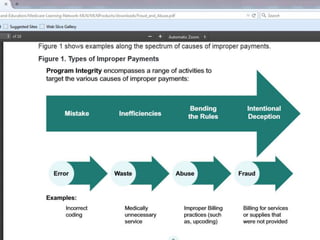
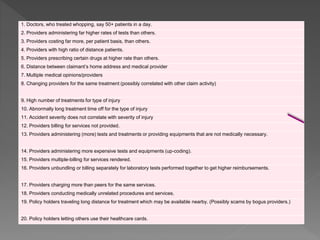
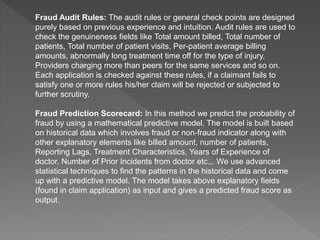
I managed medical malpractice claims and ensured doctors' diagnoses and medical services were justified. I audited claims from an insurance provider using their software, checking doctors' performance and investigating potential fraud like excessive medical services. I monitored medical codes from providers and focused on potential fraud from hospitals, clinics, pharmacies and doctors.