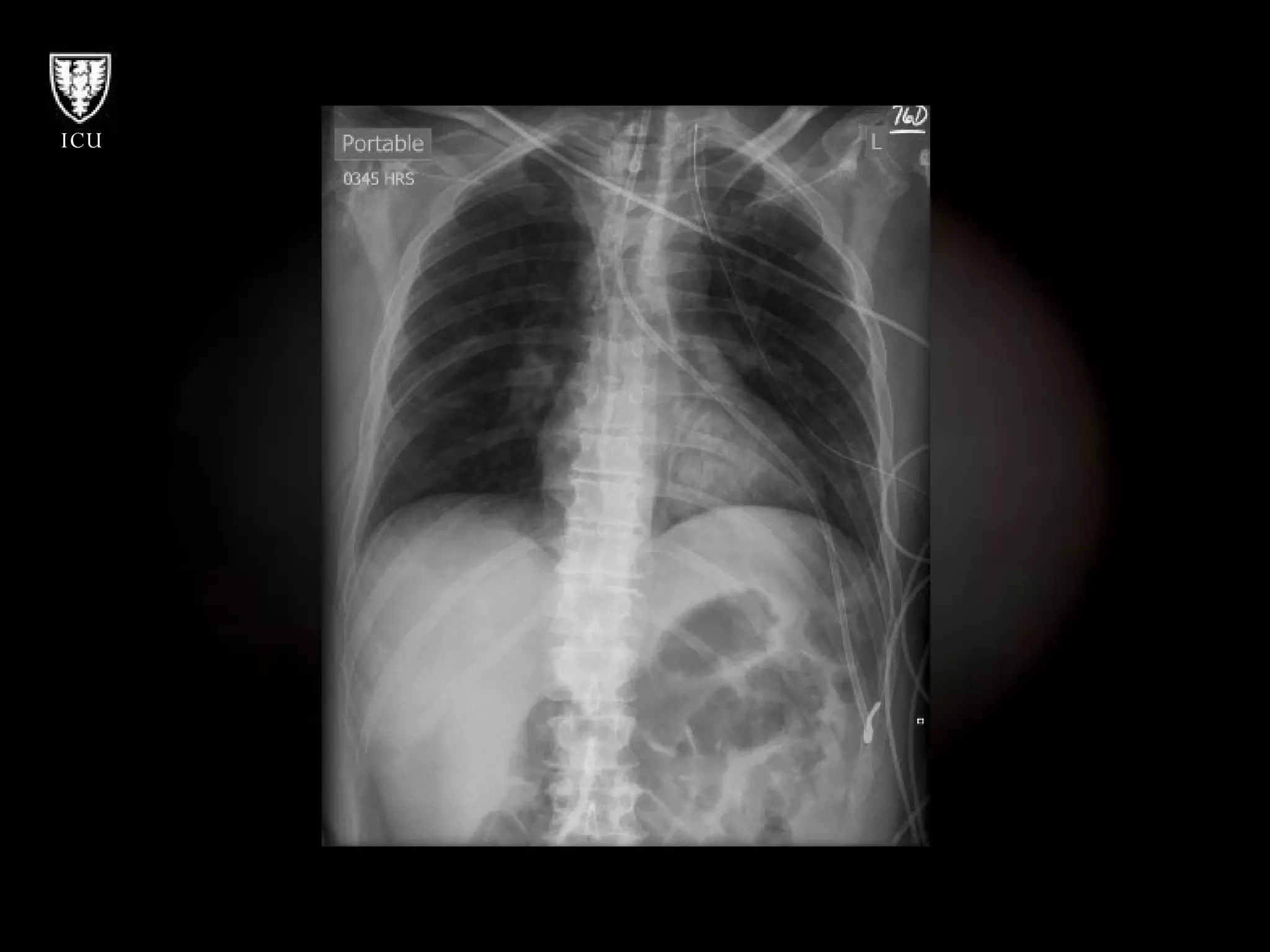
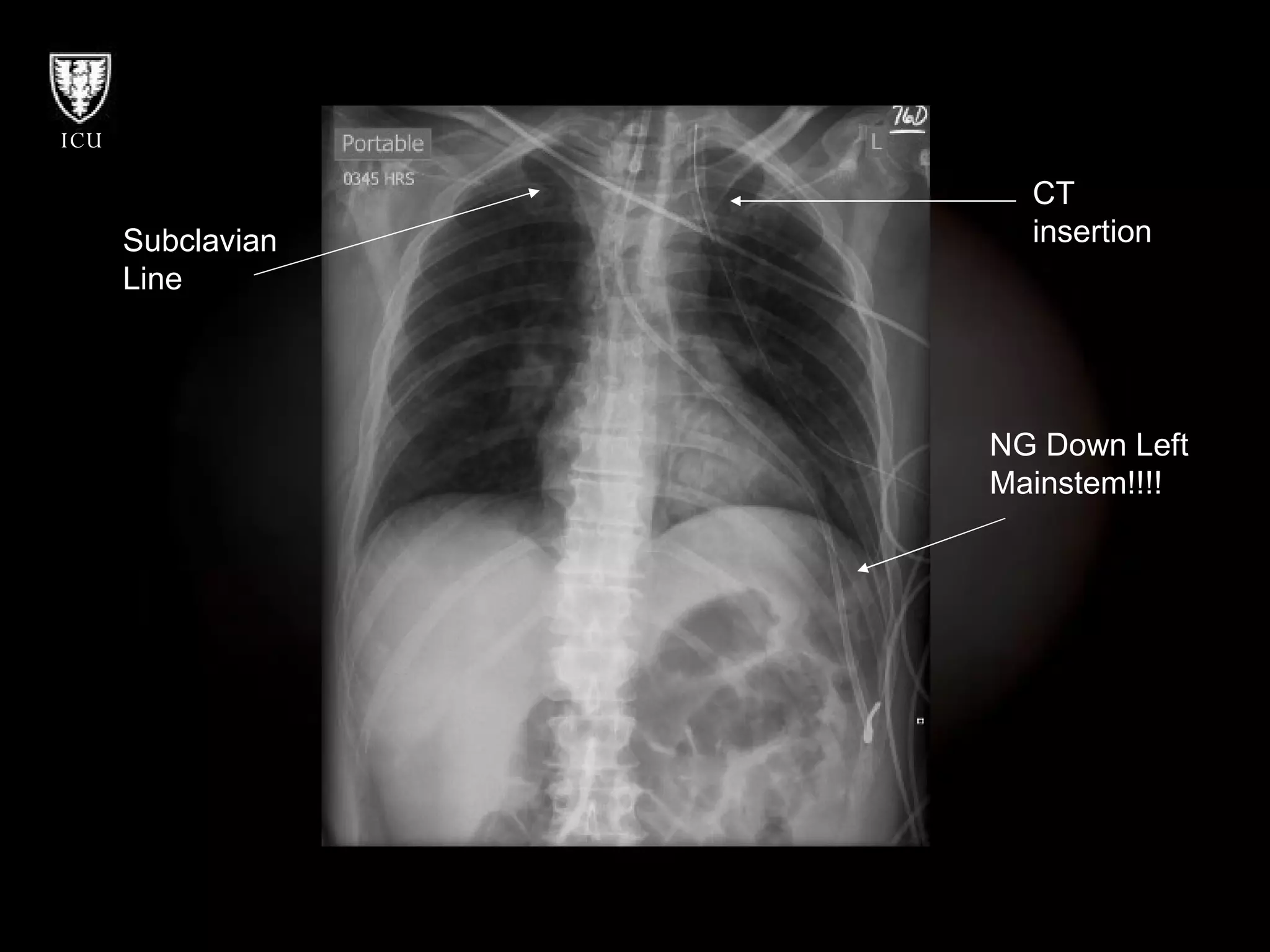
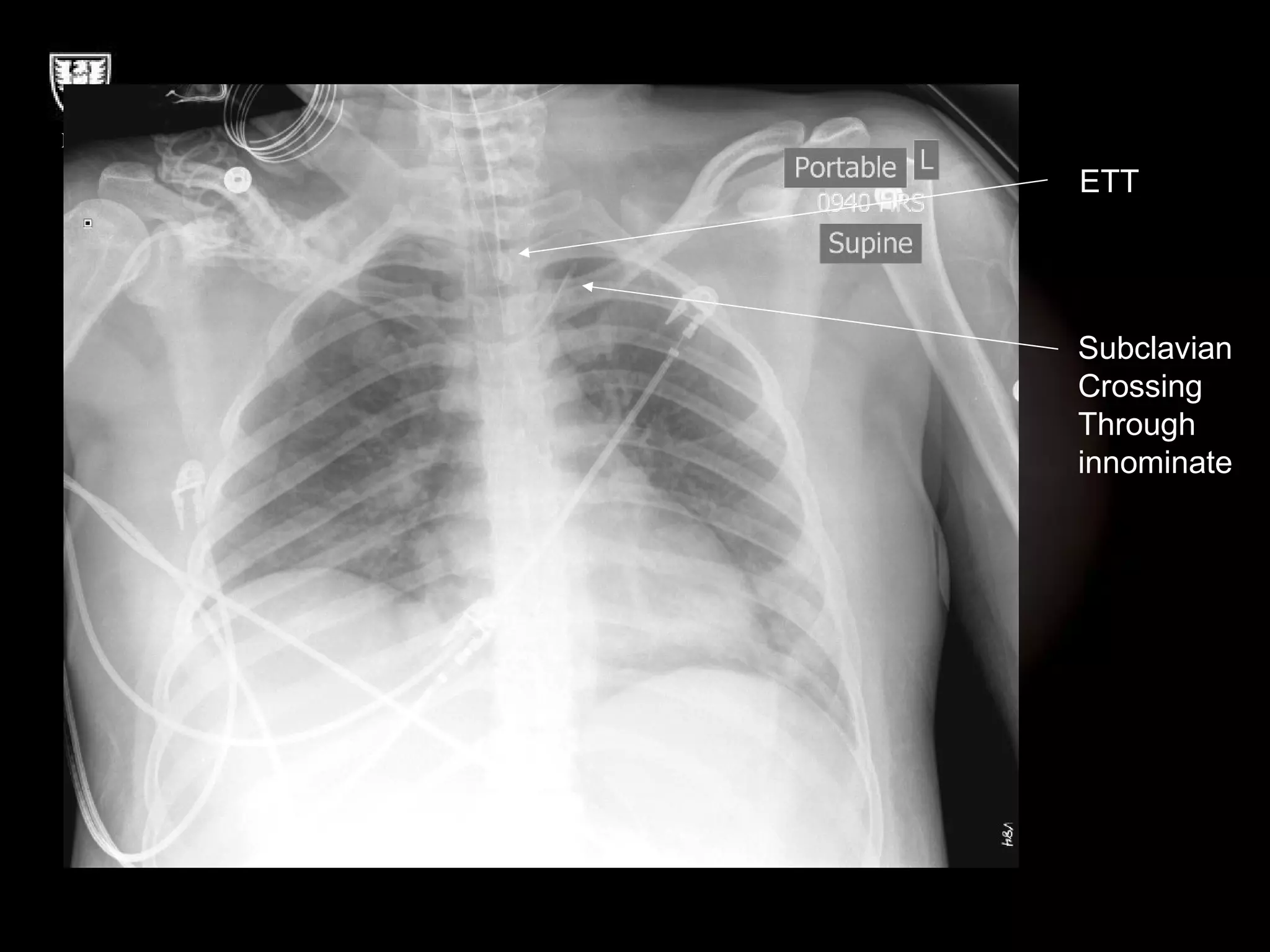
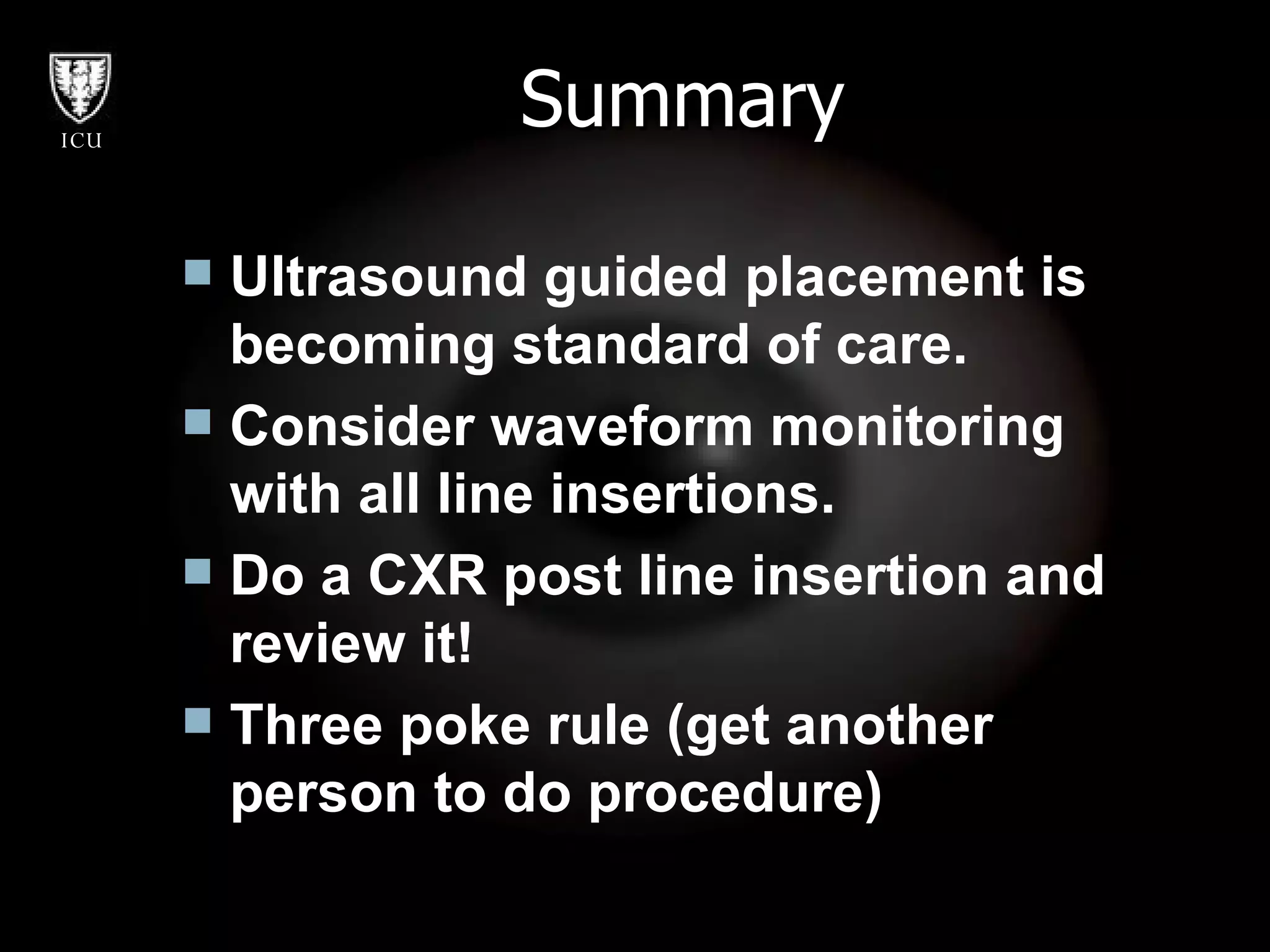
Central line insertions can have mechanical, infectious, and thrombotic complications. Mechanical complications include pneumothorax, hemothorax, arterial puncture, and organ injury. Ultrasound guidance and checking waveforms can help prevent wrong vessel cannulation. Infectious complications are common so strict sterile technique is important. Managing complications involves treating underlying issues like draining pneumothoraces or applying pressure to arterial punctures. Regularly checking placement with imaging can find problems early.