Jems201303 dl-1
- 1. MARCH 2013 ISSUE Always En Route At t
- 2. Making Precious Minutes Count™ Macro. Mini. All Set. When a patient requires intravenous therapy, EMS providers need to administer care as quickly as possible. The AMSafe-3® IV Administration Set features a 3-in-1 multi-drip chamber that allows providers to select a 10, 15 or 60 drop setting on the spot. The AMSafe-3 drop setting can be adjusted without interrupting patient care. Since the device combines three IV sets into one, it reduces inventory and takes up less room on an ambulance or in an equipment bag. 1712-30204 1712-30304 D38301 AMSafe-3 IV Set, 91”, 1 luer activated AMSafe-3 IV set, 89” with backcheck valve, AMSafe-3 IV Set, 83”, 1 luer activated injection site and 1 pre-pierced injection site, 1 pre-pierced injection site, 1 luer activated injection site and 1 pre-pierced injection site and pre-pierced injection sites, slide For more information or a product demonstration, contact your dedicated Account Manager or call 800.533.0523 Choose 11 at www.jems.com/rs 800-533-0523 www.boundtree.com
- 3. Choose 12 at www.jems.com/rs
- 4. Barbara Spoden Thanks to a dedicated EMS team and use of the ResQPOD®, Barbara survived and was able to return to playing with her granddaughter. Choose 13 at www.jems.com/rs
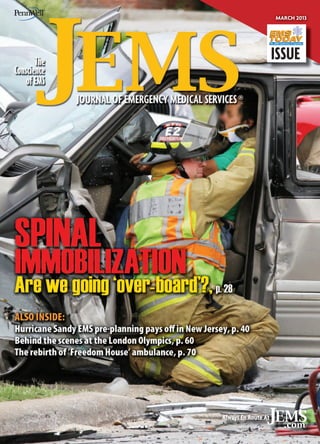
- 5. ® 28 I SPINAL IMMOBILIZATION I Time for a change By Jim Morrissey, MA, EMT-P MARCH 2013 VOL. 38 NO. 3 Contents I 40 40 50 I IN THE PATH OF DESTRUCTION I New Jersey EMS response to Superstorm Sandy aided by pre-planning & preparedness By Henry P. Cortacans, MAS, CEM, NREMT-P; & Terry Clancy, PhD, NREMT-P I THE PREHOSPITAL CARE RESEARCH FORUM PRESENTS ... I Selected abstracts for presentation at the 31st annual EMS Today Conference & Exposition in Washington, D.C., March 5–9, 2013 58 DEPARTMENTS & COLUMNS I EXPANDING THE MISSION I 60 I PLANNING LIKE AN OLYMPIAN I 5 I LOAD & GO I Now on JEMS.com 10 I EMS IN ACTION I Scene of the Month 12 I FROM THE EDITOR I ‘Special Stretchers’ By A.J. Heightman, MPA, EMT-P 14 I LETTERS I In Your Words 16 I PRIORITY TRAFFIC I News You Can Use 20 I LEADERSHIP SECTOR I Impact Ahead 22 I 24 I 80 I 82 I By Gary Ludwig, MS, EMT-P TRICKS OF THE TRADE I Batteries By Thom Dick CASE OF THE MONTH I Forward Fall By Michael Orland, MD HANDS ON I Product Reviews from Street Crews By Dominic Silvestro, EMT-P, EMS-I LIGHTER SIDE I The Slow Farewell By Steve Berry Mission: Lifeline will incorporate EMS recognition in STEMI & cardiac resuscitation systems of care By Chris Bjerke, MBA, BSN; Gary Wingrove, EMT-P; Franklin Pratt, MD; J. Lee Garvey, MD; & A. Gray Ellrodt, MD How London Ambulance Service successfully handled their ‘summer of sport’ By Jason Killens, MStJ, JP 70 I REVIVING FREEDOM HOUSE I 76 I BUILT TO SHARE I How the storied ambulance company has been reborn By Megan Corry, MA, EMT-P; Casey Keyes, BA, NREMT-B; & David Page, MS, NREMT-P The Bay Shore/Brightwaters Rescue Ambulance’s new vehicle will respond to multiple incident types and provide mutual aid By Bob Vaccaro 84 I EMPLOYMENT & CLASSIFIED ADS 87 I AD INDEX 88 I LAST WORD I The Ups & Downs of EMS I 60 Aboutvehicle involved in a multiple vehicle crash in Springfield, Mo., is being the Cover The driver of a assessed prior to extrication by a Springfield Fire Department firefighter. The issue of when to fully immobilize patients and on what devices is explored in-depth in this month’s issue of JEMS. Read more, p. 12 and pp. 28–39. IMAGE JOSEPH THOMAS PREMIER MEDIA PARTNER OF THE IAFC, THE IAFC EMS SECTION & FIRE-RESCUE MED WWW.JEMS.COM MARCH 2013 JEMS 3
- 6. The responsive emergency team delivers exceptional CPR And they choose Physio-Control to help make it happen. Today’s responsive emergency team is always looking to elevate the level of care they deliver, and they rely on evidence and data to get them there. With the CPR Solution from Physio-Control, they have the science-based, guidelines-consistent tools they need to respond better to patients—and the demands of constant performance improvement. uninterrupted hands-free compressions featuring comprehensive CPR analytics with capnography and CPR Metronome Visit our booth #811 at EMS Today 2013 in Washington D.C. to see CPR innovation in action and receive a T-shirt. physio-control.com/CPR Choose 14 at www.jems.com/rs ©2013 Physio-Control, Inc. Redmond, WA
- 7. LOAD & GO LOG IN FOR EXCLUSIVE CONTENT A BETTER WAY TO LEARN JEMSCE.COM ONLINE CONTINUING EDUCATION PROGRAM S ON LLOW U FO FEATURED BLOG: Rescuing Providence THE JOURNEY I take for granted the things I do that make up most days; starting IV’s, administering aspirin and nitro, assessing vital signs, stopping blood from leaving peoples bodies et al, but one of those mundane tasks I’ll never think of as business as usual again. Last night, while talking with a group of friends, a meeting if you will, one of the members of the group, who struggles with addiction spoke of his recent overdose, and subsequent revival and spiritual awakening. “I know how much I can do, and how much I can’t,” he explained. “Trust me, people who OD don’t do so by accident.” JEMS.com offers you JEMS com MS original content, jobs, products and resources. But we’re much more than that; we keep you in touch with your colleagues through our: > Facebook fan page; > JEMS Connect site; > Twitter account; > LinkedIn profile; > Product Connect site; and > Fire EMS Blogs site. Sponsored Product Focus MULTI-PATIENT MONITORING SYSTEM The new Multi-Patient Monitoring System (MPMS) from First Line Technology allows emergency personnel to stay connected and provide constant monitoring for up to 20 patients during triage, transport and care. The MPMS includes a roll and carry bag wired to charge both the (included) Wireless Vital Signs Monitor devices and a remote monitoring device. LIKE US facebook.com /jemsfans ▲ Check out their ad on JEMS.com! FOLLOW US twitter.com /jemsconnect DATA WEBCAST Check out our next webcast, which will be at 10 a.m. (Eastern time) March 20. In this webcast, sponsored by ZOLL Data, firefighter/paramedic and EMS 10: Innovator in EMS Awardwinner John Pringle will present, “Update on 360-degree Data: How to collect better data in the field.” He will give you practical steps to successfully integrate new electronic tools into your emergency response systems. ▲ jems.com/webcasts GET CONNECTED linkedin.com/groups? about=&gid=113182 EMS NEWS ALERTS JEMS.com Visit www.ems2020 vision.com to watch the latest 2020 Vision Leadership Series video interviews. Where do you see EMS going in 2020? That was the question put to four EMS visionaries—James J. Augustine, MD, FACEP; Matt Zavadsky, MS-HSA, EMT; David Page, MS, NREMT-P; and moderator A.J. Heightman, MPA, EMT-P. For hours, we flmed them while they created a new future. Join the 2020 EMS Visionaries LinkedIn group to get engaged in the discussion. www.FernoEMS.com Setting our sights on the future of EMS http://linkedin. ems2020vision.com jems.com/enews CHECK IT OUT jems.com/ems-products BEST BLOGGERS FireEMSBlogs.com WWW.JEMS.COM MARCH 2013 JEMS 5
- 8. ® EDITOR-IN-CHIEF I A.J. Heightman, MPA, EMT-P I aheightman@pennwell.com MANAGING EDITOR I Jennifer Berry I jenniferb@pennwell.com ASSOCIATE EDITOR I Ryan Kelley I rkelley@pennwell.com ASSISTANT EDITOR I Kindra Sclar I kindras@pennwell.com ONLINE NEWS/BLOG MANAGER I Bill Carey I billc@pennwell.com ASSOCIATE WEB EDITOR I Nicole Reino I nicoler@pennwell.com EDITORIAL DIRECTOR I Shannon Pieper I shannonp@pennwell.com MEDICAL EDITOR I Edward T. Dickinson, MD, NREMT-P, FACEP CONTRIBUTING EDITOR I Bryan Bledsoe, DO, FACEP, FAAEM ART DIRECTOR I Liliana Estep I alildesign@me.com CONTRIBUTING ILLUSTRATORS Steve Berry, NREMT-P; Paul Combs, NREMT-B CONTRIBUTING PHOTOGRAPHERS Vu Banh, Glen Ellman, Craig Jackson, Kevin Link, Courtney McCain, Tom Page, Rick Roach, Steve Silverman, Michael Strauss, Chris Swabb DIRECTOR OF ePRODUCTS/PRODUCTION I Tim Francis I timf@pennwell.com PRODUCTION COORDINATOR I Matt Leatherman I matthewl@pennwell.com PUBLICATION OFFICE 800/266-5367 I Fax 858/638-2601 ADVERTISING DEPARTMENT 800/266-5367 I Fax 858/638-2601 ADVERTISING DIRECTOR I Judi Leidiger I 619/795-9040 I j.leidiger@jems.com WESTERN ACCOUNT REPRESENTATIVE I Cindi Richardson I 661/297-4027 I c.richardson@jems.com SENIOR SALES COORDINATOR I Elizabeth Zook I 951/244-1245 I elizabethz@pennwell.com REPRINTS, ePRINTS & LICENSING I Rae Lynn Cooper I 918/831-9143 I raec@pennwell.com VICE PRESIDENT, MARKETING SERVICES I Paul Andrews I 240/595-2352 I marketingservices@pennwell.com SUBSCRIPTION DEPARTMENT I 888/456-5367 DIRECTOR, AUDIENCE DEVELOPMENT & SALES SUPPORT I Mike Shear I mshear@pennwell.com MARKETING & CONFERENCE DIRECTOR I Debbie Murray I debbiem@pennwell.com MARKETING & CONFERENCE COORDINATOR I Vanessa Horne I vhorne@pennwell.com • CHAIRMAN I Frank T. Lauinger PRESIDENT & CHIEF EXECUTIVE OFFICER I Robert F. Biolchini CHIEF FINANCIAL OFFICER I Mark C. Wilmoth SENIOR VICE PRESIDENT & GROUP PUBLISHER I Lyle Hoyt I lyleh@pennwell.com VICE PRESIDENT/PUBLISHER I Jeff Berend I jeffb@pennwell.com • • www.EMSToday.com EXECUTIVE DIRECTOR I Jeff Berend CONFERENCE DIRECTOR I Debbie Murray EDUCATION DIRECTOR I A.J. Heightman EVENT OPERATIONS MANAGER I Amanda Wilson EXHIBIT SERVICES MANAGER I Raymond Ackermann EXHIBIT SALES REPRESENTATIVE I Sue Ellen Rhine I 918/831-9786 I sueellenr@pennwell.com EXHIBIT SALES REPRESENTATIVE I Tracy Thompson I 918/832-9390 I tracyt@pennwell.com • • FOUNDING EDITOR I Keith Griffiths FOUNDING PUBLISHER James O. Page (1936–2004) ® bringing change to life ® Choose 15 at www.jems.com/rs
- 9. Accurate from the First Breath World’s smallest portable self-contained capnometer EMMA™ (Emergency Mainstream Analyzer) is a fully selfcontained mainstream capnometer that requires no routine calibration and virtually no warm up time.1 With rapid measurement of end-tidal CO2 and respiration rate, EMMA can help providers guide ventilation rates and assess the effectiveness of CPR allowing them to make adjustments in the course of treatment, breath by breath. 800-257-3810 | www.masimo.com © 2013 Masimo Corporation. All rights reserved. 1 EMMA Users Manual. Choose 16 at w ww.jems.com/rs
- 10. ® EDITORIAL BOARD WILLIAM K. ATKINSON II, PHD, MPH, MPA, EMT-P President & Chief Executive Officer, WakeMed Health & Hospitals JAMES J. AUGUSTINE, MD, FACEP Medical Director, Washington Township (Ohio) Fire Department Associate Medical Director, North Naples (Fla.) Fire Department Director of Clinical Operations, EMP Management Clinical Associate Professor, Department of Emergency Medicine, Wright State University STEVE BERRY, NREMT-P Paramedic & EMS Cartoonist, Woodland Park, Colo. BRYAN E. BLEDSOE, DO, FACEP, FAAEM Professor of Emergency Medicine, Director, EMS Fellowship, University of Nevada School of Medicine Medical Director, MedicWest Ambulance CRISS BRAINARD, EMT-P Deputy Chief of Operations, San Diego Fire-Rescue CHAD BROCATO, DHS, REMT-P Assistant Chief of Operations, Deerfield Beach (Fla.) Fire-Rescue Adjunct Professor of Anatomy & Physiology, Kaplan University J. ROBERT (ROB) BROWN JR., EFO Fire Chief, Stafford County (Va.) Fire & Rescue Department Executive Board, EMS Section, International Association of Fire Chiefs CAROL A. CUNNINGHAM, MD, FACEP, FAAEM State Medical Director, Ohio Department of Public Safety, Division of EMS THOM DICK, EMT-P Quality Care Coordinator, Platte Valley (Colo.) Ambulance BRUCE EVANS, MPA, EMT-P Deputy Chief, Upper Pine River Bayfield Fire Protection, Colorado District JAY FITCH, PHD President & Founding Partner, Fitch & Associates RAY FOWLER, MD, FACEP Associate Professor, University of Texas Southwestern School of Medicine Chief of EMS, University of Texas Southwestern Medical Center Chief of Medical Operations, Dallas Metropolitan Area BioTel (EMS) System ADAM D. FOX, DPM, DO Assistant Professor of Surgery, Division of Trauma Surgery & Critical Care, University of Medicine & Dentistry of New Jersey Former Advanced EMT-3 (AEMT-3) GREGORY R. FRAILEY, DO, FACOEP, EMT-P Medical Director, Prehospital Services, Susquehanna Health Tactical Physician, Williamsport (Pa.) Bureau of Police Special Response Team 8 JEMS MARCH 2013 JEFFREY M. GOODLOE, MD, FACEP, NREMT-P Professor & EMS Section Chief Emergency Medicine, University of Oklahoma School of Community Medicine Medical Director, EMS System for Metropolitan Oklahoma City & Tulsa KEITH GRIFFITHS President, RedFlash Group Founding Editor, JEMS DAVE KESEG, MD, FACEP Medical Director, Columbus Fire Department Clinical Instructor, Ohio State University W. ANN MAGGIORE, JD, NREMT-P Associate Attorney, Butt, Thornton & Baehr PC Clinical Instructor, University of New Mexico, School of Medicine CONNIE J. MATTERA, MS, RN, EMT-P EMS Administrative Director & EMS System Coordinator, Northwest (Ill.) Community Hospital MIKE MCEVOY, PHD, REMT-P, RN, CCRN EMS Coordinator, Saratoga County, N.Y. EMS Editor, Fire Engineering Magazine Resuscitation Committee Chair, Albany (N.Y.) Medical College MARK MEREDITH, MD Assistant Professor, Emergency Medicine and Pediatrics, Vanderbilt Medical Center Assistant EMS Medical Director for Pediatric Care, Nashville Fire Department GEOFFREY T. MILLER, EMT-P Director of Simulation Eastern Virginia Medical School, Office of Professional Development BRENT MYERS, MD, MPH, FACEP Medical Director, Wake County EMS System Emergency Physician, Wake Emergency Physicians PA Medical Director, WakeMed Health & Hospitals Emergency Services Institute MARY M. NEWMAN President, Sudden Cardiac Arrest Foundation JOSEPH P. ORNATO, MD, FACP, FACC, FACEP Professor & Chairman, Department of Emergency Medicine, Virginia Commonwealth University Medical Center Operational Medical Director, Richmond Ambulance Authority JERRY OVERTON, MPA Chair, International Academies of Emergency Dispatch DAVID PAGE, MS, NREMT-P Paramedic Instructor, Inver Hills (Minn.) Community College Paramedic, Allina Medical Transportation Member of the Board of Advisors, Prehospital Care Research Forum PAUL E. PEPE, MD, MPH, MACP, FACEP, FCCM Professor, Surgery, University of Texas Southwestern Medical Center Head, Emergency Services, Parkland Health & Hospital System Head, EMS Medical Direction Team, Dallas Area Biotel (EMS) System DAVID E. PERSSE, MD, FACEP Physician Director, City of Houston Emergency Medical Services Public Health Authority, City of Houston Department. of Health & Human Services Associate Professor, Emergency Medicine, University of Texas Health Science Center—Houston EDWARD M. RACHT, MD Chief Medical Officer, American Medical Response JEFFREY P. SALOMONE, MD, FACS, NREMT-P Trauma Medical Director, Maricopa Medical Center Professor of Surgery, University of Arizona College of Medicine—Phoenix KATHLEEN S. SCHRANK, MD Professor of Medicine & Chief, Division of Emergency Medicine, University of Miami School of Medicine Medical Director, City of Miami Fire Rescue Medical Director, Village of Key Biscayne Fire Rescue JOHN SINCLAIR, EMT-P International Director, IAFC EMS Section Fire Chief & Emergency Manager, Kittitas Valley (Wash.) Fire & Rescue COREY M. SLOVIS, MD, FACP, FACEP, FAAEM Professor & Chair, Emergency Medicine, Vanderbilt University Medical Center Professor, Medicine, Vanderbilt University Medical Center Medical Director, Metro Nashville Fire Department Medical Director, Nashville International Airport WALT A. STOY, PHD, EMT-P, CCEMTP Professor & Director, Emergency Medicine, University of Pittsburgh Director, Office of Education, Center for Emergency Medicine RICHARD VANCE, EMT-P Captain, Carlsbad (Calif.) Fire Department JONATHAN D. WASHKO, BS-EMSA, NREMT-P, AEMD Assistant Vice President, North Shore-LIJ Center for EMS Co-Chairman, Professional Standards Committee, American Ambulance Association Ad-Hoc Finance Committee Member, NEMSAC KEITH WESLEY, MD, FACEP Medical Director, HealthEast Medical Transportation KATHERINE H. WEST, BSN, MED, CIC Infection Control Consultant, Infection Control/Emerging Concepts Inc. STEPHEN R. WIRTH, ESQ. Attorney, Page, Wolfberg & Wirth LLC. Legal Commissioner & Chair, Panel of Commissioners, Commission on Accreditation of Ambulance Services (CAAS) DOUGLAS M. WOLFBERG, ESQ. Attorney, Page, Wolfberg & Wirth LLC WAYNE M. ZYGOWICZ, BA, EFO, EMT-P EMS Division Chief, Littleton (Colo.) Fire Rescue
- 11. When urgency and bravery are essential job requirements, the success of your business depends on a commercial vehicle that won’t back down from a challenge. With an Adaptive Electronic Stability Program® 1 and both Best-In-Class* payload capacity and standing height, only the 2013 Freightliner Sprinter is designed to answer the call as boldly as you do every day. freightlinersprinterusa.com DRIVEN LIKE YOU. ©2013 Daimler Vans USA, LLC *Based on a comparison of the Automotive News classification of full-size commercial vans. 1 No system, regardless of how advanced, can overcome the laws of physics or correct careless driving. Please always wear your seat belt. Performance is limited by available traction, which snow, ice and other conditions can afect. Always drive carefully, consistent with conditions. Best performance in snow is obtained with winter tires. Choose 18 at www.jems.com/rs Choose 17 at www.jems.com/rs
- 12. EMS IN ACTION SCENE OF THE MONTH 10 JEMS MARCH 2013 >> PHOTOS JOSEPH THOMAS
- 13. PEDIATRIC IMMOBILIZATION S t. John’s/Mercy (Mo.) EMS Paramedic Christy Biram carries a 3-year-old female pediatric patient on a pediatric backboard to a waiting ambulance at the scene of a crash that involved two vehicles colliding at a stoplight. The vehicle the pediatric patient was in was hit when another vehicle allegedly ran a red light. The girl was secured properly in a child safety seat and had been extricated from the vehicle and car seat by her mother prior to EMS arrival. Her only injuries were abrasions to her thighs and clavicles from the safety seat restraints. She had been placed in spinal mobile restriction by Springfield Fire Department prior to EMS arrival. She was transported to a Level 1 trauma center, where she was treated and released. The driver of the other car collided with one of the stoplight posts, causing the battery to fly out of the vehicle and hit a pedestrian who narrowly missed getting hit by the vehicle. The pedestrian had a minor leg injury but refused care on scene, and the driver of the vehicle that ran the light had to be extricated and was transported to an emergency department. Note the crew’s professionalism, covering the patient’s body surface with a turnout coat after exposing and assessing her lower torso. WWW.JEMS.COM MARCH 2013 JEMS 11
- 14. FROM THE EDITOR PUTTING ISSUES INTO PERSPECTIVE >> BY A.J. HEIGHTMAN, MPA, EMT-P ‘SPECIAL STRETCHERS’ How two eliminated words impacted immobilization options I t’s amazing how committees, lim- FERNO FULL-BODY VACUUM MATTRESS splinting; and pad the splint carefully to ited research and the omission of prevent pressure points and discomfort to a few words can change protocols the extremity [and the patient].” and affect the delivery of patient care Morrissey’s article gives you the and comfort. Jim Morrissey’s article, science, research and reasons to “Spinal Immobilization,” pp. 28–39, allow your crews to use multiple is an epic piece of work, backed by FERNO’S EASYFIX VACUUM MATTRESS/STRETCHER proven “special stretchers,” in addi36 footnoted references that illustrate COMBINATION tion to the traditional longboard, we over-board patients, waste preto immobilize patients and “splint” cious time at penetrating injury calls their injuries. and make patients uncomfortable by I spent a day with Poway (Calif.) placing them on hard surfaces that do Fire Department Captain Andy Page not fit their anatomy or support their and crews from Engine 3711 and injuries without proper padding and Medic 3791. We applied, secured, weight distribution. moved and transported paramedic/ I’m going to take you back to 1971, firefighter Jon Maxwell up and down when EMS got its “roots” in formalstairways in some of the latest “speized education with the release of the cial stretchers” designed to properly initial EMT textbook, Emergency Care immobilize his spine. and Transportation of FERNO’S MODEL 137 FLEXIBLE STRETCHER WITH BUILT-IN We used: ConvenHARTWELL MEDICAL EVAC-U-SPLINT MATTRESS/STRETCHER USED ALONG the Sick and Injured. RESTRAINTS USED IN TANDEM WITH A VACUUM SPLINT tional scoop-style WITH A HARTWELL COMBICARRIER The first AAOS textstretchers; Full-body book stated: vacuum platforms; “Carefully splint the Vacuum splints and injured spine, avoiding a Ferno Flexible abnormal or excessive Stretcher. We also used motion. Be sure that the Ferno’s EasyFix Vacinjured person is properly uum Mattress/Stretcher splinted and transported that is being used on a long backboard or throughout Europe special stretcher withand was recently introout bending or twisting duced in the U.S. the spine in any direction.” Most of the devices I call your attention to the important words “or special offered more comfort and security than a longboard without extra stretcher” because those words were somehow omitted from padding. The vacuum devices were also durable, easily moldable to subsequent editions of the AAOS and most other textbooks. the patient, and tended to better “cradle” the patient securely. We Those omitted words resulted in decreased use of scoop and used SSCOR and Laerdal suction devices to speed up the process. canvas stretchers with slat supports, and SKED stretchers, in Perhaps the most interesting finding was that vacuum matsome systems, and should be added back into our protocols and tresses used in conjunction with the Ferno flexible stretcher and its textbooks to allow crews to use multiple devices to accomplish six conveniently-located handles, offered the best body mechanics spinal immobilization. and positioning to maneuver our patient down stairways and The “General Principles of Splinting” section in the 1971 around tight corners, proving that some things haven’t changed AAOS textbook presented treatment considerations that still since 1971, when this type of flexible stretcher was first introduced hold true today: to EMS. “All fractures should be ‘splinted where they lie’; Apply the splint or banSee a demo of the EasyFix Mattress at www.youtube.com/watch?v=-WF73wKdfZM dage before moving or transporting the patient; With some very important exceptions, a severely angulated fracture should be straightened prior to 12 JEMS MARCH 2013
- 15. The Safe Choice Introcan Safety® 3 Closed IV Catheter helps shield against Needlesticks Blood Exposure Catheter Complications From start to finish, Introcan Safety 3 provides: Fully automatic safety shield that protects against needlesticks. Multiple-access septum that helps prevent blood exposure. Advanced stabilization that minimizes catheter movement to help reduce irritation and associated restarts. Lower cost and less waste from insertion through disposal. introcansafety.bbraunusa.com 1-800-227-2862 The following is a list of supporting documents and reference material: 1) Tosini, et al “Needlestick Injury Rates According to Diferent Types of Safety-Engineered Devices: Results of a French Multicenter Study”, Infection Control and Hospital Epidemiology, Vol. 31, No. 4 April 2012 pp. 402-407 2) Bausone-Gazda D, et al, A Randomized Controlled Trial to Compare the Complications of 2 Peripheral Intravenous Catheter-Stabilization Systems, Journal of Infusion Nursing, 2012, Nov-Dec: 33(6):371 84 3) Shears G MD, Comparing an Intravenous Stabilizing Device to Tape, Journal of Infusion Nursing, Vol. 29, No. 4 July/August 2006 4) B. Braun Engineering Data on File 5) B. Braun Introcan Safety 3 Cost Analysis Model 6) McNeill, EE, et al, A Clinical Trial of a New All-in-one Peripheral Short Catheter, JAVA, 2009, Vol. 14, No. 1, pp. 46-50 13-3611_2/13_JEMS_BB 7) Infusion Nurses Society (2011), Infusion Nursing Standards of Practice, Journal of Infusion Nursing Supplement, Vol. 34, No. 15, Std. 22, Std. 36 Choose 18 at www.jems.com/rs
- 16. LETTERS IN YOUR WORDS ADDING TO THE A D DISCUSSION PHOTO COURTESY PHYSIO-CONTROL This month, we feature some T strong opinions from readers on s two recent articles. The first is a t response to a JEMS.com Street r Science column “Are the BenS efits of Mechanical CPR Worth e the Interruption Time?” by Keith t Wesley, MD, FACEP, and MarW shall J. Washick, BAS, NREMT-P, s that reviewed a study examining t interruption time in mechanii cal CPR. The second comment is c from one of our Facebook fans, f who takes issue with Thom Dick’s w August “Tricks of the Trade” colA umn advising on “Psych Transu fers: Know how to deal with these f types of patients.” t MECHANICAL CPR ADVANTAGES We read the article “Are the Benefits of Mechanical CPR Worth the Interruption Time?” (www.jems.com/article/patient-care/are-benefits-mechanical-cpr-worthinterr) with great interest. We participated in the NALE project and submitted our data as part of the article published in Resuscitation. The authors of the review bring up some important points about the findings, but we fear they do not answer the question posed in the title of their article. We have extensive experience using the mechanical compression device with more than 1,200 uses to date. One of the first things we learned when deploying the device was that crews put it as a priority and the other, time-important interventions were delayed. We had to put it into our protocols and train our people to place it later in the event, after other interventions were completed. Next, we learned that placing the device tended to cause everyone else to pause and help out. This is much like our previous experience with intubation where everyone stopped what they were doing until the “vital” procedure was completed. We changed our protocol again and trained our staff how to place the device with no or minimal interruptions in other tasks. We now have a procedure where the device is placed in stages and the maximum interruption in compressions is 15 seconds. The benefits of the device are many. We can see in our cases that interruptions are minimal and short once the device is placed. That may be the best argument when discussing whether the interruption is worth it. We see it as accepting an early 15 second delay which then prevents multiple delays later in the event. 14 JEMS MARCH 2013 During our quality assurance reviews, we see interruptions as providers tire and switch users, or as the patient’s location is changed. There is a real challenge in any research pertaining to cardiac arrest right now. That challenge is trying to associate one treatment with a definitive improvement in outcome. This is a rapidly changing body of knowledge and there is no agreed-upon protocol. So the question of whether the delay in compressions when placing the device is worth it is a difficult question to answer and maybe should not be asked. A better question might be “What are the advantages of using a mechanical compression device, and how does it fit into a system approach to care of the cardiac arrest victim?” Our extensive experience is a resounding “yes,” it is a vital part of our overall approach to improving the community’s and emergency care system’s response to cardiac arrest. Charles Lick, MD Paul Satterlee, MD Allina Health EMS PSYCH ISSUES I am sorry Thom … while I’m sure you are a great medic and all, I just feel much of this is bad advice. The main reason being, why would/ should EMS be transporting patients that are currently off their meds and/or known to be diagnosed at the hospital as psychotic, are potentially suicidal and/or homicidal, when we have very little to no education in handling this? Isn’t it enough that we have to occasionally deal with potentially psychotic, suicidal or homicidal patients? I read a story from a provider just last night who described a situation where a psych patient, who went nuts during an inter-facility transport, was able to free themselves, threaten the provider and then proceed to jump out of the ambulance and run away. The truth is, as long as these patients don’t require some sort of medical intervention en route to the receiving medical/psychological treatment facility, there is absolutely no reason whatsoever that they should not be transported by law enforcement. Law enforcement officers have the training and authority to safely handle these patients, not EMS providers. Jason M. Via Facebook Author Thom Dick, EMT-P, responds: Thanks, Jason, for highlighting these issues. I think no matter who we are or how great our skill, we don’t “know” very much about most of the sick people we meet—certainly not during the brief span of an ED visit. But even if we could be sure somebody’s etiology is psychological, does that somehow transform them into something less than a sick person? I don’t think it does. I agree with you that we all need and deserve to understand more about behavioral disorders. The Western medicine to which we all subscribe endorses a pathetic approach to people with mental illness. Your health insurance company will typically pay for a 60-minute first visit with an internist. Care to guess what they’ll allow for a first visit with a psychiatrist, for a much more complex problem? On average, they’ll pay a psychiatrist for 15 minutes. What we call caring for mental patients basically amounts to throwing drugs at them. It’s no wonder. The standard Diagnostic and Statistical Manual (DSM) you’ll find on the desk of every ED physician is republished every few years as a means of classifying people with psychiatric illnesses. The current edition, the DSM-IV, lists six technical editors—all with published direct financial ties to pharmaceutical companies. Five of those six are linked to the same pharmaceutical company (Eli Lilly). As for bad advice, every one of the suggestions in this article would have helped the crew you describe to sense, predict and prevent the incident they experienced, as well as protect the patient and the public who were also endangered. It’s sad that, after all these years, the EMS texts we trust either ignore this important part of field medicine or recommend procedures that are sure to get us injured along with the sick people we care for. In my opinion, this is medicine we’re doing here. Medicine is supposed to help people. We’re supposed to help people. And a cage car is just not part of that process.
- 17. Your patient requires urgent pain medication. How can you administer this less invasively? ® Answer. LMA MAD Nasal ™ No shot. No needle. No risk of needle stick injury. The LMA MAD Nasal™ atomization device is the safe and painless way to deliver medication into your patient’s blood * stream without an intravenous line. ATOMIZATION SPRAY SOFT CONICAL PLUG The spray atomizes drugs into a fine mist of particles 30 - 100 microns in size. The plug forms a seal with the nostril preventing expulsion of fluid. FLEXIBLE STYLET The flexible stylet allows 180° positioning of the nasal plug. *For use with drugs approved for intranasal delivery For more information contact your LMA representative or visit LMANA.com. LMA FAMILY LMA Atomization® | LMA EMS™ | LMA Airway Management™ | LMA Visualization™ | LMA Pain Management™ 4660 La Jolla Village Drive, Suite 900 | San Diego, CA 92122 | 800-788-7999 | Fax 858-622-4130 | www.LMANA.com Teleflex, LMA, LMA Airway Management, LMA Atomization, LMA Better by Design, LMA EMS, LMA MAD Nasal, LMA Pain Management, LMA Visualization and MAD are trademarks or registered trademarks of Teleflex Incorporated or its affiliates. ©2013 Teleflex Incorporated. All rights reserved. 2013-1644. Choose 19 at www.jems.com/rs
- 18. PRIORITYUSE TRAFFIC NEWS YOU CAN NFFF Response to Violent Incidents Nine questions first responders should ask T IMAGE COURTESY NATIONAL FALLEN FIRE FIGHTERS he Newtown (Conn.) school shooting and Webster (N.Y.) ambush of firefighters provide increased awareness of violence against emergency responders. East Hartford (Conn.) Fire Chief John Oates, writing for the National Fallen Fire Fighters (NFFF), has provided nine questions responders should ask: 1. Do you use risk/benefit analysis for every call? 2. Do you have an effective relationship at all levels with the law enforcement agencies in your community? 3. How good is the information you get from your dispatcher? 4. Do you allow members to “first respond” directly to the scene? 5. Does your law enforcement agency use an incident management system? 6. When responding to a potentially violent incident, do you Cover of the NFFF report “Firefighter Life Safety Initiative 12.” seek out a law enforcement PREVENTING LINE-OF-DUTY INJURY officer when you arrive? 7. Have you told your fire officers/per- Everyone Goes Home is a national prosonnel that it’s OK to leave the scene gram by the National Fallen Firefighters Foundation to prevent line-of-duty deaths if things start to turn bad? 8. Is there a point at which you don’t and injuries. In March 2004, a Firefighter respond or limit your response to vio- Life Safety Summit was held in Tampa, Fla., to address the cultural, philosophilent incidents? 9. Is your uniform easily mistaken for cal, technical and procedural problems that affected safety within the fire service. law enforcement? These questions came from a March 2012 The most important domains were identifocus group of 35 participants representing fied, resulting in 16 Firefighter Life Safety 29 organizations. The NFFF-commissioned Initiatives. Everyone Goes Home started report from this group, “Firefighter Life as a way of implementing initiatives at the Safety Initiative 12 Final Report: National local level. NFFF asked subject matter experts to protocols for response to violent incidents should be developed and championed,” is develop a white paper for each initiapart of a resource package covering 16 Fire- tive. Chief Oates provided the Initiative fighter Life Safety Initiatives of the Everyone 12 report. The Novato, Calif., 2007 summit developed actionable objectives to Goes Home program. support each of the Firefighter Life Safety Initiatives. Noting that there was, “an absence of response protocols for violent incidents in many fire departments” a focus group met in Anne Arundel County, Md., in 2012 to develop an expanded report for Initiative 12, including the nine questions. There’s no enforcement authority or funding to implement the Firefighter Life Safety Initiatives. Some feel that more effort should be directed against those who assault responders. ‘PARAMEDICS ARE NOT PUNCHING BAGS’ New South Wales, Australia, ambulance service acting Commissioner Mike Willis announced a zero-tolerance policy toward violence against EMS personnel, noting on the agency’s website that there were six assaults against paramedics in early December. There’s a perception that sanctions against those who assault EMS personnel are inadequate. In Illinois it’s a felony to assault a first responder; however, Chicago paramedics claimed, in a WLS-TV ABC News 7 report, that those who assault them get trivial punishment. One technique that has been used is to fill a courtroom with emergency responders in uniform. In January, the New York Post reported that two dozen EMS workers filled a Manhattan courtroom to support their colleague who was allegedly choked by a drunken assistant district attorney. — Michael J. Ward, MGA Reports referenced in this article are available at: www.everyonegoeshome. com/news/2013/initiative12_012913.html For more of the latest EMS news, go to jems.com/news 16 JEMS MARCH 2013
- 19. The JEMS Family of Products: Helping You Save Lives JEMS, Journal of Emergency Medical Services With content from writers who are EMS professionals in the feld, JEMS provides the information you need on clinical issues, new products and EMS trends. Available in print and digital editions! JEMS.com eNewsletter JEMS.com Website Your online connection to the EMS world, JEMS.com gives you information on: • Products • Jobs • Patient Care • Training • Technology Product Connect The JEMS eNewsletter gives you breaking news, articles and product information. It’s free to subscribe … stay ahead of the latest news! Giving you the detailed product information you need, when you need it. We collect all the information from manufacturers and put it in one place, so it’s easy for you to fnd and easy for you to read. Go to www.jems.com/ems-products Archived Webcasts • PEARS: Helping You Help Kids • Lessons From Our Battlefelds: New Approaches to Shock Management • Securing the Airway: The Expanding Role of Extraglottic Devices • Maximizing Your Revenue • Advances in Assisted Ventilation: Where have we come from & where are we going? ® TM Free … Available 24/7! For more information on the JEMS Family of EMS Products: www.JEMS.com
- 20. PRIORITY TRAFFIC >> CONTINUED FROM PAGE 16 SERVING THOSE WHO SERVE Effectively treating military personnel & veterans F irst responders are a critical first contact point for members of the armed forces and veterans in crisis. Many EMS and other emergency response agencies aren’t effectively prepared to effectively serve those who serve. For example, first responders often don’t have sufficient knowledge of military culture and few know how to de-escalate calls involving military members and veterans. Special programming at this year’s 2013 EMS Today Conference & Exposition will focus on serving this special population. The conference will feature presentations by a team from Arizona’s Military/Veteran First Responder Initiative. This effort, facilitated by the Arizona Coalition for Military Families (ACMF), brings together public and private sector partners from the military, government and community to focus on strengthening crisis response for military members and veterans, including those experiencing post-traumatic stress and traumatic brain injury. The training, which has been developed by the ACMF over the past four years, is nationally recognized as a best-practice approach to improve the coordination of care through training and networking personnel. In the past year, through this partnership, more than 2,200 first responders in Arizona have received training, with plans for several hundred more this spring. This initiative fits into a larger state effort to build community capacity to care for and support service members, veterans and their families, including initiatives around behavioral health, higher education, employment and faith-based communities. The Arizona Coalition for Military Families and partners are currently exploring how to expand this training effort to reach first responders across the country. The presentation team at EMS Today Conference & Exposition will include Captain Dean Pedrotti of the Phoenix Fire Department, SSG (Ret.) Patrick Ziegert of the Office of the Arizona Attorney General and Colleen Day Mach of the Arizona Coalition for Military Families. The main presentation is Friday, March 8, from 8–10 a.m. with a presentation on post-traumatic stress on Saturday, March 9, from 10–10:30 a.m. — Thomas Winkel, MA, LPC, NCC DUTY TO ACT ARE YOU ALWAYS ON CALL? S cenario: A medic stops at the grocery store after her shift. She’s still in her company uniform and witnesses an older man drop to the floor, apparently unconscious. Does the medic have a legal duty to act? Probably not. If she chooses to walk on by, can she be held legally liable? Again, probably not. Why? Because she doesn’t have a legal duty to act. Tort law requires four elements for a plaintiff to hold a defendant legally responsible for a personal injury. These elements are 1) a legal duty to act; 2) a breach of that duty; 3) proximate causation (i.e., the defendant’s breach of duty was the legal cause of the plaintiff’s harm); and 4) damages (i.e., losses or harm that merits financial compensation). Unless an EMS provider has a legal duty to the patient, they cannot be held liable in tort law. In our scenario above, the medic was off duty, having completed her shift. The fact that she was in uniform doesn’t change the analysis; your legal duty to act isn’t dependent on your wardrobe. To use the reverse of this example, if the medic was on duty, spilled grape juice on her uniform at work and changed into a non-uniform shirt, she still has a duty to respond when called. Certainly, the fact that the medic was in uniform while off duty at the grocery store, probably with a patch or some insignia that identified her employer, still doesn’t create a legal duty to act when she witnessed the man fall to the floor. Of course, it could raise a public relations issue if the medic elects not to provide assistance to the patient, but it doesn’t give rise to a legal duty. As this scenario makes clear, there’s a difference between a legal duty and a moral duty. Certainly, many EMS providers feel they may have a moral duty to act in this scenario, though that is a personal decision that the law permits each of us to make based on our own values and beliefs. In fact, this is why most states have Good Samaritan laws: to incentivize people to act on behalf of a fellow human being in peril even though they may have no legal duty to do so. Can the medic’s employer be held liable for the medic’s failure to act? They possibly can in the court of public opinion, but not in tort law. If the agency is dispatched to respond, of course, that’s a different story. But her employer cannot be held liable simply because an offduty employee decided not to render aid as a bystander. What are the liability ramifications in this case if the medic does choose to act and provides care to the patient? Can the medic be held liable? Can her employer? Let’s start with the medic herself. When she decided to act voluntarily, most states’ laws would hold her liable only for harm that resulted from gross negligence, recklessness or intentional misconduct—not for acts of ordinary negligence. (Gross negligence vs. ordinary negligence is a threshold issue that is typically decided by the judge before the case goes to trial.) Some individual EMS providers choose to carry personal liability insurance to address concerns about personal liability, though in truth it’s quite rare for an EMS provider to have to pay out of their own pocket in a tort case. (In fact, we haven’t encountered it in our nearly 20 years in the practice of law.) Lastly, what is the liability of the medic’s employer if the medic chooses to act, in her uniform, while off duty? That is a bit more complex. If the employer has a policy (or even an unwritten expectation communicated to employees) making it a job requirement to provide off-duty care as a bystander, then it can possibly be held liable, because any errors or omissions committed by the medic would then likely be found to have occurred in the course and scope of her employment. However, in our experience, it’s unlikely (and inadvisable) for an EMS agency to have such a policy, which means the agency itself could most likely not be held liable for any acts or omissions committed by one of its employees off duty. The concept of a legal duty to act is a basic principle of tort law, and is the threshold issue in determining whether an EMS provider can face liability for their acts or omissions. Check out the most interesting and bizarre cases at jems.com/case 18 JEMS MARCH 2013 Pro Bono is written by attorneys Doug Wolfberg and Steve Wirth founding partners of Page, Wolfberg & Wirth, a national EMS industry law firm. Visit the firm’s website at www.pwwemslaw.com.
- 21. QUICK TAKE AWARD WINNERS FireEMS blogger, JEMS sister sites gain recognition Fire/EMSBlogs blogger Michael Morse, who pens the Rescuing Providence blog, was one of three Rhode Island writers who received the prestigious MacColl Johnson Fellowships from the Rhode Island Foundation. Morse, who was one of three writers to receive $25,000, writes about his work as an EMT/firefighter with the Providence Fire Department at http://rescuingprovidence.com. Two JEMS sister publications were named Jesse H. Neal Awards competition finalists. The Law Officer Facebook page is up for Best Use of Social Media, and FirefighterNation. com is being considered for Best Website. The American Business Media considers the Neal Awards the industry’s most prestigious and sought-after editorial honors. BOOK REVIEW Alright, Let’s Call it a Draw: The Life of John Pryor By Richard (and John) Pryor, based on the life and death of John Pryor, MD John P. Pryor, MD, FACS, former trauma program director for the Hospital of the University of Pennsylvania in Philadelphia, JEMS author and JEMS Editorial Board member, was killed by an enemy mortar round in Mosul, Iraq on Christmas morning of 2008. This posthumous biography, penned by John’s younger brother, Richard, is a moving and in-depth look into the life of an EMT turned trauma surgeon. It provides a rarely written view of the motivation and dedication behind heroic behavior. John Pryor’s journey began as a humble EMT in upstate New York. Like many JEMS readers, an inner voice compelled John to serve his fellow man. Ultimately, he decided that he wanted to be a surgeon. This seemingly impossible dream led him to Grenada in the Caribbean, Buffalo, N.Y., and Philadelphia as well as onto the pile at the World Trade Center on Sept. 11, 2001. Reading this book helps one realize that anything can be accomplished once you set your mind to doing so. It’s also a powerful and sometimes painful insight into the costs involved in achieving these dreams. Alright, Let’s Call it a Draw is an eloquently detailed compilation of stories and incidents that became the pivotal moments in the life of Dr. John Pryor. It details the life events that made him a man of conviction, a man of integrity, and a family man. This book reveals the unique characteristics of John’s life that resulted in an exceptional individual whose family, colleagues, friends and all who knew him would ultimately be proud of. Every EMS provider will see a little bit of themselves in the life of John Pryor. Anyone who ever wondered what medical school is like will gain an inside perspective. This book is a must read for every emergency services provider. You won’t be able to put it down. To obtain a copy, go to www.drjohnpryor.com. —Mike McEvoy, PhD, REMT-P, RN, EMT-P & A.J. Heightman, MPA, EMT-P Choose 20 at www.jems.com/rs
- 22. LEADERSHIP SECTOR PRESENTED BY THE IAFC EMS SECTION >> BY GARY LUDWIG, MS, EMT-P IMPACT AHEAD I t’s final! In June 2011, the U.S. Supreme Court upheld the Patient Protection and Affordable Care Act (PPACA), commonly known as Obamacare. This past November, President Barack Obama won reelection and Democrats maintained a majority control of the Senate. Any hopes Republicans had of repealing the law went away with those two opportunities. By the end of Obama’s second term, many of the PPACA’s core components will have been in effect for three years or more. There’s really no turning back; healthcare as we know it is going to change. The healthcare bill was 2,733 pages long and EMS is only referenced a few times in the document. But the effect on EMS will be dramatic. I suspect that many EMS systems will look totally different in 10 years. I know; you’ve heard this rhetoric before. About 15 years ago, we heard that managed care organizations would be the “gatekeepers” that would keep people from unnecessarily calling 9-1-1 to go to an emergency department (ED). We heard that call centers for insurance providers would properly evaluate the caller and route them to the appropriate level of care instead of calling 9-1-1. Those changes largely failed to materialize. CHANGES TO MANAGED CARE The problem with managed care is that it was mainly an effort by some insurance providers to control costs and profits, and it was voluntary. The PPACA will be legally required. Besides the 2,733 pages of the bill itself, more than 14,000 pages of federal regulations have already been written. In addition, the PPACA is partially funded through tax reforms (e.g., a 2.3% tax on medical devices costing more than $100). Expect those manufacturers to pass that cost on to you when you purchase devices costing more than $100. Although nobody truly knows how these changes will affect healthcare, there’s one thing we can be sure of: People are still 20 JEMS MARCH 2013 PHOTO ALLKINDZA/ISTOCKPHOTO.COM Obamacare will transform future EMS systems readmittals and other quality of care issues, hospitals may partner with the local EMS system to perform a variety of services. These can include checking on the patient with home visits for the first three days, or if complications arise, transporting the patient to another level of care. START PREPARING NOW EMS managers should prepare now for the changes that are coming. As patients with insurance are moved to management systems and existing Medicare patients are moved to ACOs, prepare for initial call load increases. This should be followed by a leveling-off period. Start meeting with your local hospital administrators to discuss partnerships that can come about with the implementation of the PPACA. As the saying goes, “Chance favors the prepared mind.” EMS systems that start preparing for the long-term impacts of the PPACA will no doubt reap the benefits. going to get shot, have heart attacks at the ball game and get into auto accidents going home from work. Our 9-1-1-based EMS systems will still be needed to address such medical emergencies. What’s most likely to change for EMS is how we deal with chronically ill patients who call 9-1-1 because they have waited too long to address their medical problem or because they lack health insurance and use the ED as an entry into the healthcare system to address their problem. For Medicare patients, these needs will most likely be met through accountable care organizations GLOSSARY (ACOs), which are just starting to form. The main function of an Accountable The main function of an ACO is to moniCare Organization (ACO) is to monitor tor and control reimbursements for healthand control reimbursements for healthcare providers while also monitoring the care providers while also monitoring the quality of the care being provided. The quality of the care being provided. The PPACA allowed for the establishment of a PPACA allowed for the establishment Medicare Shared Savings Program (MSSP), of a Medicare Shared Savings Program which allows for ACOs to contract with (MSSP), which allows for ACOs to conMedicare. Under this type of scenario, the tract with Medicare. Under this type of ACO would need to be totally responsible scenario, the ACO would need to be for the quality, cost, care and management of totally responsible for the quality, cost, at least 5,000 Medicare recipients. care and management of at least 5,000 An ACO can deny or reduce payment if Medicare recipients. the provider isn’t meeting quality standards. For example, reimbursement can be denied when a patient is readmitted to a hospital within three days for the Gary Ludwig, MS, EMT-P, is a deputy same problem. It’s therefore in that fire chief with the Memphis (Tenn.) Fire hospital’s interest to make sure the Department. He has 30 years of fire and patient doesn’t get readmitted for the rescue experience. He’s chair of the EMS same problem. Section for the International Association of Fire How does this affect EMS? To avoid such Chiefs and can be reached at www.garyludwig.com.
- 23. Choose 21 at www.jems.com/rs
- 24. TRICKSOUR PATIENTS & OURSELVES OF THE TRADE CARING FOR >> BY THOM DICK, EMT-P BATTERIES Preventing failures we can’t afford I PHOTO THOM DICK survived a grade-school envilate-model diesel depends on a supronment where academic failure ply of urea (and why). And that if meant physical pain. My teacher you’re having steering issues, the first would command me to put my hands thing you should wonder about is on my desk, and she would play rap the air pressure in your tires. Think music on them with a maple pointer. of it the way you think about anatAnd that was nothing, compared to omy and physiology. what awaited me at home when my By far, the most common kinds of dad returned from work. critical failures I’ve seen are failures My crime: not “applying” myself. to start. It turns out, they’re also the Nothing less than a B would do, easiest to prevent—partly by crews because in Pop’s view, non-achievewho understand their instruments, ment meant lack of effort. and partly by proactive agencies Looking back, I don’t recall my that adhere to scheduled preventive slightly neurotic teachers enjoying Batteries eventually fail, no matter what we do. Preventing replacement of their batteries. their work any more than I did mine. failures to start is the key to making sure those failures The thing about batteries is they don’t harm a patient. And not surprisingly, they sucked at it. all eventually fail. A good commerI loved auto shop, though; got straight As you know, an ambulance can either cial ambulance-sized battery should cost As in auto shop. Auto shop, music and writ- earn you a living or kill you on any day of about $200, and the average ambulance ing. Grew up with Rochester QuadraJets, your career. It can kill other people, too. To has two of those. They should be replaced 235 and 327 Chevy engines, and VW bugs. operate, it needs to be able to start, steer, about once a year (even if they work just Listened to the Wolf Man every night, play- stop and stay running. It also needs to pro- fine), they should be protected from rapiding Patsy Cline, Gene Pitney, The Righteous vide a stable interior environment, and its charging, and their connections should be Brothers, Motown, and later The Beach safety restraints need to work. You don’t kept tight and squeaky-clean. You know Boys and Beatles. Idolized Walter Cronkite need a mechanic or a supervisor to tell you what they’ll cost, so you can budget for and dreamed of being him someday. Then when any of those systems fails; and when their replacement. in 1970, as a young journalism student, I they do, you’re like a pilot. Nobody gets to Now let’s think about the consequences found a job as an ambulance attendant. I argue with your decision to put yourself of a failure. When a battery fails, it’ll typiinstantly recognized my calling in life. Of out of service. cally do so when you least expect it to. course, if you worked for an ambulance serI’ve learned to see critical failures not You can’t project what it’ll cost. A pair of vice in those days, it was probably a small just as events that prevent you from run- dead ones is too big to jump-start, they one. And in small organizations, everybody ning calls, but as events that could pre- place unacceptable stress on alternators, does more than one job. vent you from running calls. So, an engine they generate towing bills and they’re surOne of my jobs between calls was man- that cranks hard or leaks fluids needs to rounded by three-sided billboards that aging a fleet: tracking the licenses, buying be taken out of service. So does a tire that say “we screwed up.” And worst of all, the batteries, checking the tires and log- reveals excessive or unusual wear. they interrupt our basic mission of helpging the maintenance. I was untaught, so I In fact, your ambulance will almost ing sick people. made a lot of mistakes. But I loved ambu- always warn you before it fails. So you Don’t think this is important? OK, Lifelances, and I learned a ton about what probably deserve to understand how Saver. Put your hands on the table makes them safe and reliable. I take care of it works and what it’s telling you. in front of you. ... a fleet to this day. Mechanical education is partly Thom Dick has been involved in EMS There are two kinds of vehicle failures, your agency’s responsibility and for 41 years, 23 of them as a full-time Life-Saver. One is the kind that takes you partly yours. Given your access to EMT and paramedic in San Diego County. out of service immediately. Most agencies the Internet, there’s no reason why He’s currently the quality care coordinacall those critical failures. The other kind, a you shouldn’t know some of the non-critical failure, needs to be fixed none- same stuff your vehicle tech knows. For tor for Platte Valley Ambulance, a hospital-based theless. But it won’t keep you from run- instance, that a cracked windshield can 9-1-1 system in Brighton, Colo. Contact him at ning a call. defeat your airbag restraints. That your boxcar414@comcast.net. 22 JEMS MARCH 2013
- 25. A REVOLUTION IN EMERGENCY CARE NEW DESIGN Clinicians can deliver aerosol & CPAP therapy with Only One oxygen source. EZ ADVANTAGE: INTEGRATED NEBULIZER Offers the capability of an in-line nebulizer. ∙ Uses only one oxygen supply source ∙ Easy Set-Up, Less Parts. ADVANTAGE: CPAP SYSTEM CONSUMES 50% LESS OXYGEN Neb Off Neb On CPAP conserves oxygen while maintaining high FiO2 delivery Increasing flow may be necessary when activating the nebulizer. ADVANTAGE: BUILT-IN MANOMETER & PRESSURE RELIEF VALVE SAFE, SURE, SUPERIOR CPAP. ADVANTAGE: ADVANCED MASK DESIGN ∙ Quick Disconnect Clips ∙ Straight Rotating Port ∙ Soft Forehead Padding to reduce pressure on nose. ∙ CPAP & Nebulizer in One System ∙ Less Parts, Easy Set-Up ∙ Only One O2 Source With so many advantages, it clearly puts you at an advantage. Choose 22 at www.jems.com/rs www.mercurymed.com Visit Mercury Medicalʼs Booths #1431 & #1432 at the 2013 EMS Today Conference & Expo Walter E. Washington Convention Center Washington, D.C. March 7 - 9, 2013
- 26. CASE OF THE MONTH DILEMMAS IN DAY-TO-DAY CARE >> BY MICHAEL ORLAND, MD FORWARD FALL Get a handle on handlebar injuries I t’s 2 a.m. on a Friday night and a medic unit responds to a call of a “pedestrian struck.” On arrival, city law enforcement declares the scene to be safe and directs the unit to the opposite shoulder of the highway. EMS providers find a 35-year-old male lying in the prone position with a moderately damaged mountain bike beside him. The patient says he was riding home from his friend’s house when he got “bumped” by a passing car, hit a pothole and fell forward off his bike. Although his breath indicates recent alcohol intake, he’s able to answer questions in a moderately slurred voice. Initially the patient refuses medical evaluation and transport to the hospital, but the medics are able to convince him otherwise. The airway is intact with no debris or blood, and breath sounds are equal bilaterally. His respiratory rate is 22 and pulse oximetry 96% on room air. A cervical collar is placed on the patient, and he is log-rolled and secured onto a backboard. The heart rate is found to be 110 mmHg with a blood pressure of 136/92. His helmet has an abrasion to the front but is otherwise intact. Your trauma exam is notable for a 2x3 cm round-shaped wound to the midline epigastric region, just inferior to the xiphoid process, with moderate non-pulsatile bleeding. You note that when the patient exhales following a deep inspiration, there’s a small bulge in the wound that subsequently resolves with the following inspiration. No air movement or bubbling from the wound is detected. The abdomen is mildly distended with moderate diffuse tenderness and there are multiple partial thickness abrasions to the bilateral elbows, hands and lower extremities. Although he’s clinically intoxicated, his Glasgow Coma Scale (GCS) is determined to be 15. 24 JEMS MARCH 2013 PHOTOS COURTESY EDWARD T. DICKINSON ASSESSMENT & TREATMENT A deep breath by the patient produces a small bulge in the ring-shaped wound, indicating traumatic abdominal hernia. Once in the mobile unit, you place the patient on 4 lpm oxygen via nasal cannula and a cardiac monitor. You secure a sterile abdominal gauze pad over the open abdominal wound. The total scene time is 12 minutes, and transport time to the local trauma center is 20 minutes. You place an 18-gauge IV in the patient’s right antecubital fossa and administer 500 ccs of normal saline en route. The dressing controls the bleeding from the abdominal wound, and there’s no significant clinical change in the patient during transport. TRAUMA CENTER CARE On arrival to the trauma center, the trauma team repeats the primary and secondary surveys. Vital signs arenít significantly changed: Heart rate is 112, respiratory rate is 18, blood pressure is 132/88, and pulse oximetry is 100% on room air. The trauma team also performs a focused assessment with sonography for trauma (FAST) exam, which demonstrates a small amount of free fluid in the right upper quadrant, specifically Morrisonís pouch. A FAST exam, which is regularly performed during a trauma survey, uses four different locations to place the ultrasound and screen for free fluid in 10 distinct potential spaces. Free fluid, often blood in the traumatic patient, is a strong indicator of significant abdominal or thoracic injury, and the FAST exam allows early identification of these patients in order to expedite surgical intervention. Morrison’s pouch is a potential space between the inferior aspect of the liver and superior aspect of the right kidney. It is recognized as the most likely location to identify free fluid associated with a serious intra-abdominal injury. Given the stable vital signs, a CT scan of the head, cervical spine, chest, abdomen and pelvis is performed to fully evaluate the injuries. The CT scans demonstrate
- 27. Choose 23 at www.jems.com/rs
- 28. CASE OF THE MONTH >> CONTINUED FROM PAGE 24 IMAGE COURTESY EDWARD T. DICKINSON hernia will appear as a discrete bulge on abdominal exam that may expand and reduce with a change in abdominal pressure or remain constant. It’s important to recognize this clinical sign and its association with significant traumatic injuries, but no other specific care should be performed except for a sterile dressing application to any open wounds. Application of manual pressure or compression of any kind to the mass isn’t advised because it may exacerbate other injuries. CONCLUSION This CT scan demonstrates a 2 cm anterior fascial defect and associated abdominal wall hernia at the site of the open wound. a 2 cm anterior abdominal wall hernia at the site of the open wound, injury to two areas of the small bowel with likely perforation given the surrounding small foci of free air and a grade 2 liver laceration. The patient is immediately taken to the operating room, where he undergoes an exploratory laporatomy with resection of two portions of the small bowel, suture repair of the liver laceration and primary repair of the abdominal hernia with mesh. His post-operative course is uneventful, and the patient is discharged to home one week later. DISCUSSION At first glance, a fall from a bicycle can often be mistaken as a non-significant mechanism. As is often the case with lateral falls, a low level of energy is being distributed to a large area of the body or to an extremity. However, forward falls from a bicycle are frequently higher energy, which is distributed to a smaller area of the body. More specifically, the body can be struck in the chest or abdomen by the handlebars or the head by the ground or stationary object. This focused impact in combination with increased abdominal pressure as a result of the initial impact of the bicycle places the patient at significant risk of injury to the abdominal wall and anterior abdominal organs, including the liver, spleen, stomach, bladder, colon and 26 JEMS MARCH 2013 small bowel. Therefore, any patient who falls at a high rate of speed or falls forward off of a bicycle should be considered to have suffered a significant mechanism of injury and treated as such. Blunt traumatic injuries from a bicycle handlebar are more common in the pediatric population. A two-year retrospective chart review at a major children’s hospital found an average age of 8.8 years for this injury, with 79% of patients in this population being boys. Of the 14 patients who presented for evaluation to the ED, 11 had a ring-shaped ecchymotic area noted in the abdomen with a variety of lacerations and abrasions. After evaluation, it was found that 21% had an intestinal perforation and 21% had an abdominal wall hernia, as large as 5 cm.1 In the multiple case reports published, traumatic abdominal wall hernias due to a handlebar injury more often occur in the lower abdomen and appear as a ring- or circular-shaped ecchymosis, abrasion or open wound. In the pediatric population, a handlebar injury is the most common cause of a traumatic abdominal hernia and isn’t a reliable indicator for more significant traumatic injuries. In contrast, seatbelt trauma in a motor vehicle collision is the more frequent mechanism for abdominal hernias in adults and is almost always associated with other significant injuries.2 Clinically, a traumatic abdominal wall In this case, the ALS unit provided prompt and efficient care for their trauma patient; starting with airway, breathing and circulation (ABCs), and proceeding through spinal immobilization and secondary examination. They recognized the significant mechanism and were able to persuade the patient to receive the care he required. Large-bore IV access was obtained, fluid resuscitation was initiated and appropriate wound care was provided—all while expediting transport to a trauma facility. In summary, falling forward onto a bicycle places a patient at risk of a handlebar injury and should be considered a significant traumatic mechanism that may cause serious abdominal injuries with no major outward signs of trauma on exam. A traumatic abdominal wall hernia will appear as an area of ecchymosis or small wound with an underlying bulge. Although this doesn’t require specific care, it should be recognized as a significant injury. In adults, it may indicate additional serious abdominal injuries. As such, these patients should be transported expeditiously to the closest trauma center. Michael Orland, MD, is a resident physician in emergency medicine at the Hospital of the University of Pennsylvania and a former EMT with the Pennington First Aid Squad. He can be reached at Michael.Orland@ uphs.upenn.edu. REFERENCES 1. Karaman I, Karaman A, Aslan M, et al. A hidden danger of childhood trauma: Bicycle handlebar injuries. Surg Today. 2009;39(7):572–574 2. Haimovici L, Papafragkou S, Kessler E, et al. Handlebar hernia: Traumatic abdominal wall hernia with multiple enterotomies. A case report and review of the literature. J Pediatr Surg. 2007;42(3):567-569.
- 29. Choose 24 at www.jems.com/rs
- 30. 28 JEMS MARCH 2013 PHOTO BY CHRIS SWABB
- 31. TIME FOR A CHANGE >> BY JIM MORRISSEY, MA, EMT-P rehospital spinal immobilization has long been r held as the standard of care for victims of blunt h or penetrating trauma who have experienced a o mechanism of injury (MOI) forceful enough to m possibly damage the spinal column. The majority p of EMS textbooks stress that any significant MOI, regardless of f b signs and symptoms of spine injury, requires full-body immobilization, which is typically defined as a cervical collar being applied and the patient being secured to a backboard with head stabilizers in place. This approach to patient immobilization has been accepted and implemented as the standard of care for decades with little scientific evidence justifying the practice.1–3 In addition, scant data shows that immobilization in the field has a positive effect on neurological outcomes in patients with blunt or penetrating trauma.1,4–6 In fact, several studies and articles show that spine immobilization may cause more harm than good in a select sub-set of trauma patients.5–7 Many experts question the current practice of prehospital spinal immobilization.1,2,4–15 There are now some guidelines, textbooks and an increasing number of EMS agencies that support a progressive, evidence-based approach in an effort to lessen unnecessary spinal immobilizations in the field. It’s problematic to use MOI alone as the key indicator for prehospital spinal immobilization. In addition, the harmful sequelae and potential dangers of spine immobilization need to be considered in any field protocol. We need to examine appropriate spine injury assessment guidelines and algorithms that allow for the selective immobilization of injured patients. We also should review immobilization devices and techniques that are more appropriate for patients who do require immobilization, or better termed, spinal motion restriction (SMR), by EMS providers. OUTDATED INDICATORS? It typically takes several years for EMS textbooks to catch up with new evidence and then additional time for the EMS instructional community to modify curricula and change current practice. For example, definitions of mechanisms that require spinal immobilization found in most EMS textbooks are outdated and problematic. Such indicators for potential spine injury as fall, damage to the vehicle, injury above the clavicle and mechanism of injury involving motion, are not particularly helpful when determining the best course of action in the field. Especially troubling has been the lack of emphasis on the assessment of the patient before making a decision about immobilization. Historically, more emphasis has been placed on what happened to the vehicle or the best guess on how far someone may have fallen, instead of what actually happened to the person. It isn’t the fall that causes injury; it’s the sudden stop at the end. The more sudden the stop, the more likely an injury results, especially if the kinetic energy was transmitted to the head and/or neck. The physical condition of the patient must also be considered. A young, athletic person is able to withstand more forces than an elderly patient. So the spectrum of potential injuries is best determined through a detailed history and physical exam. Vehicle damage has long been considered a strong indicator of potential spine injury, yet improvements in vehicular design and construction should change the way we look at vehicle damage. Vehicle technology and passenger protection is far superior to what it has been, particularly since the 70’s when EMS textbooks began advocating back boarding of patients in vehicles with significant damage. Vehicle damage zones are now inherently built into newer WWW.JEMS.COM MARCH 2013 JEMS 29
- 32. SPINAL IMMOBILIZATION >> CONTINUED FROM PAGE 29 PRECAUTIONARY IMMOBILIZATION PHOTO COURTESY JIM MORRISSEY/JOSH KENNEDY It isn’t surprising that the term and practice of “precautionary immobilization” has developed. It’s estimated that at least five million patients are immobilized in the prehospital environment in the U.S. each year. Most have no complaints of neck or back pain or other evidence of spine injury.3,11,12 (See Photo 2.) EMS personnel historically have neither been given the tools nor the authority to make informed decisions about objectively determining the need for prehospital spinal immobilization. This may be because the emergency medical community thought immobilization was always safe, conservative and always in the best interest of the patient. However, evidence now shows that, in some cases, spinal immobilization may not be in the patient’s best interest.1–3,7,8,10–13 Some prehospital care providers will admit that they often immobilize patients without evidence of spine injury because they want to avoid being questioned on arrival at the emergency department (ED). This dynamic can (and must) change with education and outreach. BACKBOARD-BASED IMMOBILIZATION There are many situations (hostile environment, life threatening injuries) where spinal immobilization may be detrimental to good patient care. This training scenario emphasizes rapid extrication. 30 JEMS MARCH 2013 victims of penetrating trauma without neurologic deficits.20 In the setting of drowning, the 2010 evidence-based guidelines from the American Heart Association state that “Routine c-spine immobilization is a Class III (potentially harmful) unless clear trauma is evident in the history or exam, because it may unnecessarily delay or impede ventilations. ”21 PHOTO A.J. HEIGHTMAN vehicles, designed to absorb and dissipate the kinetic energy of a collision, and keep the passenger cabin relatively isolated and protected.16 An experienced paramedic once said, “The cake box might be crumpled, but the cake can be fine.” Some textbooks accurately address this issue. Even as far back as 1990, the American Academy of Orthopaedic Surgeons addressed emergency medical responders in an extended-care environment, stating, “Patients with a positive mechanism of injury, without signs and symptoms, and with a normal pain response may be treated without full spine immobilization, if approved by your medical control physician.” 17 Emergency medical personnel who work in extended-care, tactical, combat and wilderness environments have long realized the need to safely and accurately assess and clear patients regarding spinal injuries.18,19 New guidelines from Prehospital Trauma Life Support and the National Association of EMS Physicians have diminished the emphasis on immobilizing Assessment is still the key to determining the need for spinal immobilization. In addition to patient discomfort and anxiety associated with backboard-based immobilization, there are several potentially significant consequences. Standard immobilization requires the patient’s body to conform to a flat, hard surface. In addition, EMS secures a cervical collar around the patient’s neck and uses tape to secure the patient’s head to the board. This practice often increases patient anxiety and has the potential to aggravate underlying injuries. Standard spinal immobilization techniques can also take away the patient’s ability to effectively protect their own airway thus significantly increasing the risk of aspiration.3–6,11,13 Patient vomiting, bleeding, airway drainage and swelling are common problems associated with trauma patients. Even with one EMS provider dedicated to the management of the airway and patient suction, it cannot be assumed that a suction catheter can handle the job when significant bleeding and/or vomiting is presented. The continued spinal stability of a patient who is turned on their side to facilitate airway drainage and control is also questionable. Patients typically experience a significant
- 33. Choose 25 at www.jems.com/rs Choose 26 at www.jems.com/rs
- 34. SPINAL IMMOBILIZATION PHOTO COURTESY JIM MORRISEY/JOSH KENNEDY >> CONTINUED FROM PAGE 30 Patients with penetrating trauma (ex., gunshots and stabbings) to the head and torso usually do not benefit from spine immobilization. shift in body weight and distribution, causing more movement to the spine than the immobilization process was intended to prevent. In a comprehensive review published in Prehospital and Disaster Medicine, healthy volunteers who were immobilized on a backboard were found to be “significantly more likely to complain of pain when compared with immobilization on a vacuum mattress.” Adverse effects of backboard-based immobilization documented in this study include increased ventilatory effort, pain and discomfort. In addition to pressure injury, the backboard may also be the cause of pain—even in otherwise healthy volunteers. The resultant posterior surface/back pain of immobilized patients has been documented to result in unnecessary radiographs and potential clinical ambiguity regarding the cause of the pain.3,22 There’s an increased cost associated with some of these complications. It has been documented that supine patient immobilization results in a 15–20% reduction in respiratory capacity, and that respiratory effectiveness is markedly reduced by the strapping systems typically used.3,9,13 Patients are often either strapped securely, thus having diminished respiratory capacity, or loosely secured, facilitating easier breathing. Neither scenario is ideal. The challenge is exacerbated in obese patients, the elderly and patients with such underlying diseases as congestive heart failure, COPD, asthma and pneumonia. Done properly, immobilization in the field takes time and multiple personnel. Time delay to the ED or trauma center arrival has been cited as a significant problem for critical trauma victims. Several studies have looked at the risk vs. benefit of prehospital immobilization, with several authors and researchers questioning the value of current practices.1,2,7,8,11,15 Choose 27 at www.jems.com/rs 32 JEMS MARCH 2013
- 35. Studies have also shown limited or no benefit of prehospital immobilization of penetrating trauma patients. (See photos on pages 32 and 33.) Unnecessary immobilization of this subset of trauma patients can result in prolonged on-scene time and delayed transport to definitive care, which may increase morbidity and mortality.4–6,14,18,23–25 Several studies show that cervical collars by themselves aren’t without risk or significant consequences.4,26–28 One study concludes that cervical collars frequently increase intracranial pressure and may be particularly harmful if used on head-injured patients.26 Another researcher observed that cervical collars “can result in abnormal distraction within the upper cervical spine in the presence of severe injury.”28 In addition, cervical collars hide areas of the head and neck, resulting in the increased possibility of missing injuries or evolving problems, such as swelling, hematoma and tracheal deviation.27,28 In addition, the longer a patient is immobilized, the more likely that cutaneous pressure ulcers will develop, most notably in the occipital, sacral or heel areas.9,12,22,29,30 This is especially true in elderly, unconscious and neurologically impaired patients. This problem may be significantly reduced with padding or use of a vacuum mattress. Unfortunately, the vast majority of the patients who are immobilized don’t get padding in voids or areas of significant body weight/pressure or a vacuum mattress that distributes beads/padding in voids and uneven body surface areas. THE PENETRATING TRAUMA PATIENT As referenced earlier, there is a growing body of evidence that suggests penetrating trauma victims shouldn’t be routinely immobilized. Immobilization has been associated with higher mortality in patients with penetrating trauma.4–6,14,23–25 Independent studies show that whether the penetrating trauma is to the head, neck or torso, immobilization is unnecessary, interferes BEGIN THE CHALLENGE AT: PHOTO COURTESY JIM MORRISSEY/JOSH KENNEDY heart.org/acls-ep Tactical teams often use compact, flexible extraction devices. Choose 28 at www.jems.com/rs WWW.JEMS.COM MARCH 2013 JEMS 33
- 36. SPINAL IMMOBILIZATION >> CONTINUED FROM PAGE 33 with and delays emergent care, and should be seriously reconsidered as the standard of care.4–6,14,23 A Journal of Trauma article concluded, “Indirect spinal injury does not occur in patients with gunshot wounds to the head.” The authors state, “Protocols mandating cervical spine immobilization after a gunshot wound to the head are unnecessary and may complicate airway management.”14 Another retrospective study showed similar concerns about the use of a cervical collar with patients who have penetrating injuries to the neck. This study suggests that avoiding the collar should be the rule, and that a provider who chooses to apply a cervical collar should have good justification. The authors also suggest that frequent examination of the underlying structures and tissue is warranted if a cervical collar is used.4 A comprehensive retrospective analysis of gunshot injuries to the torso found that immobilization was of little or no benefit, even if an unstable spine fracture was present. The authors argue that airway management, including intubation, is far more complicated and problematic with prehospital spinal immobilization in place.5,6 In fact, failed airway management was reported to be the secondleading error preceding death of trauma patients, accounting for 16% of mortality in one study. This study also highlights the potential delay to definitive surgical treatment and the lack of neurologic improvement after gunshot injury to the spinal cord, suggesting that prehospital spinal immobilization is unjustified.5,6 PROPER SPINE INJURY ASSESSMENT AIRPOWER® R8 Lower profile zipper Station/EMS boot > Built in Arch Support > Steel toe protection > Chemical/bloodborne pathogen protection > Waterproof & breathable Quality shoes for law enforcement, fire and rescue services, hunting, work wear, and leisure time HAIX® North America Inc. 2320 Fortune Drive, Suite 120, Lexington KY 40509 Phone 859-281-0111, Fax 859-281-0113, Toll free 866-344-HAIX (4249) Visit us at DAY EMS TO 49 0 Booth 1 www.haix.com Choose 29 at www.jems.com/rs 34 JEMS MARCH 2013 For many trauma patients, a vetted field assessment criterion that focuses on the assessment of the patient rather than the mechanism of injury would obviate unwarranted immobilization.3,11,31 Many emergency medicine specialists believe an accurate, reliable, simple-to-perform spinal injury assessment could reduce spine immobilizations drastically. Thankfully, there is a trend in this direction across the nation. The idea of “clearing” a patient of spinal injury in the field has been, and continues to be debated. However, there are prehospital spine assessment protocols that safely and accurately allow EMTs and paramedics to omit prehospital spinal immobilization in certain patients. Some EMS experts prefer the term “selective immobilization” to “clearing” the c-spine, but the end result is the same. The end result is the reduction of the incidence of unwarranted spinal immobilizations. For example, the Maine spine injury assessment guidelines, developed by Peter Goth, MD, in the 1990s, have been shown to be accurate and safe.10,31,32 Several states and EMS systems around the nation use this, or a similar protocol, to help decrease the number of trauma patients being subjected to prehospital spinal immobilization. The origin of this type of spinal assessment was initially intended to help ED physicians clinically decide if they can safely clear patients from prehospital spinal immobilization and reduce or eliminate unnecessary radiographic studies. It has been shown that the proper clinical exam and history is more accurate at predicting spine injuries than X-ray review.10,32–35 The spine injury assessment guidelines that have been adopted
- 37. PHOTO COURTESY JIM MORRISEY/JOSH KENNEDY by multiple prehospital systems are based on the Canadian C-spine rule and the National Emergency X-Radiography Utilization Study (NEXUS) low-risk criteria. Each has similar parameters, requiring that the patient be awake, alert, conversant and without significant distracting injury or intoxication. In addition, the guidelines further state that the physical exam should reveal no pain or tenderness to the posterior neck and back and the neurologic exam must find normal motor and sensory function in the extremities.10,18,31,33–35 Studies show that prehospital care providers can safely apply spine injury assessment criteria and not miss any clinically significant spine injuries.10,31,32 Although these guidelines are PHOTO CHRIS SWABB Some patients, such as pediatric patients, require special spinal immobilization consideration. Children have been immobilized acceptably in specialized spinal devices for decades. Choose 30 at www.jems.com/rs WWW.JEMS.COM MARCH 2013 JEMS 35
- 38. SPINAL IMMOBILIZATION Patients can be immobilized safely and comfortably via a combination of a backboard or other flexible or scoop-type stretcher, such as shown here with a Hartwell Combi-Carrier/vacuum mattress combination. However, long-established norms are hard to break, and extensive training was required to make this new policy successful. EMS schools, fire departments and other EMS providers, as well as emergency department staff, needed to be exposed to the literature and trained in the new protocol. Initial training and outreach has been well received and the early indicators have shown a significant reduction in spine immobilizations. The end result is: >> A better understanding of the need for expeditious care under specific circumstances, in particular, the need to move rapidly when penetrating trauma is present; >> All involved are empowered to break the paradigm of “board them all” as a result of understanding the importance of proper spinal/neurological assessment and assessment parameters that allow crews to assess for serious spinal indications and perform selective immobilization. We did the same process decades ago when we adopted rapid removal techniques for 36 JEMS MARCH 2013 PHOTO A.J. HEIGHTMAN A vacuum splint can be used as a highly moldable and comfortable cervical immobilization device. of patients. Many of these devices are better suited to patient movement in tight spaces and crew body mechanics when carrying and transferring patients down stairways and other difficult environments. Of course, crews have to take special caution when dealing with and managing high-risk patients, including pediatric patients, the elderly and those with such degenerative bone disorders as osteoporosis. Field personnel need to be conservative while evaluating these patients and should provide spinal motion restriction when in doubt.33,34 UNCONVENTIONAL OPTIONS Even with appropriate application of spine injury assessment guidelines, some patients still require some degree of prehospital spinal motion restriction. Vacuum mattresses and other break-away and flexible stretchers have been used successfully throughout Europe for years. They score well in several critical areas, including patient comfort, secure immobilization, insulation, lack of pressure PHOTO A.J. HEIGHTMAN patients in lieu of spending precious minutes placing splints and half backboards on critical patients. Little or no untoward results occurred with that change in procedure; >> More attention to patient comfort and pain instead of routine placement of trauma patients on a hard, uncomfortable platform that often put them in anatomically-incorrect positions for extended time periods, made patients unnecessarily claustrophobic lying supine and immobile and exacerbation of respiratory distress in patients due to the supine position, strap placement, and existing conditions such as CHF, COPD or morbid obesity; and >> The ability to deploy and maximize the usage of alternative immobilization and transfer devices and stretchers such as vacuum mattresses, scoop or CombiCarriers and flexible stretchers such as Ferno and SKED stretchers and others that feature lateral patient support slats and multiple handles for convenient movement and transfer PHOTO A.J. HEIGHTMAN available, training and practice is needed to become proficient at using these criteria. Alameda County (Calif.) EMS has revised its spine injury assessment protocol to accurately reflect the current literature and research. (See Figure 1, p. 38). Its goals in 2012 were to reduce unnecessary immobilization, and use treatment modalities in the best interest of and provide the most comfort to the patient. In some cases, this meant forgoing prehospital spinal immobilization to expedite transport to a trauma center. PHOTO ED DOERR >> CONTINUED FROM PAGE 35 This patient is securely immobilized in a FERNO Germa Easyfix vacumm mattress – stretcher. Vacuum mattresses and stretchers pad voids and distribute a patient’s weight evenly.
- 39. Choose 31 at www.jems.com/rs HealthEMS® Mobile • Industry–Leading ePCR Secure field data collection using your hardware of choice • HealthEMS® FlexFields Unique functionality creates customized ePCR • HealthEMS® Integrates to CAD and EKG Wireless data exchange eliminates manual entry improving accuracy • HealthEMS® XchangER Two-way wireless communication of ePCR data to/from hospital HealthEMS® EHR • Industry-Leading EHR Advanced QA solution supports CQI • HealthEMS® Xchange NEMSIS Gold compliant, v3 development in process • HealthEMS® is CARES Compliant; Sansio is the IT partner of the CARES network • myPatientEncounters™ Provides patients with secure, online access to their EHR NEW • • • • EMS Web-Based Revenue Cycle Management Solution! Improved efficiency with ePCR system integrated to billing system Accurate/Automatic ICD-9/10 coding, medical necessity, service level, loaded mileage, eligibility checking HIPAA Compliant Transactions 4010/5010 electronic claims and remittances Complete AR Management Workload management/change management and reporting Visit www.HealthEMS.NET or call 877.506.2747 for Demo #1 EMS Software as a Service (SaaS) Solution – Over 25% Top EMS Agencies Use HealthEMS® Sansio 11 East Superior Street, Suite 310 Choose 32 at www.jems.com/rs Duluth, MN 55802
- 40. SPINAL IMMOBILIZATION >> CONTINUED FROM PAGE 36 Figure 1: Alameda County (Calif.) 2012 Spinal Immobilization Procedure POTENTIAL FOR UNSTABLE SPINAL INJURY? YES > Age > 65 > Meet Trauma Patient Criteria for Mechanism of Injury (Section 3) > Axial load to the head (e.g. diving injury) > Numbness or tingling in extremities If any one of the high-risk factors above are present, strongly consider spinal motion restriction (SMR). A reliable patient is cooperative, sober and alert without: Significant Distracting Injuries Language Barrier YES RELIABLE PATIENT? NORMAL SPINE EXAM? NORMAL MOTOR/SENSORY? OMIT SMR NO Low-risk factors: > Simple rear-end MVC > Ambulatory at any time on scene > No neck pain at scene > Absence of midline cervical spine tenderness The low-risk factors above allow safe omission of SMR. sore development and, in the case of some vacuum device configurations, allow crews to utilize them without a cervical collar.12,29,30 When considering adding vacuum mattresses, vacuum stretchers or other immobilization devices to your arsenal, keep in mind that they don’t require more effort or training than using backboards. Vacuum mattresses can also effectively pad voids, distribute weight evenly and immobilize patients on their side because the device can be “molded” around the patient to best package them safely. (See photos on page 36.) However, keep in mind that backboards 38 JEMS MARCH 2013 POSSIBLE SPINE INJURY APPLY SMR SPINAL PAIN/TENDERNESS Palpate vertebral column thoroughly MOTOR/SENSORY EXAM Wrist or finger extension (both hands) Plantarflexion (both feet) Dorsiflexion (both feet) Check gross sensation in all extremities Check for abnormal sensations to extremities (e.g. parathesias) To obtain a copy of the complete Alameda County Spinal Injury Assessment Procedure, go to the web version of this article at jems.com/journal still have a place, especially to restrain or slide a patient out of an extrication mess. There is also nothing that precludes you from utilizing a combination of devices such as a backboard or scoop-type stretcher to remove a patient and transfer them to a more moldable or comfortable secure surface such as a vacuum mattresses. Many systems use this combination or deploy vacuum mattresses in conjunction with flexible stretchers. (See photo, top of page 36.) Another emerging school of thought questions the need for traditional prehospital spinal immobilization at all—even for patients who have positive evidence of a spinal column or spinal cord injury. One group of researchers who compared various extrication tools and methods found that allowing a patient to self-extricate from a vehicle with a cervical collar alone caused less movement of the spine than the use of cervical collar, KED extrication device and standard extrication techniques.36 This triggers a series of questions that are beyond the scope of this article. Groups such as the National Association of EMS Physicians and the U.S. Metropolitan Municipalities Medical Directors and Global Affiliates Consortium
