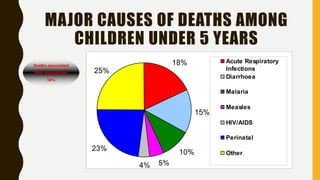
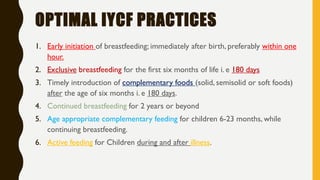
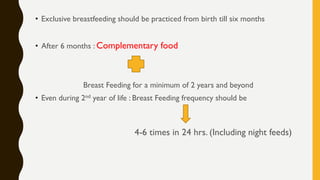
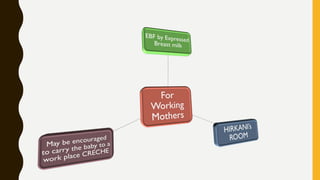
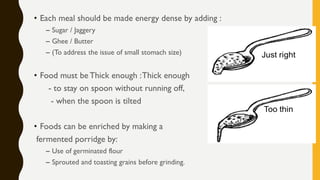
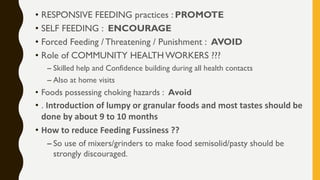
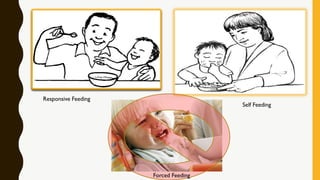
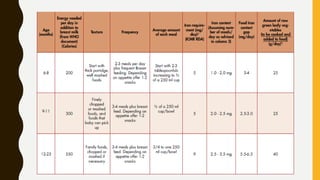
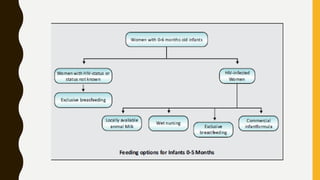
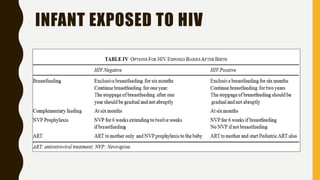
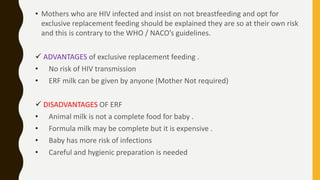
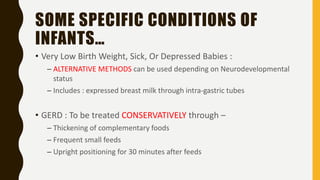
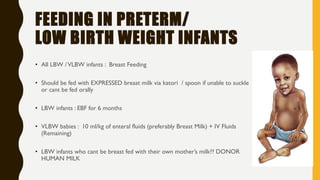
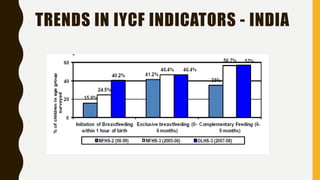
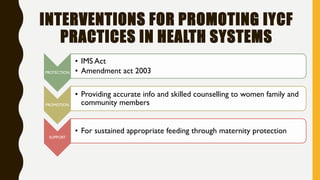
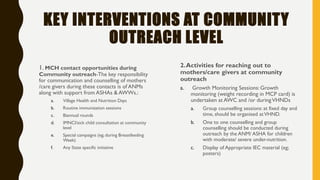
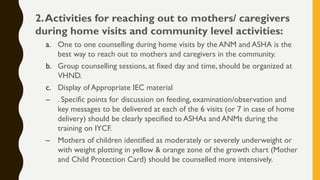
The document provides guidelines for infant and young child feeding (IYCF) developed by WHO and UNICEF, emphasizing the critical importance of appropriate feeding practices for infants and children under two years, who are particularly vulnerable to malnutrition. It outlines key IYCF practices, technical guidelines, and specific feeding recommendations in various conditions, including those for HIV-affected mothers and infants. Furthermore, the document details regulations and interventions aimed at promoting breastfeeding and proper nutrition, along with penalties for violations of the Infant Milk Substitutes Act in India.